Abstract
Purpose
This study aimed to evaluate the associations between dyslipidemia and pulmonary function parameters assessed by spirometry and the forced oscillation technique in asthmatic children.
Methods
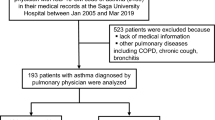
Asthmatic children (5–18 years old) had fasting serum lipid profiles including low-density lipoprotein cholesterol (LDL-C), total cholesterol (TC), triglyceride (TG), and high-density lipoprotein cholesterol (HDL-C) concentrations, and C-reactive protein (CRP) measured. Pulmonary function tests were assessed by spirometry and the forced oscillation technique (FOT).
Results
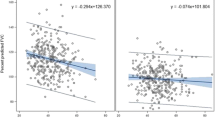
One hundred forty-one asthmatic children were enrolled with a mean (SD) age of 11.82 (3.38) years. Eighty-eight (62.4%) children were boys, 64 (45.4%) had dyslipidemia, and 20 (14.2%) were obese. Among the children with dyslipidemia, a high LDL-C concentration (65.6%) was the most common form of dyslipidemia, followed by high TC (57.8%), high TG (35.9%), and low HDL-C concentrations (15.6%). Multivariable analysis showed significant associations between HDL-C concentrations and respiratory resistance at 5 Hz (R5) and respiratory resistance at 20 Hz (R20), and TC concentrations were modestly associated with reactance at 5 Hz (X5), the frequency of resonance (Fres), and the area of reactance (ALX). Asthmatic children who had high LDL-C concentrations had a significantly higher expiratory phase R5, whole breath R20, and expiratory phase R20 than those in children with normal LDL-C concentrations.
Conclusion
This study suggests an association of blood cholesterol, especially HDL-C and LDL-C, and respiratory resistance measured by the FOT, irrespective of the obesity status. An intervention for improving LDL-C and HDL-C concentrations may be beneficial on lung function parameters in asthmatic children.
Clinical Trial Registration: TCTR20200305005; date of registration: 03-04-2020 (retrospectively registered).

Similar content being viewed by others
Data Availability
The data that support the findings of this study are not publicly available because they contain information that could compromise the privacy of research participants but are available from the corresponding author (W.M.) upon reasonable request.
Abbreviations
- FVC:
-
Forced vital capacity
- FEV1 :
-
Forced expiratory volume in 1 second
- FEF25–75 :
-
Forced expiratory flow at 25–75% of FVC
- PACT:
-
Pediatric asthma control test
- PAQLQ:
-
Pediatric Asthma Quality of Life Questionnaire
- CRP:
-
C-reactive protein
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- FOT:
-
Forced oscillation technique
- R5 :
-
Respiratory resistance at 5 Hz
- R20 :
-
Respiratory resistance at 20 Hz
- X5 :
-
Respiratory reactance at 5 Hz
- ALX:
-
Area of reactance
- Fres:
-
Resonance frequency
References
Vinding RK, Stokholm J, Chawes BLK, Bisgaard H (2016) Blood lipid levels associate with childhood asthma, airway obstruction, bronchial hyperresponsiveness, and aeroallergen sensitization. J Allergy Clin Immunol 137:68–74. https://doi.org/10.1016/j.jaci.2015.05.033
Lu M, Wu B, Qiao R, Gu H, Din Y, Dong X (2019) No associations between serum lipid levels or HOMA-IR and asthma in children and adolescents: a NHANES analysis. J Clin Res Pediatr Endocrinol 11:270–277. https://doi.org/10.4274/jcrpe.galenos.2019.2018.0098
Expert Panel on Integrated Guidelines for Cardiovascular Health, Risk Reduction in Children and Adolescents (2011) Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128(Suppl 5):S213–S256. https://doi.org/10.1542/peds.2009-2107C
Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL (2015) Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999–2012. JAMA Pediatr 169:272–279. https://doi.org/10.1001/jamapediatrics.2014.3216
Kavey RE (2015) Combined dyslipidemia in childhood. J Clin Lipidol 9:S41–S56. https://doi.org/10.1016/j.jacl.2015.06.008
