Abstract
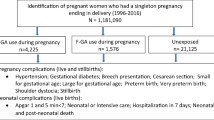
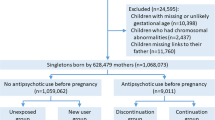
Despite growing concern about reproductive safety of antipsychotics, there is a paucity of research specifically assessing prenatal antipsychotic prescribing practices for psychotic disorders. This population-based cohort study identified women aged 15–50 years with diagnosis of psychotic disorders, who delivered their first and singleton child between 2003–2018 in Hong Kong, with an aim to examine temporal trends and predictors of prenatal antipsychotic use as well as antipsychotic utilization patterns before and during pregnancy. Data were retrieved from territory-wide medical-record database of public healthcare services. Of 804 women, 519 (65%) redeemed at least one prescription for antipsychotics during pregnancy. Older age at conception (25–34 years: OR 2.12 [95% CI 1.22–3.67]; 35–50 years: 2.52 [1.38–4.61]; 15–24 years as reference category) and antipsychotic treatment within 12 months pre-pregnancy (24.22 [16.23–36.16]) were significantly associated with prenatal antipsychotic use. Second-generation-antipsychotic (SGA) use during pregnancy increased over 16-year study period, while prenatal first-generation-antipsychotic (FGA) use showed declining trend. Overall antipsychotic and SGA use progressively decreased across pre-pregnancy and trimesters of pregnancy. Further analyses on antipsychotic use trajectories revealed that 87.4% (n = 459) of 529 women receiving antipsychotics in 12-month pre-pregnancy redeemed antipsychotic prescription during pregnancy, and 63.4% (n = 333) continued antipsychotic treatment throughout pregnancy. Only 7.5% of the cohort (n = 60) commenced antipsychotics in pregnancy. This is one of the few studies evaluating real-world prenatal antipsychotic utilization among women with psychotic disorders. Future research delineating risk conferred by illness-related factors and antipsychotic exposure on adverse maternal and fetal outcomes is warranted to facilitate treatment guideline development.


Similar content being viewed by others
References
Perala J, Suvisaari J, Saarni SI et al (2007) Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry 64:19–28
Chang WC, Wong CSM, Chen EYH et al (2017) Lifetime prevalence and correlates of schizophrenia-spectrum, affective, and other non-affective psychotic disorders in the Chinese adult population. Schizophr Bull 43:1280–1290
Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386:743–800
Palmer BA, Pankratz VS, Bostwick JM (2005) The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 62:247–253
Stubbs B, Koyanagi A, Veronese N et al (2016) Physical multimorbidity and psychosis: Comprehensive cross-sectional analysis including 242,952 people across 48 low- and middle-income countries. BMC Med 14:189
Oakley P, Kisely S, Baxter A et al (2018) Increased mortality among people with schizophrenia and other non-affective psychotic disorders in the community: a systematic review and meta-analysis. J Psychiatr Res 102:245–253
Taylor CL, Munk-Olsen T, Howard LM, Vigod SN (2020) Schizophrenia around the time of pregnancy” leveraging population-based health data and electronic health record data to fill knowledge gaps. BJPsych Open 6:e97
Breadon C, Kulkarni J (2019) An update on medication management of women with schizophrenia in pregnancy. Expert Opin Pharmacother 20:1365–1376
Dazzan P (2021) Schizophrenia during pregnancy. Curr Opin Psychiatry 34:238–244
Damkier P, Videbech P (2018) The safety of second-generation antipsychotics during pregnancy: a clinically focused review. CNS Drugs 32:351–366
Kucukgoncu S, Guloksuz S, Celik K et al (2020) Antipsychotic exposure in pregnancy and the risk of gestational diabetes: a systematic review and meta-analysis. Schizophr Bull 46:311–318
Viguera AC, Freeman MP, Góez-Mogollón L et al (2021) Reproductive safety of second-generation antipsychotics: updated data from the Massachusetts General Hospital National Pregnancy Registry for atypical antipsychotics. J Clin Psychiatry 82:20m13745
