Abstract
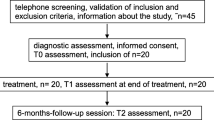
The Metacognitive Training for Depression (D-MCT) is a highly structured group therapy that has been shown to be effective in reducing depressive symptoms. First evidence suggests that need for control represents a mechanism of change. However, more research is needed to evaluate the mode of action of each module and identify predictors of treatment response. Two sequential studies (one naturalistic pilot study [study I, N = 45] and one randomized controlled trial [study II, N = 32]) were conducted to evaluate the session-specific effects and predictors of D-MCT in patients with depression. The D-MCT was conducted over eight weeks, and patients answered a questionnaire on dysfunctional beliefs (e.g., negative filter) and depressive symptoms (e.g., lack of energy, self-esteem) before and after each session. Linear mixed-effects models showed that several dysfunctional beliefs and symptoms improved over the course of the treatment; three modules were able to evoke within-session effects, but no between-session effects were found. The improvement in lack of energy in one module was identified as a relevant predictor in study I via lasso regression but was not replicated in study II. Exploratory analyses revealed further predictors that warrant replication in future studies. The identified predictors were inconclusive when the two studies were compared, which may be explained by the different instruments administered. Even so, the results may be used to revise questionnaires and improve the intervention.



Similar content being viewed by others
Availability of data and material
The data supporting the results and analyses presented in the paper are available upon request from first author.
References
Vos T, Abajobir AA, Abbafati C, Abbas KM, Abate KH, Abd-Allah F et al (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100):1211–1259
National Institute for Health & Clinical Excellence (NICE) (2020) The nice guideline on the treatment and management of depression [Internet]
Cuijpers P, Van Straten A, Warmerdam L (2008) Are individual and group treatments equally effective in the treatment of depression in adults? A meta-analysis. Eur J Psychiatry 22(1):38–51
McDermut W, Miller IW, Brown RA (2001) The efficacy of group psychotherapy for depression: a meta-analysis and review of the empirical research. Clin Psychol Sci Pract 8(1):98–116
Cuijpers P, Noma H, Karyotaki E, Cipriani A, Furukawa TA (2019) Effectiveness and acceptability of cognitive behavior therapy delivery formats in adults with depression: a network meta-analysis. JAMA Psychiat 76(7):700–707
Bundespsychotherapeutenkammer (2011) BPtK-Studie zu Wartezeiten in der ambulanten psychotherapeutischen Versorgung. Umfrage der Landespsychotherapeutenkammern und der BPtK. BPtK 46
Jelinek L, Hauschildt M, Moritz S (2015) Metakognitives Training bei Depression (D-MKT). Beltz, J, Weinheim
Moritz S, Woodward TS (2007) Metacognitive training for schizophrenia patients (MTC): a pilot study on feasibility, treatment adherence, and subjective efficacy. Ger J Psychiatry 10:69–78
Eichner C, Berna F (2016) Acceptance and efficacy of metacognitive training (MCT) on positive symptoms and delusions in patients with schizophrenia: a meta-analysis taking into account important moderators. Schizophr Bull 42(4):952–962
Liu Y-C, Tang C-C, Hung T-T, Tsai P-C, Lin M-F (2018) The efficacy of metacognitive training for delusions in patients with schizophrenia: a meta-analysis of randomized controlled trials informs evidence-based practice. Worldviews Evid-Based Nurs 15(2):130–139
Jelinek L, Hauschildt M, Wittekind CE, Schneider BC, Kriston L, Moritz S (2016) Efficacy of metacognitive training for depression: a randomized controlled trial. Psychother Psychosom 85(4):231–234
Moritz S, Schneider BC, Peth J, Arlt S, Jelinek L (2018) Metacognitive Training for Depression (D-MCT) reduces false memories in depression. A randomized controlled trial. Eur Psychiatry. https://doi.org/10.1016/j.eurpsy.2018.05.010
Jelinek L, Moritz S, Hauschildt M (2017) Patients’ perspectives on treatment with Metacognitive Training for Depression (D-MCT): results on acceptability. J Affect Disord 221:17–24
Lorenzo-Luaces L, German RE, DeRubeis RJ (2015) It’s complicated: the relation between cognitive change procedures, cognitive change, and symptom change in cognitive therapy for depression. Clin Psychol Rev 41:3–15
Brouwer ME, Williams AD, Forand NR, DeRubeis RJ, Bockting CLH (2019) Dysfunctional attitudes or extreme response style as predictors of depressive relapse and recurrence after mobile cognitive therapy for recurrent depression. J Affect Disord 243:48–54
Lemmens LHJM, Müller VNLS, Arntz A, Huibers MJH (2016) Mechanisms of change in psychotherapy for depression: an empirical update and evaluation of research aimed at identifying psychological mediators. Clin Psychol Rev 50:95–107
Beck AT (1964) Thinking and depression: II. Theory and therapy. Arch Gen Psychiatry 10(6):561–571
Hofmann SG, Asmundson GJG, Beck AT (2013) The science of cognitive therapy. Behav Ther 44(2):199–212
