Abstract
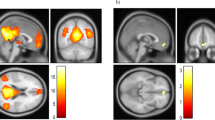
Empathy is the ability to generate emotional responses (i.e., cognitive empathy) and to make cognitive inferences (i.e., affective empathy) to other people’s emotions. Empirical evidence suggests that patients with bipolar disorder (BD) exhibit impairment in cognitive empathy, but findings on affective empathy are inconsistent. Few studies have examined the neural mechanisms of cognitive and affective empathy in patients with BD. In this study, we examined the empathy-related resting-state functional connectivity (rsFC) in BD patients. Thirty-seven patients with BD and 42 healthy controls completed the self-report Questionnaires of Cognitive and Affective Empathy (QCAE), the Yoni behavioural task, and resting-sate fMRI brain scans. Group comparison of empathic ability was conducted. The interactions between group and empathic ability on seed-based whole brain rsFC were examined. BD patients scored lower on the Online Simulation subscale of the QCAE and showed positive correlations between cognitive empathy and the rsFC of the dorsal Medial Prefrontal Cortex (dmPFC) with the lingual gyrus. The correlations between cognitive empathy and the rsFC of the temporal–parietal junction (TPJ) with the fusiform gyrus, the cerebellum and the parahippocampus were weaker in BD patients than that in healthy controls. These findings highlight the underlying neural mechanisms of empathy impairments in BD patients.



Similar content being viewed by others
References
World-Health-Organization (1993) The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization
Vazquez GH, Holtzman JN, Lolich M et al (2015) Recurrence rates in bipolar disorder: systematic comparison of long-term prospective, naturalistic studies versus randomized controlled trials. Eur Neuropsychopharmacol 25:1501–1512
Vlad M, Raucher-Chene D, Henry A, Kaladjian A (2018) Functional outcome and social cognition in bipolar disorder: is there a connection? Eur Psychiatry 52:116–125
Bio DS, Soeiro-de-Souza MG, Otaduy MCG et al (2013) The impact of limbic system morphology on facial emotion recognition in bipolar I disorder and healthy controls. Neuropsychiatr Dis Treat 9:743
Moreno-Manso JM, García-Baamonde ME, Blázquez-Alonso M et al (2018) Empathy and coping strategies in youths subject to protection measures. Child Youth Serv Rev 93:100–107
Reniers RLEP, Corcoran R, Drake R et al (2011) The QCAE: a questionnaire of cognitive and affective empathy. J Pers Assess 93:84–95
Shamay-Tsoory SG, Harari H, Aharon-Peretz J, Levkovitz Y (2010) The role of the orbitofrontal cortex in affective theory of mind deficits in criminal offenders with psychopathic tendencies. Cortex 46:668–677
Inoue Y, KkS Y (2006) Deficit in theory of mind is a risk for relapse of major depression. J Affect Disord 95:125–127
Haroa JM, Gonzalez-Pinto A, Novick D et al (2011) 2-year course of bipolar disorder type I patients in outpatient care: factors associated with remission and functional recovery. Eur Neuropsychopharmacol 21:287–293
Bora E, Bartholomeusz C, Pantelis C (2016) Meta-analysis of Theory of mind (ToM) impairment in bipolar disorder. Psychol Med 46:253–264
Lysaker PH, Irarrázaval L, Gagen EC et al (2018) Metacognition in schizophrenia disorders: comparisons with community controls and bipolar disorder: replication with a Spanish language Chilean sample. Psychiatry Res 267:528–534
Shamay-Tsoory SG, Harari OH, Levkovitz Y (2009) Neuropsychological evidence of impaired cognitive empathy in euthymic bipolar disorder. J Neuropsychiatry Clin Neurosci 21:59–67
Derntl B, Seidel E-M, Schneider F, Habel U (2012) How specific are emotional deficits? A comparison of empathic abilities in schizophrenia, bipolar and depressed patients. Schizophr Res 142:58–64
