Abstract
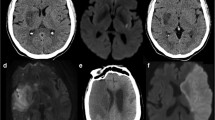
The present study aimed to investigate prospectively the frequency of laminar infarcts (LI) within a standard stroke unit population. Laminar infarcts follow neuroanatomical borders rather than the vascular architecture. The LI are rarely noticed in clinical routine because they are typically not detected by computed tomography. As there is a lack of systemic studies about this specific infarct pattern, little is known about their frequency, clinical characteristics or pathophysiological mechanisms. Consecutive acute ischemic stroke unit patients were prospectively enrolled during a 12 month period. The LI were defined as ischemic lesions following the gyral anatomy of the cerebral cortex. The clinical assessment included a standardized questionnaire, clinical syndromes and standard diagnostic results. There were 491 consecutive ischemic stroke patients enrolled (243 female, mean age 75 ± 12 years). The MRI revealed no laminar lesion crossing vascular territories and 28 patients with LI non-crossing vascular territories (7 %). According to the TOAST classification, 61 % of LI were classified as stroke of undetermined etiology (TOAST V) including 46 % with completed evaluation (TOAST Vb). In contrast to these findings, only 20 % of the whole study cohort with non-laminar infarcts were classified as TOAST V. The results indicate that LI are rare. In clinical routine, patients with LI require particular attention. Within the TOAST classification, this specific infarct pattern seems to be underrepresented.


Similar content being viewed by others
References
Schatlo B, Dreier JP, Glasker S et al (2010) Report of selective cortical infarcts in the primate clot model of vasospasm after subarachnoid hemorrhage. Neurosurgery 67:721–728 discussion 728–729
Weidauer S, Vatter H, Beck J et al (2008) Focal laminar cortical infarcts following aneurysmal subarachnoid haemorrhage. Neuroradiology 50:1–8
Dreier JP, Major S, Manning A et al (2009) Cortical spreading ischaemia is a novel process involved in ischaemic damage in patients with aneurysmal subarachnoid haemorrhage. Brain 132:1866–1881
Stoltenburg-Didinger G (1987) Brain lesions secondary to subarachnoid hemorrhage due to ruptured aneurysms. In: Cervós-Navarro J, Ferszt R (eds) Stroke and microcirculation, vol 42, no 2, p 223
Dreier JP (2011) The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med 17:439–447
Ducros A, Boukobza M, Porcher R, Sarov M, Valade D, Bousser MG (2007) The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome. A prospective series of 67 patients. Brain J Neurol 130:3091–3101
Sibbitt WL Jr, Brooks WM, Kornfeld M, Hart BL, Bankhurst AD, Roldan CA (2010) Magnetic resonance imaging and brain histopathology in neuropsychiatric systemic lupus erythematosus. Semin Arthritis Rheum 40:32–52
Finsterer J (2009) Laminar cortical necrosis in mitochondrial disorders. Clin Neurol Neurosurg 111:655–658
Klingebiel R, Friedman A, Shelef I, Dreier JP (2008) Clearance of a status aurae migraenalis in response to thrombendarterectomy in a patient with high grade internal carotid artery stenosis. J Neurol Neurosurg Psychiatry 79:89–90
Dreier JP, Ebert N, Priller J et al (2000) Products of hemolysis in the subarachnoid space inducing spreading ischemia in the cortex and focal necrosis in rats: a model for delayed ischemic neurological deficits after subarachnoid hemorrhage? J Neurosurg 93:658–666
Dreier JP, Sakowitz OW, Harder A et al (2002) Focal laminar cortical MR signal abnormalities after subarachnoid hemorrhage. Ann Neurol 52:825–829
Neil-Dwyer G, Lang DA, Doshi B, Gerber CJ, Smith PW (1994) Delayed cerebral ischaemia: the pathological substrate. Acta Neurochir (Wien) 131:137–145
Shin HK, Dunn AK, Jones PB, Boas DA, Moskowitz MA, Ayata C (2006) Vasoconstrictive neurovascular coupling during focal ischemic depolarizations. J Cereb Blood Flow Metab 26:1018–1030
Strong AJ, Anderson PJ, Watts HR et al (2007) Peri-infarct depolarizations lead to loss of perfusion in ischaemic gyrencephalic cerebral cortex. Brain 130:995–1008
Tatu L, Moulin T, Bogousslavsky J, Duvernoy H (1996) Arterial territories of human brain: brainstem and cerebellum. Neurology 47:1125–1135
Amarenco P, Goldstein LB, Callahan A 3rd et al (2009) Baseline blood pressure, low- and high-density lipoproteins, and triglycerides and the risk of vascular events in the stroke prevention by aggressive reduction in cholesterol levels (SPARCL) trial. Atherosclerosis 204:515–520
Ferro JM, Oliveira V, Melo TP et al (1991) Role of endarterectomy in the secondary prevention of cerebrovascular accidents: results of the European carotid surgery trial (ECST). Acta Med Port 4:227–228
Amarenco P, Bogousslavsky J, Caplan LR, Donnan GA, Hennerici MG (2009) Classification of stroke subtypes. Cerebrovasc Dis 27:493–501
Amarenco P, Bogousslavsky J, Caplan LR, Donnan GA, Hennerici MG (2009) New approach to stroke subtyping: the A-S-C-O (phenotypic) classification of stroke. Cerebrovasc Dis 27:502–508
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke 24:35–41
Sun-Edelstein C, Bigal ME, Rapoport AM (2009) Chronic migraine and medication overuse headache: clarifying the current International Headache Society classification criteria. Cephalalgia 29:445–452
Hotter B, Pittl S, Ebinger M et al (2009) Prospective study on the mismatch concept in acute stroke patients within the first 24 h after symptom onset—1000Plus study. BMC Neurol 9:60
Ay H, Benner T, Arsava EM et al (2007) A computerized algorithm for etiologic classification of ischemic stroke: the causative classification of stroke system. Stroke 38:2979–2984
Sheerin F, Pretorius PM, Briley D, Meagher T (2008) Differential diagnosis of restricted diffusion confined to the cerebral cortex. Clin Radiol 63:1245–1253
Kastrup O, Maschke M, Wanke I, Diener HC (2002) Posterior reversible encephalopathy syndrome due to severe hypercalcemia. J Neurol 249:1563–1566
Covarrubias DJ, Luetmer PH, Campeau NG (2002) Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol 23:1038–1048
Lauritzen M (1994) Pathophysiology of the migraine aura. The spreading depression theory. Brain 117(Pt 1):199–210
Acknowledgments
The study was conducted in the setting of a government-sponsored stroke research project ‘Kompetenznetz Schlaganfall’ (Bundesministerium für Bildung und Forschung, FK 01GI9903) and in the setting of the Center for Stroke Research Berlin (CSB) (01 EO 0801) and supported by DFG DR 323/5-1.
Conflicts of interest
The authors declare no further conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ziegler, A., Dreier, J.P., Bode, F. et al. Laminar infarcts in clinical routine: a prospective analysis in standard stroke unit patients. J Neurol 260, 2118–2123 (2013). https://doi.org/10.1007/s00415-013-6948-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-013-6948-5