Abstract
Purpose
Postoperative pneumonia remains a common complication of surgery, despite increased attention. The purpose of our study was to determine the effects of routine surgery and post-surgical opioid administration on airway protection risk.
Methods
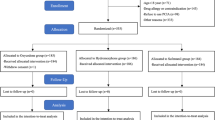
Eight healthy adult cats were evaluated to determine changes in airway protection status and for evidence of dysphagia in two experiments. (1) In four female cats, airway protection status was tracked following routine abdominal surgery (spay surgery) plus low-dose opioid administration (buprenorphine 0.015 mg/kg, IM, q8-12 h; n = 5). (2) Using a cross-over design, four naive cats (2 male, 2 female) were treated with moderate-dose (0.02 mg/kg) or high-dose (0.04 mg/kg) buprenorphine (IM, q8-12 h; n = 5).
Results
Airway protection was significantly affected in both experiments, but the most severe deficits occurred post-surgically as 75% of the animals exhibited silent aspiration.
Conclusion
Oropharyngeal swallow is impaired by the partial mu-opioid receptor agonist buprenorphine, most remarkably in the postoperative setting. These findings have implications for the prevention and management of aspiration pneumonia in vulnerable populations.


Similar content being viewed by others
References
Haller L et al (2022) Post-operative dysphagia in anterior cervical discectomy and fusion. Ann Otol Rhinol Laryngol 131(3):289–294
Goeze A et al (2022) Post-operative prevalence of dysphagia in head-and-neck cancer patients in the acute care units. Laryngorhinootologie 101(4):320–326
Greenberg JA et al (2022) Evaluation of post-operative dysphagia following anti-reflux surgery. Surg Endosc 36(7):5456–5466
Hayes M et al (2022) Prevalence, nature and trajectory of dysphagia postoesophageal cancer surgery: a prospective longitudinal study protocol. BMJ Open 12(9):e058815
Nath A et al (2016) Dysphagia after vertical sleeve gastrectomy: Evaluation of risk factors and assessment of endoscopic intervention. World J Gastroenterol 22(47):10371–10379
Skoretz SA et al (2020) A systematic review of tracheostomy modifications and swallowing in adults. Dysphagia 35(6):935–947
Garibaldi RA et al (1981) Risk factors for postoperative pneumonia. Am J Med 70(3):677–680
Arozullah AM et al (2001) Development and validation of a multifactorial risk index for predicting postoperative pneumonia after major noncardiac surgery. Ann Intern Med 135(10):847–857
Kozlow JH et al (2003) Epidemiology and impact of aspiration pneumonia in patients undergoing surgery in Maryland, 1999–2000. Crit Care Med 31(7):1930–1937
Chughtai M et al (2017) The epidemiology and risk factors for postoperative pneumonia. J Clin Med Res 9(6):466–475
Chughtai M et al (2017) The incidence of postoperative pneumonia in various surgical subspecialties: a dual database analysis. Surg Technol Int 30:45–51
Steffens C et al (2020) The association between prescribed opioid receipt and community-acquired pneumonia in adults: a systematic review and meta-analysis. J Gen Intern Med 35(11):3315–3322
Almirall J et al (2013) Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J 41(4):923–928
Jean A (2001) Brain stem control of swallowing: neuronal network and cellular mechanisms. Physiol Rev 81(2):929–969
Pitts T, Iceman KE (2023) Deglutition and the regulation of the swallow motor pattern. Physiology 38(1):10–24
Gupte T, Knack A, Cramer JD (2022) Mortality from aspiration pneumonia: incidence, trends, and risk factors. Dysphagia 37(6):1493–1500
Bateman JT, Saunders SE, Levitt ES (2023) Understanding and countering opioid-induced respiratory depression. Br J Pharmacol 180(7):813–828
Roughan JV, Flecknell PA (2002) Buprenorphine: a reappraisal of its antinociceptive effects and therapeutic use in alleviating post-operative pain in animals. Lab Anim 36(3):322–343
Koehl JL, Zimmerman DE, Bridgeman PJ (2019) Medications for management of opioid use disorder. Am J Health Syst Pharm 76(15):1097–1103
Foley KM (1993) Opioids. Neurol Clin 11(3):503–522
Roy S et al (2011) Opioid drug abuse and modulation of immune function: consequences in the susceptibility to opportunistic infections. J Neuroimmune Pharmacol 6(4):442–465
Patel D, Vaezi M (2018) Opioid-induced esophageal dysfunction: an emerging entity with sweeping consequences. Curr Treat Options Gastroenterol 16(4):616–621
Patel DA et al (2022) Opioid exposure differentially impacts esophageal body contraction over the lower esophageal sphincter. Gastroenterology 163(2):403–410
Savilampi J et al (2014) Aspiration induced by remifentanil: a double-blind, randomized, crossover study in healthy volunteers. Anesthesiology 121(1):52–58
