Abstract
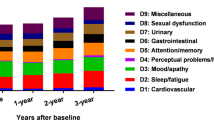
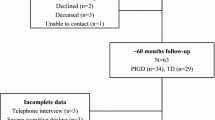
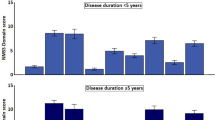
Non-motor symptoms are gaining relevance in Parkinson’s disease (PD) management but little is known about their progression and contribution to deterioration of quality of life. We followed prospectively 707 PD patients (62 % males) for 2 years. We assessed non-motor symptoms referred to 12 different domains, each including 1–10 specific symptoms, as well as motor state (UPDRS), general cognition, and life quality. Hoehn & Yahr (H&Y) stage was used to categorize patient status (I–II mild; III moderate; IV–V severe). We found that individual non-motor symptoms had variable evolution over the 2-year follow-up with sleep, gastrointestinal, attention/memory and skin disturbances (hyperhidrosis and seborrhea) becoming more prevalent and psychiatric, cardiovascular, and respiratory disorders becoming less prevalent. Development of symptoms in the cardiovascular, apathy, urinary, psychiatric, and fatigue domains was associated with significant life-quality worsening (p < 0.0045, alpha with Bonferroni correction). During the observation period, 123 patients (17 %) worsened clinically while 584 were rated as stable. There was a fivefold greater increase in UPDRS motor score in worse compared with stable patients over 24 months (p < 0.0001 vs. baseline both in stable and worse group). The total number of reported non-motor symptoms increased over 24 months in patients with motor worsening compared to stable ones (p < 0.001). Thirty-nine patients died (3.4 % of patients evaluable at baseline) with mean age at death of 74 years. Deceased patients were older, had significantly higher H&Y stage and motor score, and reported a greater number of non-motor symptoms at baseline. In conclusion, overall non-motor symptom progression does not follow motor deterioration, is symptom-specific, and only development of specific domains negatively impacts quality of life. These results have consequences for drug studies targeting non-motor features.




Similar content being viewed by others
References
Chaudhuri KR, Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P et al (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord 21:916–923
Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, Macphee G et al (2007) Prevalence of nonmotor symptoms in Parkinson’s disease in an international setting; study using nonmotor symptoms questionnaire in 545 patients. Mov Disord 22:1623–1629
Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP, Bottacchi E et al (2009) The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord 24:1641–1649
Chaudhuri KR, Martinez-Martin P, Brown RG, Sethi K, Stocchi F, Odin P et al (2007) The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov Disord 22:1901–1911
Simuni T, Sethi K (2008) Non-motor manifestations of Parkinson’s disease. Ann Neurol 64(Suppl 2):S65–S80
Beiske AG, Loge JH, Rønningen A, Svensson E (2009) Pain in Parkinson’s disease: prevalence and characteristics. Pain 141:173–177
Honig H, Antonini A, Martinez-Martin P, Forgacs I, Faye GC, Fox T et al (2009) Intrajejunal levodopa infusion in Parkinson’s disease: a pilot multicenter study of effects on nonmotor symptoms and quality of life. Mov Disord 24:1468–1474
Barone P, Poewe W, Albrecht S et al (2010) Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 9:573–580
Hely MA, Morris JG, Reid WG, Trafficante R (2005) Sydney Multicenter Study of Parkinson’s disease: non-L-dopa responsive problems dominate at 15 years. Mov Disord 20:190–199
Buter TC, van den Hout A, Matthews FE, Larsen JP, Brayne C, Aarsland D (2008) Dementia and survival in Parkinson disease: a 12-year population study. Neurology 70:1017–1022
Chaudhuri KR, Schapira AH (2009) Non-motor symptoms of Parkinson’s disease: dopaminergic pathophysiology and treatment. Lancet Neurol 8(5):464–474
Antonini A, Colosimo C, Marconi R, Morgante L, Barone P (2008) The PRIAMO Study: background, methods and recruitment. Neurol Sci 29:61–65
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Fahn S, Elton R, Members of the UPDRS Development Committee (1987) The unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M (eds) Recent developments in Parkinson’s disease, vol 2. Macmillan Health Care Information, Florham Park, pp 153–63, 293–304
