Abstract
Introduction
Reported associations between World Trade Center (WTC) occupational exposure and chronic obstructive pulmonary disease (COPD) or asthma COPD overlap (ACO) have been inconsistent. Using spirometric case definitions, we examined that association in the largest WTC occupational surveillance cohort.
Methods
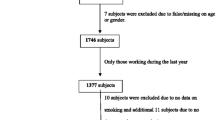
We examined the relation between early arrival at the 2001 WTC disaster site (when dust and fumes exposures were most intense) and COPD and ACO in workers with at least one good quality spirometry with bronchodilator response testing between 2002 and 2019, and no physician-diagnosed COPD before 9/11/2001. COPD was defined spirometrically as fixed airflow obstruction and ACO as airflow obstruction plus an increase of ≥ 400 ml in FEV1 after bronchodilator administration. We used a nested 1:4 case-control design matching on age, sex and height using incidence density sampling.
Results
Of the 17,928 study participants, most were male (85.3%) and overweight or obese (84.9%). Further, 504 (2.8%) and 244 (1.4%) study participants met the COPD and ACO spirometric case definitions, respectively. In multivariable analyses adjusted for smoking, occupation, cohort entry period, high peripheral blood eosinophil count and other covariates, early arrival at the WTC site was associated with both COPD (adjusted odds ratio [ORadj] = 1.34, 95% confidence interval [CI] 1.01–1.78) and ACO (ORadj = 1.55, 95%CI 1.04–2.32).
Conclusion
In this cohort of WTC workers, WTC exposure intensity was associated with spirometrically defined COPD and ACO. Our findings suggest that early arrival to the WTC site is a risk factor for the development of COPD or of fixed airway obstruction in workers with pre-existing asthma.
Similar content being viewed by others
References
de la Hoz RE, Shohet MR, Chasan R, Bienenfeld LA, Afilaka AA, Levin SM, Herbert R (2008) Occupational toxicant inhalation injury: the World Trade Center (WTC) experience. Int Arch Occup Environ Health 81(4):479–485. https://doi.org/10.1007/s00420-007-0240-x
de la Hoz RE (2011) Occupational lower airway disease in relation to World Trade Center inhalation exposure. Curr Opin Allergy Clin Immunol 11(2):97–102. https://doi.org/10.1097/ACI.0b013e3283449063
Prezant DJ, Weiden M, Banauch GI, McGuinness G, Rom WN, Aldrich TK, Kelly KJ (2002) Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med 347(11):806–815. https://doi.org/10.1056/NEJMoa021300
Herbert R, Moline J, Skloot G, Metzger K, Barron S, Luft B, Markowitz S, Udasin I, Harrison D, Stein D, Todd AC, Enright P, Stellman JM, Landrigan PJ, Levin SM (2006) The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect 114(12):1853–1858. https://doi.org/10.1289/ehp.9592
Wisnivesky JP, Teitelbaum S, Todd AC, Boffeta P, Crane M, Crowley L, de la Hoz RE, Dellenbaugh C, Harrison D, Herbert R, Kim H, Jeon Y, Kaplan J, Katz C, Levin S, Luft B, Markowitz S, Moline JM, Ozbay F, Pietrzak RH, Shapiro M, Sharma V, Skloot G, Southwick S, Stevenson L, Udasin I, Wallenstein S, Landrigan PJ (2011) Persistence of multiple illnesses in September 11 rescue workers. Lancet 378(9794):888–897. https://doi.org/10.1016/S0140-6736(11)61180-X
de la Hoz RE, Weber J, Xu D, Doucette JT, Liu X, Carson DA, Celedón JC (2019) Chest CT scan findings in World Trade Center workers. Arch Environ Occup Health 74(5):263–270. https://doi.org/10.1080/19338244.2018.1452712
de la Hoz RE, Liu X, Doucette JT, Reeves AP, Bienenfeld LA, Wisnivesky JP, Celedón JC, Lynch DA, San José Estépar R (2018) Increased airway wall thickness is associated with adverse longitudinal first-second forced expiratory volume trajectories of former World Trade Center workers. Lung 196(4):481–489. https://doi.org/10.1007/s00408-018-0125-7
