Abstract
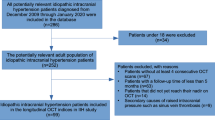
The objectives of the study were to investigate the value of optical coherence tomography in detecting papilledema in patients with idiopathic intracranial hypertension (IIH), a disease which is difficult to monitor and which can lead to permanent visual deficits; to analyze retinal changes over time. In this non-interventional case–control study, spectral-domain optical coherence tomography (SD-OCT) was used to analyze the retinal and optic nerve head (ONH) morphology of 21 patients with IIH and 27 age- and sex-matched healthy controls over time. We analyzed the ONH volume using a custom-made algorithm and employed semi-automated segmentation of macular volume scans to assess the macular retinal nerve fiber layer (RNFL) and ganglion cell layer and inner plexiform layer complex as well as the total macular volume. In IIH patients, the ONH volume was increased and correlated with cerebrospinal fluid (CSF) pressure. The ONH volume decreased after the initiation of treatment with acetazolamide. The macular RNFL volume decreased by 5% in 3.5 months, and a stepwise multivariate regression analysis identified CSF pressure as the main influence on macular RNFL volume at diagnosis. The only factor predicting macular RNFL volume loss over time was ONH volume. SD-OCT can non-invasively monitor changes in retinal and ONH morphology in patients with IIH. Increased ONH volume leads to retinal atrophy in the form of macular RNFL volume loss, presumably due to mechanic jamming of the optic nerve at the disc and subsequent axonal loss.







Similar content being viewed by others
References
Markey KA, Mollan SP, Jensen RH et al (2016) Understanding idiopathic intracranial hypertension: mechanisms, management, and future directions. Lancet Neurol 15:78–91. doi:10.1016/S1474-4422(15)00298-7
Friedman DI, Liu GT, Digre KB (2013) Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 81:1159–1165. doi:10.1212/WNL.0b013e3182a55f17
Mollan SP, Ali F, Hassan-smith G et al (2016) Evolving evidence in adult idiopathic intracranial hypertension : pathophysiology and management. doi:10.1136/jnnp-2015-311302
Olesen J, Bousser G, Diener HC et al (2004) The international classification of headache disorders: 2nd edn. Cephalalgia 24 (Suppl 1):9–160
Wall M, McDermott MP, Kieburtz KD et al (2014) Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA 311:1641–1651. doi:10.1001/jama.2014.3312
Peng K, Fuh J, Wang S (2012) Intracranial hypertension and its mimics. Nat Rev Neurol Gr 8:700–710. doi:10.1038/nrneurol.2012.223
Radhakrishnan K, Ahlskog JE, Cross SA et al (1993) Idiopathic intracranial hypertension (pseudotumor cerebri). Descriptive epidemiology in Rochester, Minn, 1976 to 1990. Arch Neurol 50:78–80. http://www.ncbi.nlm.nih.gov/pubmed/8418804. Accessed 30 Apr 2016
Albrecht P, Blasberg C, Lukas S et al (2015) Retinal pathology in idiopathic moyamoya angiopathy detected by optical coherence tomography. Neurology 85:521–527. doi:10.1212/WNL.0000000000001832
Kaufhold F, Kadas EM, Schmidt C et al (2012) Optic nerve head quantification in idiopathic intracranial hypertension by spectral domain OCT. PLoS One 7:e36965. doi:10.1371/journal.pone.0036965
Hartmann CJ, Klistorner AI, Brandt AU et al (2014) Axonal damage in papilledema linked to idiopathic intracranial hypertension as revealed by multifocal visual evoked potentials. Clin Neurophysiol. doi:10.1016/j.clinph.2014.12.014
Ringelstein M, Albrecht P, Kleffner I et al (2015) Retinal pathology in Susac syndrome detected by spectral-domain optical coherence tomography. Neurology 85:610–618. doi:10.1212/WNL.0000000000001852
Albrecht P, Müller A-K, Südmeyer M et al (2012) Optical coherence tomography in parkinsonian syndromes. PLoS One 7:e34891. doi:10.1371/journal.pone.0034891