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Dubois B, Slachevsky A, Litvan I, Pillon B (2000) The FAB: a Frontal Assessment Battery at bedside. Neurology 55:1621–1626
Peto V, Jenkinson C, Fitzpatrick R, Greenhall R (1995) The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual Life Res 4:241–248
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
McDowell I, Newell C (1996) Measuring health: a guide to rating scales and questionnaires. Oxford University Press, New York
Measso GF, Cavarzeran F, Zappalà G, Lebowitz BD, Pirozzolo FJ, Amaducci LA et al (1993) The Mini-Mental State Examination: normative study of a random sample of Italian population. Dev Neuropsychol 9:77–85
Appollonio I, Leone M, Isella V, Piamarta F, Consoli T, Villa ML et al (2005) The Frontal Assessment Battery (FAB): normative values in an Italian population sample. Neurol Sci 26:108–116
Istituto Nazionale di Statistica (2008) Tavole di mortalità della popolazione residente
Poewe W, Mahlknecht P (2009) The clinical progression of Parkinson’s disease. Parkinsonism Relat Disord 15:S28–S32
Schrag A, Dodel R, Spottke A, Bornschein B, Siebert U, Quinn NP (2007) Rate of clinical progression in Parkinson’s disease. A prospective study. Mov Disord 22:938–945
Maetzler W, Liepelt I, Liepelt I, Berg D (2009) Progression of Parkinson’s disease in the clinical phase: potential markers. Lancet Neurol 8:1158–1171
Chaudhuri KR, Prieto-Jurcynska C, Naidu Y, Mitra T, Frades-Payo B, Tluk S et al (2010) The non-declaration of nonmotor symptoms of Parkinson’s disease to health care professionals: an international study using the nonmotor symptoms questionnaire. Mov Disord 25:697–701
Trenkwalder C, Kies B, Rudzinska M et al (2011) Rotigotine effects on early morning motor function and sleep in Parkinson’s disease: a double-blind, randomized, placebo-controlled study (RECOVER). Mov Disord 26(1):90–99
Hoops S, Nazem S, Siderowf AD et al (2009) Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology 73(21):1738–1745
Conflicts of interest
A. Antonini has received honoraria for consulting services and symposia from Abbott, Boehringer Ingelheim, GSK, Lundbeck, UCB, Novartis and Merck Serono; P. Barone has received honoraria for consulting services and symposia from Boehringer Ingelheim; R. Marconi has received honoraria for consulting services and symposia from Boehringer Ingelheim; L. Morgante has received honoraria for consulting services and symposia from Boehringer Ingelheim; C. Colosimo has received honoraria for consulting services and symposia from Boehringer Ingelheim; and all other authors have nothing to disclose.
Ethical standards
The study was approved by the Ethic Committee of each individual institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the PRIAMO study group.
The members of the PRIAMO study group are given in Appendix 1.
Appendices
Appendix 1: The PRIAMO study group
First name | Last name | Unit | Hospital | Town |
|---|---|---|---|---|
Salvatore | Zappulla | Neurologia | Ospedale Umberto I | Enna |
Clelia | Pellicano | Clinica Neurologica | Ospedale Sant’Andrea, II Facoltà di Medicina e Chirurgia, “Sapienza” Università di Roma | Roma |
Sara | Meoni | Clinica Neurologica I | Day Hospital Dip. Scienze Neurologiche e Psichiatriche | Firenze |
Marianna | Capecci | Clinica di Neuroriabilitazione | Ospedale Umberto I | Ancona |
Natalia | Caravona | Centro Parkinson Dipartimento di Neurologia e Psichiatria e Centro di Ricerca per le Malattie Sociali (CIMS) | “Sapienza” Università di Roma | Roma |
Gianni | Pezzoli | Centro Parkinson | Istituti Clinici di Perfezionamento | Milano |
Vittorio | Petretta | Neurologia e Stroke | A.O.R.N. San Giuseppe Moscati | Avellino |
Massimo | Pederzoli | Neurologia | Ospedale Civile | Vimercate |
Fulvio | Pepe | Neurologia | Fondazione Poliambulanza | Brescia |
Marianna | Amboni | IDC-Hermitage-Capodimonte | Napoli | |
Daniela | Frosini | Centro Parkinson | Azienda Ospedaliero-Universitaria Pisana | Pisa |
Sergio | Zanini | Clinica Neurologica | Policlinico Universitario Udine | Udine |
Giampiero | Volpe | Neurofisiopatologia Dip. Neuro Orto Traumatologia | Presidio Ospedaliero S. Luca | Vallo della Lucania |