de la Hoz RE, Shapiro M, Nolan A, Celedón JC, Szeinuk J, Lucchini RG (2020) Association of low FVC spirometric pattern with WTC occupational exposures. Respir Med 170:106058. https://doi.org/10.1016/j.rmed.2020.106058
Liu X, Reeves AP, Antoniak K, San José Estépar R, Doucette JT, Jeon Y, Weber J, Xu D, Celedón JC, de la Hoz RE (2021) Association of quantitative CT lung density measurements with divergent FEV1 trajectories in WTC workers. Clin Respir J 15(6):613–621. https://doi.org/10.1111/crj.13313
Haghighi A, Cone JE, Li J, de la Hoz RE (2021) Asthma-COPD overlap in World Trade Center Health Registry enrollees, 2015–2016. J Asthma 58(11):1415–1423. https://doi.org/10.1080/02770903.2020.1817935
Singh A, Liu C, Putman B, Zeig-Owens R, Hall CB, Schwartz T, Webber MP, Cohen HW, Berger KI, Nolan A, Prezant DJ, Weiden MD (2018) Predictors of asthma/COPD overlap in FDNY firefighters with World Trade Center dust exposure: a longitudinal study. Chest 154(6):1301–1310. https://doi.org/10.1016/j.chest.2018.07.002
Woskie SR, Kim H, Freund A, Stevenson L, Park BY, Baron S, Herbert R, Siegel de Hernandez M, Teitelbaum S, de la Hoz RE, Wisnivesky JP, Landrigan P (2011) World Trade Center disaster: assessment of responder occupations, work locations, and job tasks. Am J Ind Med 54(9):681–695. https://doi.org/10.1002/ajim.20997
de la Hoz RE (2010) Occupational asthma and lower airway disease in former World Trade Center workers and volunteers. Curr Allergy Asthma Rep 10(4):287–294. https://doi.org/10.1007/s11882-010-0120-4
de la Hoz RE, Shohet MR, Cohen JM (2010) Occupational rhinosinusitis and upper airway disease: the World Trade Center experience. Curr Allergy Asthma Rep 10(2):77–83. https://doi.org/10.1007/s11882-010-0088-0
de la Hoz RE, Christie J, Teamer J, Bienenfeld LA, Afilaka AA, Crane M, Levin SM, Herbert R (2008) Reflux symptoms and disorders and pulmonary disease in former World Trade Center rescue and recovery workers and volunteers. J Occup Environ Med 50 (12):1351-1354. https://doi.org/10.1097/JOM.0b013e3181845f9b
de la Hoz RE, Johannson KA (2023) World Trade Center Health Program best practices for the diagnosis and treatment of fibrosing interstitial lung diseases. Arch Environ Occup Health 78(4):232–235. https://doi.org/10.1080/19338244.2023.2166007
Cone JE, de la Hoz RE (2023) World Trade Center Health Program best practices for diagnosing and treating chronic obstructive pulmonary disease. Arch Environ Occup Health 78(4):229–231. https://doi.org/10.1080/19338244.2022.2146040
Hankinson JL, Odencratz JR, Fedan KB (1999) Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med 159(1):179–187. https://doi.org/10.1164/ajrccm.159.1.9712108
American Thoracic Society (1995) Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 152(3):1107–1136. https://doi.org/10.1164/ajrccm.152.3.7663792
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CPM, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338. https://doi.org/10.1183/09031936.05.00034805
Enright PL, Skloot GS, Cox-Ganser JM, Udasin IG, Herbert R (2010) Quality of spirometry performed by 13,599 participants in the World Trade Center Worker and Volunteer Medical Screening Program. Respir Care 55(3):303–309. https://rc.rcjournal.com/content/55/3/303.short
Wallingford KM, Snyder EM (2001) Occupational exposures during the World Trade Center disaster response. Toxicol Ind Health 17(5–10):247–253. https://doi.org/10.1191/0748233701th112oa
Lippmann M, Cohen MD, Chen LC (2015) Health effects of World Trade Center (WTC) dust: an unprecedented disaster’s inadequate risk management. Crit Rev Toxicol 45(6):492–530. https://doi.org/10.3109/10408444.2015.1044601