Tagaito Y, Isono S, Nishino T (1998) Upper airway reflexes during a combination of propofol and fentanyl anesthesia. Anesthesiology 88(6):1459–1466
Olfson M et al (2020) Trends in buprenorphine treatment in the United States, 2009–2018. JAMA 323(3):276–277
Shulman M, Wai JM, Nunes EV (2019) Buprenorphine treatment for opioid use disorder: an overview. CNS Drugs 33(6):567–580
Elkader A, Sproule B (2005) Buprenorphine: clinical pharmacokinetics in the treatment of opioid dependence. Clin Pharmacokinet 44(7):661–680
Davis MP, Pasternak G, Behm B (2018) Treating chronic pain: an overview of clinical studies centered on the buprenorphine option. Drugs 78(12):1211–1228
Robinson SE (2002) Buprenorphine: an analgesic with an expanding role in the treatment of opioid addiction. CNS Drug Rev 8(4):377–390
Zhuang J et al (2017) Mu-opioid receptors in the caudomedial NTS are critical for respiratory responses to stimulation of bronchopulmonary C-fibers and carotid body in conscious rats. Respir Physiol Neurobiol 235:71–78
Maletz SN et al (2022) Nucleus tractus solitarius neurons activated by hypercapnia and hypoxia lack Mu opioid receptor expression. Front Mol Neurosci 15:932189
Hardemark Cedborg AI et al (2015) Effects of morphine and midazolam on pharyngeal function, airway protection, and coordination of breathing and swallowing in healthy adults. Anesthesiology 122(6):1253–1267
Frazure M et al (2024) Serotonin therapies for opioid-induced disordered swallow and respiratory depression. J Appl Physiol (1985). https://doi.org/10.1152/japplphysiol.00509.2023
Steagall P, Monteiro-Steagall B, Taylor P (2014) A review of the studies using buprenorphine in cats. J Vet Intern Med 28(3):762–770
Steagall PV et al (2009) Dose-related antinociceptive effects of intravenous buprenorphine in cats. Vet J 182(2):203–209
Plumb DC (2005) Plumb’s veterinary drug handbook. 2005: Fifth edition. Stockholm, Wis. : PhrmaVet ; Ames, Iowa : Distributed by Blackwell Pub
Holman SD et al (2013) Development, reliability, and validation of an infant mammalian penetration-aspiration scale. Dysphagia 28(2):178–187
Rosenbek JC et al (1996) A penetration-aspiration scale. Dysphagia 11(2):93–98
Martin-Harris B et al (2008) MBS measurement tool for swallow impairment–MBSImp: establishing a standard. Dysphagia 23(4):392–405
Tang W et al (2015) Kappa coefficient: a popular measure of rater agreement. Shanghai Arch Psychiatry 27(1):62–67
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428
Gharavi R et al (2015) Transporter-mediated disposition of opioids: implications for clinical drug interactions. Pharm Res 32(8):2477–2502
Waldhoer M, Bartlett SE, Whistler JL (2004) Opioid receptors. Annu Rev Biochem 73:953–990
Williams JT et al (2013) Regulation of mu-opioid receptors: desensitization, phosphorylation, internalization, and tolerance. Pharmacol Rev 65(1):223–254
Pasternak GW, Pan YX (2013) Mu opioids and their receptors: evolution of a concept. Pharmacol Rev 65(4):1257–1317
Pitts T, Iceman KE (2023) Deglutition and the regulation of the swallow motor pattern. Physiology (Bethesda) 38(1):10
Ramirez JM et al (2021) Neuronal mechanisms underlying opioid-induced respiratory depression: our current understanding. J Neurophysiol 125(5):1899–1919
Bolser DC, DeGennaro FC (1994) Effect of codeine on the inspiratory and expiratory burst pattern during fictive cough in cats. Brain Res 662(1–2):25–30
Lang IM, Marvig J (1989) Functional localization of specific receptors mediating gastrointestinal motor correlates of vomiting. Am J Physiol 256(1 Pt 1):G92–G99
Blivis D et al (2007) Differential effects of opioids on sacrocaudal afferent pathways and central pattern generators in the neonatal rat spinal cord. J Neurophysiol 97(4):2875–2886
Irnaten M et al (2003) Mu-opioid receptors are located postsynaptically and endomorphin-1 inhibits voltage-gated calcium currents in premotor cardiac parasympathetic neurons in the rat nucleus ambiguus. Neuroscience 116(2):573–582
Rommel N, Hamdy S (2016) Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol 13(1):49–59
Logemann JA (2007) Swallowing disorders. Best Pract Res Clin Gastroenterol 21(4):563–573
Logemann JA (1997) Role of the modified barium swallow in management of patients with dysphagia. Otolaryngol Head Neck Surg 116(3):335–338
Donner MW (1985) Radiologic evaluation of swallowing. Am Rev Respir Dis 131(5):S20–S23
German RZ et al (2017) Animal models for dysphagia studies: what have we learnt so far. Dysphagia 32(1):73–77
Lever TE et al (2015) Videofluoroscopic validation of a translational murine model of presbyphagia. Dysphagia 30(3):328–342
Harris RA et al (2017) Standardization of a videofluoroscopic swallow study protocol to investigate dysphagia in dogs. J Vet Intern Med 31(2):383–393