Wang Z, Brauer R, Man KKC, Alfageh B, Mongkhon P, Wong ICK (2021) Prenatal exposure to antipsychotic agents and the risk of congenital malformations in children: a systematic review and meta-analysis. Br J Clin Pharmacol 87:4101–4123
Huybrechts KF, Hernández-Díaz S, Patorno E et al (2016) Antipsychotic use in pregnancy and the risk for congenital malformations. JAMA Psychiat 73:938–946
Ellfolk M, Leinonen MK, Gissler M, Kiuru-Kuhlefelt S, Saastamoinen L, Malm H (2021) Second-generation antipsychotic use during pregnancy and risk of congenital malformations. Eur J Clin Pharmacol 77:1737–1745
Poels EMP, Schrijver L, Kamperman AM et al (2018) Long-term neurodevelopmental consequences of intrauterine exposure to lithium and antipsychotics: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry 27:1209–1230
Jablensky AV, Morgan V, Zubrick SR, Bower C, Yellachich L (2005) Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatry 162:79–81
Vigod SN, Kurdyak PA, Dennis CL et al (2014) Maternal and newborn outcomes among women with schizophrenia: a retrospective population-based cohort study. BJOG 121:566–574
Simoila L, Isometsä E, Gissler M, Suvisaari J, Halmesmäki E, Lindberg N (2018) Obstetric and perinatal health outcomes related to schizophrenia: a national register-based follow-up study among Finnish women born between 1965 and 1980 and their offspring. Eur Psychiatry 52:68–72
Gentile S, Fusco ML (2019) Schizophrenia and motherhood. Psychiatry Clin Neurosci 73:376–385
Petersen I, McCrea RL, Osborn DJP et al (2014) Discontinuation of antipsychotic medication in pregnancy: a cohort study. Schizophr Res 159:218–225
Taylor CL, Stewart R, Ogden J, Broadbent M, Pasupathy D, Howard LM (2015) The characteristics and health needs of pregnant women with schizophrenia compared with bipolar disorder and affective psychoses. BMC Psychiatry 15:88
Tosato S, Albert U, Tomassi S et al (2017) A systematized review of atypical antipsychotics in pregnant women: balancing between risks of untreated illness and risks of drug-related adverse effects. J Clin Psychiatry 78:e477–e489
Taylor CL, Broadbent M, Khondoker M, Stewart RJ, Howard LM (2018) Predictors of severe relapse in pregnant women with psychotic or bipolar disorders. J Psychiatr Res 104:100–107
Epstein RA, Bobo WV, Shelton RC et al (2013) Increasing use of atypical antipsychotics and anticonvulsants during pregnancy. Pharmacoepidemiol Drug Saf 22:794–801
Toh S, Li Q, Craig T et al (2013) Prevalence and trends in the use of antipsychotic medications during pregnancy in the U.S., 2001–2007: a population-based study of 585,615 deliveries. Arch Women Ment Health 16:149–157
Margulis AV, Kang EM, Hammad TA (2014) Patterns of prescription of antidepressants and antipsychotics across and within pregnancies in a population-based UK cohort. Matern Child Health J 18:1742–1752
Park Y, Huybrechts KF, Cohen JM et al (2017) Antipsychotic medication use among publicly insured pregnant women in the United States. Psychiatr Serv 68:1112–1119
Schaffer AL, Zoega H, Tran DT, Buckley NA, Pearson S, Havard A (2019) Trajectories of antipsychotic use before and during pregnancy and associated maternal and birth characteristics. Aust N Z J Psychiatry 53:1208–1221
Reutfors J, Cesta CE, Cohen JM et al (2020) Antipsychotic drug use in pregnancy: a multinational study from ten countries. Schizophr Res 220:106–115
Galbally M, Frayne J, Watson SJ, Snellen M (2019) Psychopharmacological prescribing practices in pregnancy for women with severe mental illness: a multicenter study. Eur Neuropsychopharmacol 29:57–65
Hospital Authority Head Office IT Department (2003) Clinical data analysis & reporting system (CDARS) user’s manual, 2nd edn. Hong Kong Hospital Authority, Hong Kong, p 3
Cheung NT, Fung V, Wong WN et al (2007) Principles-based medical informatics for success–How Hong Kong built one of the world’s largest integrated longitudinal electronic patients records. Stud Health Technol Inform 129:307–310