Thurston G, Maciejczyk P, Lall R, Hwang J, Chen LC (2003) Identification and characterization of World Trade Center disaster fine particulate matter air pollution at a site in Lower Manhattan following September 11. Epidemiology 14(5):S87–S88
Geyh AS, Chillrud S, Williams DL, Herbstman JB, Symons JM, Rees K, Ross J, Kim SR, Lim HJ, Turpin B, Breysse P (2005) Assessing truck driver exposure at the World Trade Center disaster site: personal and area monitoring for particulate matter and volatile organic compounds during October 2001 and April 2002. J Occup Environ Hyg 2(3):179–193. https://doi.org/10.1080/15459620590923154
Wheeler K, McKelvey W, Thorpe L, Perrin M, Cone J, Kass D, Farfel M, Thomas P, Brackbill R (2007) Asthma diagnosed after September 11, 2001 among rescue and recovery workers: findings from the World Trade Center Health Registry. Environ Health Perspect 115(11):1584–1590. https://doi.org/10.1289/ehp.10248
Global Initiative for Chronic Obstructive Lung Disease (2021) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease - 2021 report. https://goldcopd.org/2021-gold-reports/. 1
Mekov E, Nuñez A, Sin DD, Ichinose M, Rhee CK, Maselli DJ, Coté A, Suppli Ulrik C, Maltais F, Anzueto A, Miravitlles M (2021) Update on asthma-COPD overlap (ACO): a narrative review. Int J Chron Obstruct Pulmon Dis 16:1783–1799. https://doi.org/10.2147/copd.s312560
Fletcher CM (1952) The clinical diagnosis of pulmonary emphysema - an experimental study. Proc R Soc Med 45(9):577–584
Williams N (2017) The MRC breathlessness scale. Occup Med (Lond) 67(6):496–497. https://doi.org/10.1093/occmed/kqx086
Ferris BG (1978) Epidemiology standardization project (American Thoracic Society). Am Rev Respir Dis 118(6 Pt 2):1–120
Singh D, Agusti A, Martinez FJ, Papi A, Pavord ID, Wedzicha JA, Vogelmeier CF, Halpin DMG (2022) Blood eosinophils and chronic obstructive pulmonary disease: a GOLD Science Committee 2022 review. Am J Respir Crit Care Med 11:17–24. https://doi.org/10.1164/rccm.202201-0209PP
Hennessy S, Bilker WB, Berlin JA, Strom BL (1999) Factors influencing the optimal control-to-case ratio in matched case-control studies. Am J Epidemiol 149(2):195–197. https://doi.org/10.1093/oxfordjournals.aje.a009786
Richardson DB (2004) An incidence density sampling program for nested case-control analyses. Occup Environ Med 61(12):e59. https://doi.org/10.1136/oem.2004.014472
Austin PC (2009) Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Communications in Statistics - Simulation and Computation 38(6):1228–1234. https://doi.org/10.1080/03610910902859574
Webber MP, Lee R, Soo J, Gustave J, Hall CB, Kelly K, Prezant D (2011) Prevalence and incidence of high risk for obstructive sleep apnea in World Trade Center-exposed rescue/recovery workers. Sleep Breath 15(3):283–294. https://doi.org/10.1007/s11325-010-0379-7
Weber J, Reeves AP, Doucette JT, Jeon Y, Sood A, San José Estépar R, Celedón JC, de la Hoz RE (2020) Quantitative CT evidence of airway inflammation in World Trade Center workers and volunteers with low FVC spirometric pattern. Lung 198(3):555–563. https://doi.org/10.1007/s00408-020-00350-5
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CPM, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J (2005) Interpretative strategies for lung function tests. Eur Respir J 26(5):948–968. https://doi.org/10.1183/09031936.05.00035205
Calverley PMA, Burge PS, Spencer S, Anderson JA, Jones PW (2003) Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax 58(8):659–664. https://doi.org/10.1136/thorax.58.8.659