Stevens M et al (2021) Pathophysiology of aspiration in a unilateral SLN lesion model using quantitative analysis of VFSS. Int J Pediatr Otorhinolaryngol 140:110518
Cullins MJ, Connor NP (2019) Reduced tongue force and functional swallowing changes in a rat model of post stroke dysphagia. Brain Res 1717:160–166
Kobara-Mates M et al (1995) Physiology of oropharyngeal swallow in the cat: a videofluoroscopic and electromyographic study. Am J Physiol 268(2 Pt 1):G232–G241
Sampson S, Eyzaguirre C (1964) Some functional characteristics of mechanoreceptors in the larynx of the cat. J Neurophysiol 27:464–480
Pitts T et al (2013) Coordination of cough and swallow: a meta-behavioral response to aspiration. Respir Physiol Neurobiol 189(3):543–551
Karlsson JA, Lanner AS, Persson CG (1990) Airway opioid receptors mediate inhibition of cough and reflex bronchoconstriction in guinea pigs. J Pharmacol Exp Ther 252(2):863–868
Kamei J (1996) Role of opioidergic and serotonergic mechanisms in cough and antitussives. Pulm Pharmacol 9(5–6):349–356
Kamei J et al (1989) Subsensitivity to the cough-depressant effects of opioid and nonopioid antitussives in morphine-dependent rats: relationship to central serotonin function. Pharmacol Biochem Behav 34(3):595–598
Babaei A et al (2019) Chronic daily opioid exposure is associated with dysphagia, esophageal outflow obstruction, and disordered peristalsis. Neurogastroenterol Motil 31(7):e13601
Finnerty CC et al (2013) The surgically induced stress response. JPEN J Parenter Enteral Nutr 37(5 Suppl):21S-S29
Priebe HJ (2016) Pharmacological modification of the perioperative stress response in noncardiac surgery. Best Pract Res Clin Anaesthesiol 30(2):171–189
Kohl BA, Deutschman CS (2006) The inflammatory response to surgery and trauma. Curr Opin Crit Care 12(4):325–332
Iscoe S (1998) Control of abdominal muscles. Prog Neurobiol 56(4):433–506
Depauw P et al (2019) The significance of intra-abdominal pressure in neurosurgery and neurological diseases: a narrative review and a conceptual proposal. Acta Neurochir (Wien) 161(5):855–864
Pitts T et al (2022) Laryngeal and swallow dysregulation following acute cervical spinal cord injury. J Neurophysiol 128(2):405–417
Pitts T et al (2015) Effect of laparotomy on the swallow-breathing relationship in the cat. Lung 193(1):129–133
Sanchez MJ et al (2022) Chronic opioid use is associated with obstructive and spastic disorders in the esophagus. Neurogastroenterol Motil 34(3):e14233
Snyder DL, Vela MF (2020) Opioid-induced esophageal dysfunction. Curr Opin Gastroenterol 36(4):344–350
Patel D, Callaway J, Vaezi M (2019) Opioid-induced foregut dysfunction. Am J Gastroenterol 114(11):1716–1725
Hiss SG, Treole K, Stuart A (2001) Effects of age, gender, bolus volume, and trial on swallowing apnea duration and swallow/respiratory phase relationships of normal adults. Dysphagia 16(2):128–135
Riley LH 3rd et al (2005) Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine 30(22):2564–9
Bollschweiler E et al (2008) Prevalence of dysphagia in patients with gastroesophageal reflux in Germany. Dysphagia 23(2):172–176
Mori T et al (2022) Association between inflammation and functional outcome in patients with sarcopenic dysphagia. J Nutr Health Aging 26(4):400–406
Huff A et al (2020) Sex-specific vagal and spinal modulation of swallow and its coordination with breathing. PLoS ONE 15(6):e0234194
Fishman MA, Kim PS (2018) Buprenorphine for chronic pain: a systemic review. Curr Pain Headache Rep 22(12):83
Funding
Research reported in this publication was supported by NIH Grants NS110169, HL155721, HL163008, HD110951, NS097781, OT20D001983, the Craig H. Neilsen Foundation Pilot Research Grant 546714, Kentucky Spinal Cord and Head Injury Research Trust, Rebecca Hammond Endowment and the Commonwealth of Kentucky Challenge for Excellence. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to conception and design of the study. MF, CLG and TP collected data. MF, KEI and TP analyzed data and prepared figures. MF, KEI and TP wrote the initial draft. All authors edited, revised and reviewed the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest, financial or otherwise, are declared by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file 2 (M4V 13074 kb)
Supplementary file 3 (M4V 22300 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Frazure, M., Greene, C.L., Iceman, K.E. et al. Dysphagia as a Missing Link Between Post-surgical- and Opioid-Related Pneumonia. Lung 202, 179–187 (2024). https://doi.org/10.1007/s00408-024-00672-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-024-00672-8