Abstract
Purpose
Acute exacerbations of COPD (AECOPD) are important factors contributing to mortality risk. The rate of exacerbations varies overtime. An inconsistent pattern of exacerbation occurrence is a common finding. The mortality risk associated with such a pattern is not entirely clear. Our objective was to assess the risk of mortality associated with various possible patterns of AECOPD trajectories.
Methods
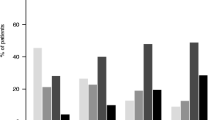
This is a multicenter historical cohort study. Four different exacerbation trajectories were defined according to the incidence of severe AECOPD requiring hospital admission 2 years before and after the date of the first visit to the respiratory clinic—Consistent non-exacerbators (NEx): no AECOPD before or after the index date; consistent exacerbators (Ex): at least one AECOPD both before and after the index date; converters to exacerbators (CONV-Ex): no exacerbations before and at least one AECOPD after the index date; converters to non-exacerbators (CONV-NEx): at least one AECOPD before the index date, and no exacerbations after said date. All-cause mortality risk for these trajectories was assessed.
Results
A total of 1713 subjects were included in the study: NEx: 1219 (71.2%), CONV-NEx: 225 (13.1%), CONV-Ex: 148 (8.6%), Ex: 121 (7.1%). After correcting for confounding variables, the group with the highest mortality risk was Ex. The CONV-Ex and CONV-Nex groups had a mortality risk between Ex and NEx, with no significant differences between them.
Conclusion
Different possible trajectories of severe AECOPD before and after a first specialized consultation are associated with different mortality risks. An inconsistent pattern of exacerbations has a mortality risk between Ex and NEx, with no clear differences between CONV-Ex and CONV-NEx.

Similar content being viewed by others
Data availability
The data were anonymized for analysis.
References
Suissa S, Dell’Aniello S, Ernst P (2012) Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax 67:957–963. https://doi.org/10.1136/thoraxjnl-2011-201518
Soler-Cataluna JJ, Martinez-Garcia MA, Roman SP et al (2005) Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 60:925–931. https://doi.org/10.1136/thx.2005.040527
Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. 2022 report. https://goldcopd.org/2022-gold-reports-2/. Accessed 20 June 2022
Sadatsafavi M, McCormack J, Petkau J et al (2021) Should the number of acute exacerbations in the previous year be used to guide treatments in COPD? Eur Respir J 57:2002122. https://doi.org/10.1183/13993003.02122-2020
Han MK, Quibrera PM, Carretta EE et al (2017) Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med 5:619–626. https://doi.org/10.1016/S2213-2600(17)30207-2
Lipson DA, Barnhart F, Brealey N et al (2018) Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med 378:1671–1680. https://doi.org/10.1056/NEJMoa1713901
Rabe KF, Martinez FJ, Ferguson GT et al (2020) Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med 383:35–48. https://doi.org/10.1056/NEJMoa1916046
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Klein JP, Moeschberger ML (2003) Survival analysis. Techniques for censored and truncated data, 2nd edn. Springer Publishers, New York
Whittaker H, Rubino A, Müllerova H et al (2022) Frequency and severity of exacerbations of COPD associated with future risk of exacerbations and mortality: a UK routine health care data study. Int J Chron Obstruct Pulmon Dis 17:427–437. https://doi.org/10.2147/COPD.S346591
Sadatsafavi M, Xie H, Etminan M et al (2018) The association between previous and future severe exacerbations of chronic obstructive pulmonary disease: updating the literature using robust statistical methodology. PLoS ONE 13(1):e0191243. https://doi.org/10.1371/journal.pone.0191243
Le Rouzic O, Roche N, Cortot AB et al (2018) Defining the “frequent exacerbator” phenotype in COPD. A hypothesis-free approach. Chest 153:1106–1115. https://doi.org/10.1016/j.chest.2017.10.009
Reilev M, Lykkegaard J, Halling A et al (2017) Stability of the frequent exacerbator in the general population: a Danish nationwide register-based study. Primary Care Respir Med 27(1):25. https://doi.org/10.1038/s41533-017-0029-7
Donaldson GC, Müllerova H, Locantore N et al (2013) Factors associated with change in exacerbation frequency in COPD. Respir Res 14(1):79. https://doi.org/10.1186/1465-9921-14-79
Cote CG, Dordelly LJ, Celli BR (2007) Impact of COPD exacerbations on patient-centered outcomes. Chest 131:696–704. https://doi.org/10.1378/chest.06-1610
Ferguson GT, Rabe KF, Martinez FJ et al (2018) Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir Med 6:747–758. https://doi.org/10.1016/S2213-2600(18)30327-8
Martinez FJ, Ferguson GT, Bourne E et al (2021) Budesonide/glycopyrrolate/formoterol fumarate metered dose inhaler improves exacerbation outcomes in patients with COPD without a recent exacerbation history: a subgroup analysis of KRONOS. Int J Chron Obstruct Pulmon Dis 16:179–189. https://doi.org/10.2147/COPD.S286087
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
RG contributed to the study concept, design, acquisition of data, analysis, interpretation of data, and drafting of the first version of the manuscript; JMF-G contributed to the acquisition of data, analysis, and interpretation of data; CAA-D, AE-M, and LG-R contributed to the acquisition of data. JMF-G, CAA-D, AE-M, LG-R, DD-R, IG-T, and CE contributed to the critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
Rafael Golpe declares that he has received speaking or advisory fees, or economic aid to attend congresses from Astra-Zeneca, GSK, Novartis, Chiesi, Mundipharma, Menarini, TEVA, Grifols, Ferrer, Boehringer-Ingelheim, Rovi, and Gebro Pharma, outside the submitted work. Juan Marco Figueira-Gonçalves has received honoraria for speaking engagements and funding for conference attendance from Laboratorios Esteve, MundiPharma, AstraZeneca, Boehringer Ingelheim, Ferrer, Menarini, Rovi, GlaxoSmithKline, Chiesi, Novartis, and Gebro Pharma outside the submitted work. Carlos Antonio Amado-Diago has received speaker or consulting fees from Boehringer Ingelheim, Pfizer, AstraZeneca, Novartis, Chiesi, Faes Farma, Esteve and GlaxoSmithKline, outside the submitted work. David Dacal-Rivas reports personal fees and non-financial support from Esteve, personal fees and non-financial support from Boehringer-Ingelheim, non-financial support from GSK, non-financial support from Novartis, non-financial support from TEVA, non-financial support from Chiesi, non-financial support from Ferrer, outside the submitted work. The rest of the authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This observational, non-intervention retrospective study was performed in line with the principles of the Declaration of Helsinki. The study was authorized by Comité de Ética e Investigación Clínica del Hospital Universitario Nuestra Señora de Candelaria (Registry No: CHUNSC_2022_45).
Informed Consent
Informed consent was waived for this analysis due to the non-interventional retrospective design of the study and the use of anonymous clinical data for the analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Golpe, R., Figueira-Gonçalves, J.M., Amado-Diago, C.A. et al. Trajectories of Severe Exacerbations of Chronic Obstructive Pulmonary Disease and Their Relationship with Mortality Risk. Lung 200, 601–607 (2022). https://doi.org/10.1007/s00408-022-00565-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00565-8