Feinstein L, Wilkerson J, Salo PM, MacNell N, Bridge MF, Fessler MB, Thorne PS, Mendy A, Cohn RD, Curry MD, Zeldin DC (2020) Validation of questionnaire-based case definitions for chronic obstructive pulmonary disease. Epidemiology 31(3):459–466. https://doi.org/10.1097/ede.0000000000001176
Turner RM, DePietro M, Ding B (2018) Overlap of asthma and chronic obstructive pulmonary disease in patients in the United States: analysis of prevalence, features, and subtypes. JMIR Public Health Surveill 4(3):60. https://doi.org/10.2196/publichealth.9930
Bakakos A, Vogli S, Dimakou K, Hillas G (2022) Asthma with fixed airflow obstruction: from fixed to personalized approach. J Pers Med 12(3):333. https://doi.org/10.3390/jpm12030333
Prasad S, Gao CX, Borg B, Broder J, Brown D, Ikin JF, Makar A, McCrabb T, Hoy R, Thompson B, Abramson MJ (2022) Chronic obstructive pulmonary disease in adults exposed to fine particles from a coal mine fire. Ann Am Thorac Soc 19(2):186–195. https://doi.org/10.1513/AnnalsATS.202012-1544OC
Mehta AJ, Miedinger D, Keidel D, Bettschart R, Bircher A, Bridevaux PO, Curjuric I, Kromhout H, Rochat T, Rothe T, Russi EW, Schikowski T, Schindler C, Schwartz J, Turk A, Vermeulen R, Probst-HenschKünzli NN (2012) Occupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults. Am J Respir Crit Care Med 185(12):1292–1300. https://doi.org/10.1164/rccm.201110-1917OC
Blanc PD, Annesi-Maesano I, Balmes JR, Cummings KJ, Fishwick D, Miedinger D, Murgia N, Naidoo RN, Reynolds CJ, Sigsgaard T, Toren K, Vinnikov D, Redlich CA (2019) The occupational burden of nonmalignant respiratory diseases - an official American Thoracic Society and European Respiratory Society Statement. Am J Respir Crit Care Med 199(11):1312–1334. https://doi.org/10.1164/rccm.201904-0717ST
Szeinuk J, de la Hoz RE (2022) Occupational chronic obstructive pulmonary disease. In: Bang KM (ed) Modern Occupational Disease Diagnosis, Epidemiology, Management and Prevention, vol 1, 1st edn. Bentham Science Books, Singapore, pp 104–127
Hendryx M, Luo J, Chojenta C, Byles JE (2019) Air pollution exposures from multiple point sources and risk of incident chronic obstructive pulmonary disease (COPD) and asthma. Environ Res 179(Pt A):108783. https://doi.org/10.1016/j.envres.2019.108783
Hoffman EA, Ahmed FS, Baumhauer H, Budoff M, Carr JJ, Kronmal R, Reddy S, Barr RG (2014) Variation in the percent of emphysema-like lung in a healthy, nonsmoking multiethnic sample - The MESA Lung Study. Ann Am Thorac Soc 11(6):898–907. https://doi.org/10.1513/AnnalsATS.201310-364OC
Young KA, Regan EA, Han MK, Lutz SM, Ragland M, Castaldi PJ, Washko GR, Cho MH, Strand M, Curran-Everett D, Beaty TH, Bowler RP, Wan ES, Lynch DA, Make BJ, Silverman EK, Crapo JD, Hokanson JE, Kinney GL (2019) Subtypes of COPD have unique distributions and differential risk of mortality. Chronic Obstr Pulm Dis 6(5):400–413. https://doi.org/10.15326/jcopdf.6.5.2019.0150
Engstrom G, Lind P, Hedblad B, Wollmer P, Stavenow L, Janzon L, Lindgarde F (2002) Lung function and cardiovascular risk: relationship with inflammation-sensitive plasma proteins. Circulation 106(20):2555–2560. https://doi.org/10.1161/01.cir.0000037220.00065.0d
Engstrom G, Hedblad B, Nilsson P, Wollmer P, Berglund G, Janzon L (2003) Lung function, insulin resistance and incidence of cardiovascular disease: a longitudinal cohort study. J Intern Med 253(5):574–581. https://doi.org/10.1046/j.1365-2796.2003.01138.x
Johnston AK, Mannino DM, Hagan GW, Davis KJ, Kiri VA (2008) Relationship between lung function impairment and incidence or recurrence of cardiovascular events in a middle-aged cohort. Thorax 63(7):599–605. https://doi.org/10.1136/thx.2007.088112