Nur Zati Iwani AK, Jalaludin MY, Wan Mohd Zin RM, Fuziah MZ, Hong JYH, Abqariyah Y et al (2019) TG: HDL-C ratio is a good marker to identify children affected by obesity with increased cardiometabolic risk and insulin resistance. Int J Endocrinol 2019:8586167. https://doi.org/10.1155/2019/8586167
Ko SH, Jeong J, Baeg MK, Han KD, Kim HS, Yoon JS et al (2018) Lipid profiles in adolescents with and without asthma: Korea National Health and nutrition examination survey data. Lipids Health Dis 17:158. https://doi.org/10.1186/s12944-018-0807-4
Chanachon PN, Jotikasthira W, Kiewngam P, Sawatchai A, Kanchongkittiphon W, Manuyakorn W (2021) TG/HDL-C ratio independent of obesity associates with airflow obstruction in children with asthma. Indian J Pediatr. https://doi.org/10.1007/s12098-021-03942-y
Fenger RV, Gonzalez-Quintela A, Linneberg A, Husemoen LL, Thuesen BH, Aadahl M et al (2013) The relationship of serum triglycerides, serum HDL, and obesity to the risk of wheezing in 85,555 adults. Respir Med 107:816–824. https://doi.org/10.1016/j.rmed.2013.02.001
Oostveen E, MacLeod D, Lorino H, Farre R, Hantos Z, Desager K et al (2003) The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J 22:1026–1041. https://doi.org/10.1183/09031936.03.00089403
Bisgaard H, Klug B (1995) Lung function measurement in awake young children. Eur Respir J 8:2067–2075
Schulze J, Smith HJ, Fuchs J, Herrmann E, Dressler M, Rose MA et al (2012) Methacholine challenge in young children as evaluated by spirometry and impulse oscillometry. Respir Med 106:627–634. https://doi.org/10.1016/j.rmed.2012.01.007
Brashier B, Salvi S (2015) Measuring lung function using sound waves: role of the forced oscillation technique and impulse oscillometry system. Breathe (Sheff) 11:57–65. https://doi.org/10.1183/20734735.020514
de Oliveira Jorge PP, de Lima JHP, Chong ESDC, Medeiros D, Sole D, Wandalsen GF (2019) Impulse oscillometry in the assessment of children’s lung function. Allergol Immunopathol (Madr) 47:295–302. https://doi.org/10.1016/j.aller.2018.03.003
Komarow HD, Myles IA, Uzzaman A, Metcalfe DD (2011) Impulse oscillometry in the evaluation of diseases of the airways in children. Ann Allergy Asthma Immunol 106:191–199. https://doi.org/10.1016/j.anai.2010.11.011
Skylogianni E, Douros K, Anthracopoulos MB, Fouzas S (2016) The forced oscillation technique in paediatric respiratory practice. Paediatr Respir Rev 18:46–51. https://doi.org/10.1016/j.prrv.2015.11.001
Barochia AV, Kaler M, Cuento RA, Gordon EM, Weir NA, Sampson M et al (2015) Serum apolipoprotein A-I and large high-density lipoprotein particles are positively correlated with FEV1 in atopic asthma. Am J Respir Crit Care Med 191:990–1000. https://doi.org/10.1164/rccm.201411-1990OC
Peng J, Huang Y (2017) Meta-analysis of the association between asthma and serum levels of high-density lipoprotein cholesterol and low-density lipoprotein cholesterol. Ann Allergy Asthma Immunol 118:61–65. https://doi.org/10.1016/j.anai.2016.09.447
Su X, Ren Y, Li M, Zhao X, Kong L, Kang J (2018) Association between lipid profile and the prevalence of asthma: a meta-analysis and systemic review. Curr Med Res Opin 34:423–433. https://doi.org/10.1080/03007995.2017.1384371
Scichilone N, Rizzo M, Benfante A, Catania R, Giglio RV, Nikolic D et al (2013) Serum low density lipoprotein subclasses in asthma. Respir Med 107:1866–1872. https://doi.org/10.1016/j.rmed.2013.09.001
Rastogi D, Fraser S, Oh J, Huber AM, Schulman Y, Bhagtani RH et al (2015) Inflammation, metabolic dysregulation, and pulmonary function among obese urban adolescents with asthma. Am J Respir Crit Care Med 191:149–160. https://doi.org/10.1164/rccm.201409-1587OC
Welty FK, Alfaddagh A, Elajami TK (2016) Targeting inflammation in metabolic syndrome. Transl Res 167:257–280. https://doi.org/10.1016/j.trsl.2015.06.017
Cheng AY, Leiter LA (2006) Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. Curr Opin Cardiol 21:400–404. https://doi.org/10.1097/01.hco.0000231412.15049.fb