Chang WC, Chan JKN, Wong CSM, Hai JSH, Or PCF, Chen EYH (2020) Mortality, revascularization and cardioprotective pharmacotherapy after acute coronary syndrome in patients with psychotic disorders: a population-based cohort study. Schizophr Bull 46:774–784
Yung NCL, Wong CSM, Chan JKN, Or PCF, Chen EYH, Chang WC (2020) Mortality in patients with schizophrenia admitted for incident ischemic stroke: a population-based cohort study. Eur Neuropsychopharmacol 31:152–157
Chan JKN, Wong CSM, Or PCF, Chen EYH, Chang WC (2021) Risk of mortality and complications in patients with schizophrenia and diabetes mellitus: a population-based cohort study. Br J Psychiatry 219:375–382
Yung NCL, Wong CSM, Chan JKN, Chen EYH, Chang WC (2021) Excess mortality and life-years lost in people with schizophrenia and other non-affective psychoses: an 11-year population-based cohort study. Schizophr Bull 47:474–484
Man KKC, Chan DW, Ip P et al (2017) Prenatal antidepressant use and risk of attention-deficit/hyperactivity disorder in offspring: population based cohort study. BMJ 357:j2350
Lao KSJ, Zhao J, Blais JE et al (2020) Antipsychotics and risk of neuroleptic malignant syndrome: a population-based cohort and case-crossover study. CNS Drugs 34:1165–1175
Chang WC, Pang SLK, Chung DWS, Chan SSM (2009) Five-year stability of ICD-10 diagnoses among Chinese patients presented with first-episode psychosis in Hong Kong. Schizophr Res 115:351–357
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD9-CM administrative databases. J Clin Epidemiol 45:613–619
IBM Corp. (2019) IBM SPSS statistics for windows, version 260. IBM Corp, Armonk, NY
Damkier P, Christensen LS, Broe A (2018) Patterns and predictors for prescription of psychotropics and mood-stabilizing antiepileptics during pregnancy in Denmark 2000–2016. Br J Clin Pharmacol 84:2651–2662
Xiang YT, Ungvari GS, Correll CU, Chiu HFK, Shinfuku N (2016) Trends in the access to and the use of antipsychotic medications and psychotropic co-treatments in Asian patients with schizophrenia. Epidemiol Psychiatr Sci 25:9–17
Hálfdánarson Ó, Zoëga H, Aagaard L et al (2017) International trends in antipsychotic use: a study in 16 countries, 2005–2014. Eur Neuropsychopharmcol 27:1064–1076
Højlund M, Pottegård A, Johnsen E et al (2019) Trends in utilization and dosing of antipsychotic drugs in Scandinavia: comparison of 2006 and 2016. Br J Clin Pharmacol 85:1598–1606
Leong C, Raymond C, Chateau D et al (2017) Psychotropic drug use before, during, and after pregnancy: a population-based study in a Canadian cohort (2001–2013). Can J Psychiatry 62:543–550
Vigod SN, Fung K, Amartey A et al (2020) Maternal schizophrenia and adverse birth outcomes: what mediates the risk? Soc Psychiatry Psychiatr Epidemiol 55:561–570
Acknowledgements
The study was supported by the Hong Kong Research Grants Council (grant number: 17127417). Additional financial support to undertake this research was provided by the State Key Laboratory of Brain & Cognitive Sciences, the University of Hong Kong. The authors would like to thank the colleagues in Hospital Authority for their kind assistance in data retrieval for the current investigation.
Author information
Authors and Affiliations
Contributions
Authors WCC, CSMW and JKNC designed and conceptualized the study. Author JWYL and JKNC conducted statistical analysis and wrote the first draft of the manuscript. Authors WCC, JWYL, JKNC, and CSMW interpreted the study data. Author WCC revised and finalized the manuscript. All authors provided critical feedback to the manuscript and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Law, J.W.Y., Chan, J.K.N., Wong, C.S.M. et al. Antipsychotic utilization patterns in pregnant women with psychotic disorders: a 16-year population-based cohort study. Eur Arch Psychiatry Clin Neurosci 273, 901–909 (2023). https://doi.org/10.1007/s00406-022-01453-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-022-01453-1