Hickson DA, Burchfiel CM, Liu J, Petrini MF, Harrison K, White WB, Sarpong DF (2011) Diabetes, impaired glucose tolerance, and metabolic biomarkers in individuals with normal glucose tolerance are inversely associated with lung function: the Jackson Heart Study. Lung 189(4):311–321. https://doi.org/10.1007/s00408-011-9296-1
Godfrey MS, Jankowich MD (2016) The vital capacity is vital: epidemiology and clinical significance of the restrictive spirometry pattern. Chest 149(1):238–251. https://doi.org/10.1378/chest.15-1045
Zeig-Owens R, Singh A, Aldrich TK, Hall CB, Schwartz T, Webber MP, Cohen HW, Kelly KJ, Nolan A, Prezant DJ, Weiden MD (2018) Blood leukocyte concentrations, FEV1 decline, and airflow limitation - a 15-year longitudinal study of World Trade Center-exposed firefighters. Ann Am Thorac Soc 15(2):173–183. https://doi.org/10.1513/AnnalsATS.201703-276OC
McGee JK, Chen LC, Cohen MD, Chee GR, Prophete CM, Haykal-Coates N, Wasson SJ, Conner TL, Costa DL, Gavett SH (2003) Chemical analysis of World Trade Center fine particulate matter for use in toxicologic assessment. Environ Health Perspect 111(7):972–980. https://doi.org/10.1289/ehp.5930
Napier CO, Mbadugha O, Bienenfeld LA, Doucette JT, Lucchini R, Luna-Sánchez S, de la Hoz RE (2017) Obesity and weight gain among former World Trade Center workers and volunteers. Arch Environ Occup Health 72(2):106–110. https://doi.org/10.1080/19338244.2016.1197174
Grahame TJ, Klemm R, Schlesinger RB (2014) Public health and components of particulate matter: the changing assessment of black carbon. J Air Waste Manag Assoc 64(6):620–660. https://doi.org/10.1080/10962247.2014.912692
Aaron SD, Tan WC, Bourbeau J, Sin DD, Loves RH, MacNeil J, Whitmore GA (2017) Diagnostic instability and reversals of chronic obstructive pulmonary disease diagnosis in individuals with mild to moderate airflow obstruction. Am J Respir Crit Care Med 196(3):306–314. https://doi.org/10.1164/rccm.201612-2531OC
Acknowledgements
The authors would like to thank all participants in this study, and the staff of the Mount Sinai WTC Health Program Clinical Center of Excellence, and the WTC General Responders Cohort Data Center. Preliminary results of this work were presented as an abstract at the 2021 International Congress of the European Respiratory Society (Eur Respir J 2021;58 (Suppl 65):PA3353, https://doi.org/10.1183/13993003.congress-2021.PA3353), and as a preprint in SSRN (http://dx.doi.org/10.2139/ssrn.4353884). Dr. Roberto Lucchini is presently at the Department of Occupational and Environmental Health Sciences of the Robert Stempel College of Public Health and Social Work at Florida International University, Miami, FL, USA.
Funding
This work was supported by cooperative agreements No. U01 OH011697 (RED, PI), U01 OH011300 (AN, PI), and contract 200-2017-93325 (WTC General Responders Cohort Data Center, RGL, PI) from the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health (CDCP/NIOSH).
Author information
Authors and Affiliations
Contributions
RED, MS, and JCC designed and oversaw the study and selected analytical strategies. MS performed all statistical analyses. All authors contributed to writing, reviewed, and revised the drafts, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors had no other relevant financial conflict of interest to disclose. The contents of this article are the sole responsibility of the authors, and do not represent the official views of the CDCP/NIOSH.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de la Hoz, R.E., Shapiro, M., Nolan, A. et al. Association of World Trade Center (WTC) Occupational Exposure Intensity with Chronic Obstructive Pulmonary Disease (COPD) and Asthma COPD Overlap (ACO). Lung 201, 325–334 (2023). https://doi.org/10.1007/s00408-023-00636-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-023-00636-4