Albrecht P, Ringelstein M, Müller A-K et al (2012) Degeneration of retinal layers in multiple sclerosis subtypes quantified by optical coherence tomography. Mult Scler 18:1422–1429. doi:10.1177/1352458512439237
Albrecht P, Müller A-K, Ringelstein M et al (2012) Retinal neurodegeneration in Wilson’s disease revealed by spectral domain optical coherence tomography. PLoS One 7:e49825. doi:10.1371/journal.pone.0049825
Optical T, Tomography C, Committee S (2015) Papilledema outcomes from the optical coherence tomography substudy of the idiopathic intracranial hypertension treatment trial. Ophthalmology. doi:10.1016/j.ophtha.2015.06.003
Kadas EM, Kaufhold F, Schulz C et al (2012) 3D optic nerve segmentation in idiopathic intracranial hypertension. Bildverarbeitung für die Medizin 2012:261–267
Tewarie P, Balk L, Costello F et al (2012) The OSCAR-IB consensus criteria for retinal OCT quality assessment. PLoS One 7:e34823. doi:10.1371/journal.pone.0034823
Cruz-Herranz A, Balk LJ, Oberwahrenbrock T et al (2016) The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology. doi:10.1212/WNL.0000000000002774
Sinclair AJ, Burdon MA, Nightingale PG et al (2010) Low energy diet and intracranial pressure in women with idiopathic intracranial hypertension: prospective cohort study. BMJ 341:c2701. doi:10.1136/bmj.c2701
Bäuerle J, Nedelmann M (2011) Sonographic assessment of the optic nerve sheath in idiopathic intracranial hypertension. J Neurol 258:2014–2019. doi:10.1007/s00415-011-6059-0
Lochner P, Brio F, Zedde ML et al (2016) Feasibility and usefulness of ultrasonography in idiopathic intracranial hypertension or secondary intracranial hypertension. BMC Neurol. doi:10.1186/s12883-016-0594-3
Salgarello T, Tamburrelli C, Falsini B et al (1996) Optic nerve diameters and perimetric thresholds in idiopathic intracranial hypertension. Br J Ophthalmol 80:509–514
Hainline C, Rucker JC, Balcer LJ (2016) Current concepts in pseudotumor cerebri. Curr Opin Neurol 29:84–93. doi:10.1097/WCO.0000000000000273
Batra R, Sinclair A (2014) Idiopathic intracranial hypertension; Research progress and emerging themes. J Neurol 261:451–460. doi:10.1007/s00415-013-7019-7
Raftopoulos R, Hickman SJ, Toosy A et al (2016) Phenytoin for neuroprotection in patients with acute optic neuritis : a randomised, placebo-controlled, phase 2 trial. Lancet Neurol 15:259–269. doi:10.1016/S1474-4422(16)00004-1
Acknowledgements
The authors would like to thank Cheryl Ernest for proofreading.
Author information
Authors and Affiliations
Contributions
PA conceived the study, performed data acquisition and analysis and drafted the manuscript. CB performed data acquisition and analysis, revised the manuscript for intellectual content and created the artwork. MR performed data acquisition and analysis and revised the manuscript for intellectual content. A-KM performed data acquisition and analysis and revised the manuscript. E-MK performed data analysis and revised the manuscript. DF performed data acquisition and revised the manuscript for intellectual content. RG revised the manuscript for intellectual content. OA revised the manuscript for intellectual content and helped with the interpretation of the data. H-PH revised the manuscript for intellectual content and helped with the interpretation of the data. FP revised the manuscript for intellectual content and helped with the interpretation of the data. AB performed data analysis, revised the manuscript for intellectual content and helped with the interpretation of the data. AM drafted and revised the manuscript for intellectual content and interpreted the data.
Corresponding author
Ethics declarations
Funding
The authors received no funding for the study.