Forno E, Weiner DJ, Mullen J, Sawicki G, Kurland G, Han YY et al (2017) Obesity and airway dysanapsis in children with and without asthma. Am J Respir Crit Care Med 195:314–323. https://doi.org/10.1164/rccm.201605-1039OC
Dixon AE, Peters U (2018) The effect of obesity on lung function. Expert Rev Respir Med 12:755–767. https://doi.org/10.1080/17476348.2018.1506331
Jones MH, Roncada C, Fernandes MTC, Heinzmann-Filho JP, Sarria Icaza EE, Mattiello R et al (2017) Asthma and obesity in children are independently associated with airway dysanapsis. Front Pediatr 5:270. https://doi.org/10.3389/fped.2017.00270
Kalhoff H, Breidenbach R, Smith HJ, Marek W (2011) Impulse oscillometry in preschool children and association with body mass index. Respirology 16:174–179. https://doi.org/10.1111/j.1440-1843.2010.01906.x
Lauhkonen E, Koponen P, Nuolivirta K, Paassilta M, Toikka J, Saari A et al (2015) Obesity and bronchial obstruction in impulse oscillometry at age 5–7 years in a prospective post-bronchiolitis cohort. Pediatr Pulmonol 50:908–914. https://doi.org/10.1002/ppul.23085
Lovinsky-Desir S, Lussier SJ, Calatroni A, Gergen PJ, Rivera-Spoljaric K, Bacharier LB et al (2021) Trajectories of adiposity indicators and association with asthma and lung function in urban minority children. J Allergy Clin Immunol. https://doi.org/10.1016/j.jaci.2021.06.015
Rerksuppaphol S, Rerksuppaphol L (2011) Prevalence of dyslipidemia in Thai schoolchildren. J Med Assoc Thai 94:710–715
Stocks J, Sonnappa S, Lum S (2014) Lung function testing in children: importance of race and ethnic-specific reference equations. Expert Rev Respir Med 8:527–531. https://doi.org/10.1586/17476348.2014.927317
Sonnappa S, Bastardo CM, Stafler P, Bush A, Aurora P, Stocks J (2011) Ethnic differences in fraction of exhaled nitric oxide and lung function in healthy young children. Chest 140:1325–1331. https://doi.org/10.1378/chest.10-3280
Alblooshi A, Alkalbani A, Albadi G, Narchi H, Hall G (2017) Is forced oscillation technique the next respiratory function test of choice in childhood asthma. World J Methodol 7:129–138. https://doi.org/10.5662/wjm.v7.i4.129
Scaduto F, Giglio RV, Benfante A, Nikolic D, Montalto G, Rizzo M et al (2018) Serum lipoproteins are not associated with the severity of asthma. Pulm Pharmacol Ther 50:57–61. https://doi.org/10.1016/j.pupt.2018.04.001
Acknowledgements
We would like to thank Ms Cherapat Sasisakulporn for helping in performing the FOT and spirometry measurement.
Funding
This work was supported by the Faculty of Medicine Ramathibodi Hospital, Mahidol University.
Author information
Authors and Affiliations
Contributions
PNC, WK, and WM designed the study. PNC, WJ, and PK contributed to data collection. PNC, AS, and WM performed the statistical analysis and interpretation of the results. PNC and WM drafted the manuscript. WK and WM edited the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.The data that support the findings of this study are not publicly available because they contain information that could compromise the privacy of research participants but are available from the corresponding author (W.M.) upon reasonable request.
Ethical Approval
Ethical approval was provided by the Human Rights and Ethics Committee of the Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand (ID: MURA2019/55).
Consent to Participate
Written informed consent and informed written assent for children aged 7 years or older were obtained for all participants and their parents.
Consent for Publication
Written informed consent and informed written assent for children aged 7 years or older were obtained for all participants and their parents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chanachon, P.N., Jotikasthira, W., Kiewngam, P. et al. Association of Dyslipidemia and Respiratory Resistance Assessed by the Forced Oscillation Technique in Asthmatic Children. Lung 200, 73–82 (2022). https://doi.org/10.1007/s00408-021-00502-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-021-00502-1