Jelinek L, Van Quaquebeke N, Moritz S (2017) Cognitive and metacognitive mechanisms of change in metacognitive training for depression. Sci Rep 7(1):3449
Kazdin AE (2007) Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol 3(1):1–27
Miegel F, Cludius B, Hottenrott B, Demiralay C, Sure A, Jelinek L (2019) Session-specific effects of the Metacognitive Training for Obsessive-Compulsive Disorder (MCT-OCD). Psychother Res 30:1–13
Miegel F, Cludius B, Hottenrott B, Demiralay C, Jelinek L (2020) Session-specific effects of the Metacognitive Group Training for Obsessive-Compulsive Disorder: significant results for thought control. Sci Rep 10(1):17816
Schneider BC, Cludius B, Lutz W, Moritz S, Rubel J (2018) An investigation of module-specific effects of metacognitive training for psychosis. Z Psychol. https://doi.org/10.1027/2151-2604/a000336
Miegel F, Peth J, Rubel J, Runde A, Arlt S, Gallinat J et al. (2022) Session-specific effects on suicidality in group therapy: no evidence for contagion. Arch Suicide Res 1–14. https://doi.org/10.1080/13811118.2021.2022051
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9. J Gen Intern Med 16(9):606–613
Dietrichkeit M, Hagemann-Goebel M, Nestoriuc Y, Moritz S, Jelinek L (2021) Side effects of the metacognitive training for depression compared to a cognitive remediation training in patients with depression. Sci Rep 11(1):1–10
Hautzinger M, Keller F, Kühner C (2006) Beck Depressions-Inventar (BDI-II). Revision. Resport Psychol 3:301–302
Beck AT, Steer RA, Brown GK (1996) Beck Depression Inventory. Second edition. Manual. The Psychological Corporation, San Antonio
IBM Corp (2017) IBM SPSS Statistics for Windows
R Core Team (2020) R: a language and environment for statistical computing. Austria; [cited 2018 May 29]. Available from: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006
Tibshirani R (2011) Regression shrinkage and selection via the lasso: a retrospective. J R Stat Soc Ser B (Stat Methodol) 73(3):273–282
Schwartz B, Cohen ZD, Rubel JA, Zimmermann D, Wittmann WW, Lutz W (2021) Personalized treatment selection in routine care: integrating machine learning and statistical algorithms to recommend cognitive behavioral or psychodynamic therapy. Psychother Res 31(1):33–51
Stekhoven DJ (2012) Using the missForest package. missForest nonparametric missing value input using random for R package version 12. Pp 1–11
Jelinek L, Faissner M, Moritz S, Kriston L (2018) Long-term efficacy of Metacognitive Training for Depression (DMCT): a randomized controlled trial. Br J Clin Psychol 58(3):bjc.12213
Jelinek L, Zielke L, Hottenrott B, Miegel F, Cludius B, Sure A et al (2018) Patients’ perspectives on treatment with metacognitive training for OCD: feasibility and acceptability. Zeitschrift fur Neuropsychol 29(1):20–28
Burlingame GM (2018) Cohesion in group therapy: a meta-analysis. Psychotherapy 55(4):384–398
Moritz S, Thoering T, Kühn S, Willenborg B, Westermann S, Nagel M (2015) Metacognition-augmented cognitive remediation training reduces jumping to conclusions and overconfidence but not neurocognitive deficits in psychosis. Front Psychol 6:1048
Moritz S, Stojisavlevic M, Göritz AS, Riehle M, Scheunemann J (2019) Does uncertainty breed conviction? On the possible role of compensatory conviction in jumping to conclusions and overconfidence in psychosis. Cogn Neuropsychiatry 24(4):284–299
Zwick JC, Wolkenstein L (2017) Facial emotion recognition, theory of mind and the role of facial mimicry in depression. J Affect Disord 210:90–99
Acknowledgements
We thank Sophie Banasiak, Judith Oehme, Frederica Wallraf, and Kathrin Simon-Kutscher for their help with recruitment for the RCT.
Funding
The RCT was financed by the Asklepios-Kliniken Hamburg GmbH’s internal research funding.
Author information
Authors and Affiliations
Contributions
LJ conducted the pilot study, and LJ and MHG designed the RCT, wrote the protocol, and acquired the funding. MD and MHG conducted the RCT, and FM and JR conducted the statistical analysis. JS and AB helped with the statistical analyses. AY helped with writing the introduction. FM wrote the first draft of the manuscript; all authors edited the manuscript. All authors substantially contributed to and have approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
Metacognitive Training for Depression was developed by one of the authors (LJ). JS and FM are paid to give workshops on metacognitive training.
Consent to participate
All participants gave written informed consent for participation.
Consent for publication
All participants consented to publish their data.
Ethics approval
The study was approved by the ethics committee of the German Psychological Association (Deutsche Gesellschaft für Psychologie).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miegel, F., Rubel, J., Dietrichkeit, M. et al. Exploring mechanisms of change in the metacognitive training for depression. Eur Arch Psychiatry Clin Neurosci 274, 739–753 (2024). https://doi.org/10.1007/s00406-023-01604-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-023-01604-y