Abstract
Introduction
To increase CO2 elimination and to reduce work of breathing in hypercapnic patients, non-invasive ventilation (NIV) can be applied via mask either with non-vented CO2 exhalation systems or with vented systems with leak port. The effect of the exhalation system on CO2 rebreathing in the mask and total gas exchange remains widely unknown. Aim of this study was to compare the exhalation systems in terms of inspiratory O2 and CO2 concentrations, breathing patterns and gas exchange.
Methods
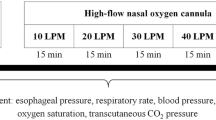
We prospectively examined 10 healthy subjects and 10 hypercapnic patients with both exhalation systems. O2 and CO2 were measured in the nose, in the mask, and in the ventilation circuit, and respiratory rate, tidal volume, and transcutaneous capnometry (PtcCO2) were recorded during the experiments.
Results
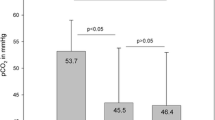
Using the non-vented system, CO2 concentrations in the mask were significantly higher in both subject groups, and PtcCO2 values in the patient group increased up to 3.6 mmHg compared to the vented system (p = 0.011). O2 concentrations increased with higher O2 flow rates, but were significantly lower in the vented settings in both groups. No effect in breathing pattern could be demonstrated during the measurement time.
Conclusion
Using NIV, the chosen exhalation system influences CO2 and O2 concentrations under the mask, CO2 rebreathing from the mask and could influence the effectiveness of the ventilation support with regards to hypercapnia treatment. To compensate for relevant hypoxia, the O2 supplementation must be set up to a sufficient level under a vented system.




Similar content being viewed by others
References
Mehta S, Hill NS (2001) Noninvasive ventilation. Am J Respir Crit Care Med 163(2):540–577. https://doi.org/10.1164/ajrccm.163.2.990611
Macrea M, Oczkowski S, Rochwerg B et al (2020) Long-term noninvasive ventilation in chronic stable hypercapnic chronic obstructive pulmonary disease. An Official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med 202(4):e74–e87. https://doi.org/10.1164/rccm.202006-2382ST
Köhnlein T, Windisch W, Köhler D et al (2014) Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med 2(9):698–705. https://doi.org/10.1016/S2213-2600(14)70153-5
Murphy PB, Rehal S, Arbane G et al (2017) Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation: a randomized clinical trial. JAMA 317(21):2177–2186. https://doi.org/10.1001/jama.2017.4451
Dreher M, Storre JH, Schmoor C, Windisch W (2010) High-intensity versus low-intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised crossover trial. Thorax 65(4):303–308. https://doi.org/10.1136/thx.2009.124263
Lukácsovits J, Carlucci A, Hill N et al (2012) Physiological changes during low- and high-intensity noninvasive ventilation. Eur Respir J 39(4):869–875. https://doi.org/10.1183/09031936.00056111
Schwarz SB, Magnet FS, Windisch W (2017) Why high-intensity NPPV is favourable to low-intensity NPPV: clinical and physiological reasons. COPD 14(4):389–395. https://doi.org/10.1080/15412555.2017.1318843
Windisch W, Dreher M, Geiseler J et al (2017) S2k-Leitlinie: Nichtinvasive und invasive Beatmung als Therapie der chronischen respiratorischen Insuffizienz – Revision 2017 [Guidelines for non-invasive and invasive home mechanical ventilation for treatment of chronic respiratory failure - update 2017]. Pneumologie 71(11):722–795. https://doi.org/10.1055/s-0043-118040
Lebret M, Léotard A, Pépin JL et al (2021) Nasal versus oronasal masks for home non-invasive ventilation in patients with chronic hypercapnia: a systematic review and individual participant data meta-analysis. Thorax 76(11):1108–1116. https://doi.org/10.1136/thoraxjnl-2020-215613