Conflicts of interest
Philipp Albrecht received research grants from Novartis, Biogen Idec, Teva, Merz Pharmaceuticals and travel/accommodation/meeting expenses from Novartis, Teva, Biogen Idec, Merz Pharmaceuticals, Ipsen, Esai and GlaxoSmithKline. Christine Blasberg declares no conflicts of interest. Marius Ringelstein received speaker honoraria from Novartis and Bayer Vital GmbH and travel reimbursement from Bayer Schering and Biogen Idec. Ann-Kristin Müller received travel grants from Novartis. Ella-Maria Kadas declares nothing to disclose. David Finis received speaker honoraria and travel grants from Thea-Pharma, TearScience and Oculus. David Finis is now an employee of Bayer Pharma AG, Wuppertal, Germany. Rainer Guthoff received speaker honoraria and travel/accommodation/meeting expenses from Novartis and Bayer Schering. Orhan Aktas received grants from the German Research Foundation (DFG), Eugène Devic European Network (EU-FP7), German Ministry of Education and Research, Schaufler Foundation, honoraria for lectures from Almirall, Novartis, Bayer, Genzyme, Teva, Merck Serono, Biogen, Roche and Medimmune, and received travel/accommodation/meeting expenses from Novartis, Bayer Schering and Merck Serono. Hans-Peter Hartung received grants from the Walter and Ilse Rose Foundation, the Eugène Devic European Network (EU-FP7) and the German Ministry of Education and Research, received honoraria for consultancy from Bayer Health Care, Biogen Idec, Geneuro, Genzyme, Medimmune, Novartis, Opexa, Receptos, Teva, Sanofi Aventis, and Hoffman La Roche and holds patents. Friedemann Paul received research support, travel grants and personal compensation for activities with Bayer, Teva, Sanofi Genzyme, Merck Serono, Biogen and Novartis. He is supported by the German Research Foundation (DFG Exc 257), the Germany Ministry of Education and Research (BMBF Competence Network Multiple Sclerosis), the European Framework Program (EU-FP7, http://www.combims.eu) and the Guthy Jackson Charitable Foundation. Alexander U. Brandt has received consulting fees and speaker honoraria from Novartis, Biogen, Bayer, Teva, Motognosis and Heidelberg Engineering. He is named as co-inventor on a patent application encompassing the optic nerve head volume algorithm. Axel Methner received research and travel grants from Biogen Idec, Novartis and TEVA Pharma.
Ethical standards
The local ethics committee of Heinrich Heine University Düsseldorf approved this prospective observational study. Written informed consent was obtained from all participants in accordance with the Declaration of Helsinki.
Electronic supplementary material
Below is the link to the electronic supplementary material.
415_2017_8532_MOESM1_ESM.tif
Supplemental Figure: Peripapillary Ring Scans in IIH patients. (A/B) Box-and-whisker plots of the mean baseline values for the retinal nerve fiber layer thickness (RNFL) and the total retinal thickness (TRT), measured in peripapillary ring scans centered on the optic disc. The analysis revealed a significant reduction of peripapillary RNFL thickness and TRT in IIH patients compared with healthy controls. (C/D) Box-and-whisker plots of the baseline values and the first follow-up visit (visit 1) as well as p-values for their comparison (GEE analysis) are provided for the peripapillary RNFL and TRT. The investigation only includes those IIH patients who performed a follow-up measurement which was of sufficient quality for analysis: Peripapillary RNFL thickness as well as TRT were significantly reduced in IIH patients at follow-up compared to the baseline. (E/F) Box-and-whisker plots of the mean rates of change per month (Δμm/month) for the different retinal intervals and retinal parameters. Bars in the boxes mark the median, boxes the interquartile range and whiskers minimum and maximum. Numbers of eyes are indicated. P-values for differences for comparison between the IIH patients and healthy controls (A-B), between the baseline and visit 1 (C-D) and between the intervals (E–F) are indicated (bar, GEE analysis) as well as the P-values for differences to zero (E–F, bar, GEE analysis; below the boxes, one-sample t test of left eyes) (TIFF 190 kb)
Rights and permissions
About this article
Cite this article
Albrecht, P., Blasberg, C., Ringelstein, M. et al. Optical coherence tomography for the diagnosis and monitoring of idiopathic intracranial hypertension. J Neurol 264, 1370–1380 (2017). https://doi.org/10.1007/s00415-017-8532-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8532-x