Gilda | Di Brigida | Dipartimento Neuroscienze, Oftalmologia e Genetica | Università degli Studi di Genova | Genova |
Marco | Di Giovanni | U.O. di Neurologia | Ospedale Regionale | Aosta |
Roberto | L’Erario | Neurologia | Ospedale Civile San Bortolo | Vicenza |
Giuseppe | Ciacci | Neurologia | Policlinico Le Scotte | Siena |
Antonio | Cannas | U.O.Neurologia | Policlinico Universitario di Monserrato | Monserrato, Cagliari |
Luisa | Giglia | Neurologia | Azienda Ospedaliera S. Elia | Caltanissetta |
Alfredo | Petrone | Neurologia | Presidio Ospedaliero Annunziata | Cosenza |
Stefano | Amidei | Neurologia | Ospedale Ramazzini | Carpi |
Giorgio | Trianni | Neurologia | P.O. F. Ferrari | Casarano |
Giovanni | Cossu | Centro Parkinson -U.O.Neurologia | Azienda Ospedaliera G.BROTZU | Cagliari |
Maria | Bloise | Dip.to Scienze Neurologiche | Policlinico Umberto I Univ.La Sapienza | Roma |
Chiara | Logi | U.O Neurologia | Ospedale Versilia | Camajore |
Francesco | Soleti | Clinica Neurologica | Università Cattolica S. Cuore Policlinico Gemelli | Roma |
Michele | Abrignani | U.O. Neurologia | Ospedale di Marsala ASP TP/2 | Marsala |
Rossana | Scala | Neurologia | Ospedale S. Maria Loreto Nuovo | Napoli |
Franco | Pennisi | Neurologia | Ospedale di Castelvetrano | Castelvetrano |
Lucia | Grasso | Neurologia | Ospedale della Misericordia | Grosseto |
Francesca | Preda | Neurologia Dip. Neuroscienze applicate alla clinica | Ospedale Sant’Anna | Ferrara |
Giacomo | Gurgone | U.O. Neurologia | Az. Osp. S.Giovanni di Dio | Agrigento |
Mario | Zappia | Clinica Neurologica I | Policlinico Universitario | Catania |
Stefania | Lanfranchi | Neurologia | Ospedale S. Antonio Abate Gallarate | Gallarate |
Tania | Avarello | Centro per lo studio delle M.Extrapiramidali | O.R. Villa Sofia | Palermo |
Francesca | Morgante | Dipartimento di Neuroscienze, Scienze psichiatriche ed Anestesiologiche | Università di Messina | Messina |
Paolo | Stanzione | Dept. Neuroscience | Università di Roma Tor Vergata | Roma |
Augusto | Scaglioni | Div. Neurologia | Ospedale di Vaio | Fidenza |
Sabina | Capellari | Centro per lo studio e la cura delle malattie extrapiramidali | Dipartimento Scienze Neurologiche Università di Bologna | Bologna |
Monia | Blundo | U.O. Neurologia | P.O. Guzzardi | Vittoria |
Lucia | Antonutti | Clinica Neurologica | Ospedale di Cattinara | Trieste |
Pasqualino | Simone | Neurologia | Ospedale Casa Sollievo della Sofferenza | San Giovanni Rotondo |
Paola | Soliveri | Neurologia I | Istituto Nazionale Neurologico C. Besta | Milano |
Biagio | Troianello | Neurologia | Istituto Clinico Città di Brescia | Brescia |
Mattia Anna | Iellamo | U.O. Neurologia | Ospedale G. Iazzolino | Vibo Valentia |
Alessandro | Mauro | Neurologia | Istituto Scientifico San Giuseppe | Piancavallo |
Maurizio | Zibetti | Dipartimento Neuroscienze | Università degli Studi di Torino | Torino |
Giuseppe | Nastasi | Neurologia | Az. Osp. Papardo | Messina |
Appendix 2
Steering committee
- Angelo Antonini:
-
Department for Parkinson’s disease IRCCS San Camillo, Venezia
- Paolo Barone:
-
Scuola Medica Salernitana, Università di Salerno, Salerno; IDC-Hermitage-Capodimonte, Napoli
- Carlo Colosimo:
-
Università La Sapienza, Roma
- Roberto Marconi:
-
Ospedale della Misericordia, Grosseto
- Letterio Morgante:
-
Dipartimento di Neuroscienze, Scienze Psichiatriche ed Anestesiologiche, Università di Messina, Italy.
Sponsorship
-
Tania Corbetta, Arina Dumitriu, Boehringer Ingelheim, Milan, Italy.
Project management, statistical analyses, and data management
-
Simona Sgarbi, project leader MediData Studi e Ricerche, Modena
-
Andrea Rapisarda, clinical project manager MediData Studi e Ricerche, Modena
-
Sara Rizzoli, Lucia Simoni, statisticians MediData Studi e Ricerche, Modena
-
Luca Zanoli, clinical data manager MediData Studi e Ricerche, Modena
-
Alessandra Manfredi, clinical operation specialist MediData Studi e Ricerche, Modena, Italy.
Rights and permissions
About this article
Cite this article
Antonini, A., Barone, P., Marconi, R. et al. The progression of non-motor symptoms in Parkinson’s disease and their contribution to motor disability and quality of life. J Neurol 259, 2621–2631 (2012). https://doi.org/10.1007/s00415-012-6557-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-012-6557-8