Schettino GP, Chatmongkolchart S, Hess DR, Kacmarek RM (2003) Position of exhalation port and mask design affect CO2 rebreathing during noninvasive positive pressure ventilation. Crit Care Med 31(8):2178–2182. https://doi.org/10.1097/01.CCM.0000081309.71887.E9
Saatci E, Miller DM, Stell IM, Lee KC, Moxham J (2004) Dynamic dead space in face masks used with noninvasive ventilators: a lung model study. Eur Respir J 23(1):129–135. https://doi.org/10.1183/09031936.03.00039503
Storre JH, Huttmann SE, Ekkernkamp E et al (2014) Oxygen supplementation in noninvasive home mechanical ventilation: the crucial roles of CO2 exhalation systems and leakages. Respir Care 59(1):113–120. https://doi.org/10.4187/respcare.02596
Thys F, Liistro G, Dozin O, Marion E, Rodenstein DO (2002) Determinants of Fi, O2 with oxygen supplementation during noninvasive two-level positive pressure ventilation. Eur Respir J 19(4):653–657. https://doi.org/10.1183/09031936.02.00263102
Schwartz AR, Kacmarek RM, Hess DR (2004) Factors affecting oxygen delivery with bi-level positive airway pressure. Respir Care 49(3):270–275
Samolski D, Antón A, Güell R, Sanz F, Giner J, Casan P (2006) Inspired oxygen fraction achieved with a portable ventilator: determinant factors. Respir Med 100(9):1608–1613. https://doi.org/10.1016/j.rmed.2005.12.005
Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338. https://doi.org/10.1183/09031936.05.00034805
Wanger J, Clausen JL, Coates A et al (2005) Standardisation of the measurement of lung volumes. Eur Respir J 26(3):511–522. https://doi.org/10.1183/09031936.05.00035005
Vianello A, Arcaro G, Molena B et al (2018) Effect of a passive exhalation port on tracheostomy ventilation in amyotrophic lateral sclerosis patients: a randomized controlled trial. J Thorac Dis 10(2):1007–1014. https://doi.org/10.21037/jtd.2018.01.102
Möller W, Feng S, Domanski U et al (2017) Nasal high flow reduces dead space. J Appl Physiol 122(1):191–197. https://doi.org/10.1152/japplphysiol.00584.2016
Miyoshi E, Fujino Y, Uchiyama A, Mashimo T, Nishimura M (2005) Effects of gas leak on triggering function, humidification, and inspiratory oxygen fraction during noninvasive positive airway pressure ventilation. Chest 128(5):3691–3698. https://doi.org/10.1378/chest.128.5.3691
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
KJF: draft of the article, conception and design, analysis and interpretation of data, critical review, final approval. GN, MS, BD, UD: conception and design, analysis and interpretation of data, critical review, draft correction and proof reading, final approval.
Corresponding author
Ethics declarations
Conflict of interest
KJ Franke, M Schroeder, U Domanski, and B Dewald have no financial or other potential conflicts of interest associated with this study. G Nilius has received research support from Fisher & Paykel Healthcare, Heinen und Löwenstein, ResMed and Weinmann; this has gone into department funds.
Ethical Approval
The study was approved under Nr 13/2014 of the ethics committee of University Witten/Herdecke.
Informed Consent
Informed consent was obtained from all individual participants. The study was already presented at the European Respiratory Society (KJ Franke, U Domanski, M Schroeder, B Stoehr, G Nilius. Non-invasive ventilation: Effect of a vented and a non-vented CO2 exhalation system on O2- and CO2-concentration. European Respiratory Journal 2016 48: OA3533; https://doi.org/10.1183/13993003.congress-2016.OA3533).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Franke, KJ., Schroeder, M., Domanski, U. et al. Non-invasive Ventilation: Effect of Vented and Non-vented Exhalation Systems on Inspiratory CO2 and O2 Concentrations, Ventilation, and Breathing Pattern. Lung 200, 251–260 (2022). https://doi.org/10.1007/s00408-022-00520-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00520-7