Fan Y, Duncan NW, De GM, Northoff G (2011) Is there a core neural network in empathy? An fMRI based quantitative meta-analysis. Neurosci Biobehav Rev 35:903–911
Danilo B, Leonhard S, Kai V et al (2012) Parsing the neural correlates of moral cognition: ALE meta-analysis on morality, theory of mind, and empathy. Brain Struct Funct 217:783–796
Baron-Cohen S, Ring HA, Wheelwright S et al (2010) Social intelligence in the normal and autistic brain: an fMRI study. Eur J Neurosci 11:1891–1898
Schurz M, Radua J, Aichhorn M et al (2014) Fractionating theory of mind: a meta-analysis of functional brain imaging studies. Neurosci Biobehav Rev 42:9–34
Kim S, Kim S, Kim H et al (2017) Altered functional connectivity of the default mode network in low-empathy subjects. Yonsei Med J 58:1061–1065
Takeuchi H, Taki Y, Rui N et al (2014) Association between resting-state functional connectivity and empathizing/systemizing. Neuroimage 99:312–322
Cox CL, Uddin LQ, Di MA et al (2012) The balance between feeling and knowing: affective and cognitive empathy are reflected in the brain’s intrinsic functional dynamics. Soc Cogn Affect Neurosci 7:727
Kim E, Jung Y, Ku J et al (2009) Reduced activation in the mirror neuron system during a virtual social cognition task in euthymic bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 33:1409–1416
Willert A, Mohnke S, Erk S et al (2016) Alterations in neural theory of mind processing in euthymic patients with bipolar disorder and unaffected relatives. Bipolar Disord 17:880–891
Lahera G, Herrera S, Reinares M et al (2015) Hostile attributions in bipolar disorder and schizophrenia contribute to poor social functioning. Acta Psychiatr Scand 131:472–482
Si T, Liang S, Dang W et al (2009) Evaluation of the reliability and validity of Chinese version of the mini-international neuropsychiatric interview in patients with mental disorders. Chinese Ment Heal J 23:397–493
Liang Y, Yang H, Ma Y et al (2019) Validation and extension of the questionnaire of cognitive and affective empathy in the Chinese setting. PsyCh J 8:439–448
Shamay-Tsoory SG, Shur S, Barcai-Goodman L et al (2007) Dissociation of cognitive from affective components of theory of mind in schizophrenia. Psychiatry Res 149:11–23
Zhang Q, Li X, Parker GJ et al (2016) Theory of mind correlates with clinical insight but not cognitive insight in patients with schizophrenia. Psychiatry Res Neuroimaging 237:188–195
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435
Gong YX (1992) Manual of Wechsler Adult Intelligence Scale-Chinese Version. Chinese Map, Changsha
Yan CG, Di WX, Zuo XN, Zang YF (2016) DPABI: data processing and analysis for (Resting-State) brain imaging. Neuroinformatics 14:339–351
Power JD, Barnes KA, Snyder AZ et al (2012) Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. Neuroimage 59:2142–2154
Friston KJ, Williams S, Howard R et al (1996) Movement-related effects in fMRI time-series. Magn Reson Med 35:346–355
Ashburner J (2007) A fast diffeomorphic image registration algorithm. Neuroimage 38:95–113
Andrewshanna JR, Reidler JS, Sepulcre J et al (2010) Functional-anatomic fractionation of the brain’s default network. Neuron 65:550–562
Fusar-Poli P, Placentino A, Carletti F et al (2009) Laterality effect on emotional faces processing: ALE meta-analysis of evidence. Neurosci Lett 452:262–267
Kim S, Kim J, Kim J et al (2007) The neural mechanism of imagining facial affective expression. Brain Res 1145:128–137
Lee J, Choi S, Kang J et al (2017) Structural characteristics of the brain reward circuit regions in patients with bipolar I disorder: a voxel-based morphometric study. Psychiatry Res Neuroimaging 269:82–89
Usnich T, Spengler S, Sajonz B et al (2015) Perception of social stimuli in mania: an fMRI study. Psychiatry Res Neuroimaging 231:71–76
Müller VI, Höhner Y, Eickhoff SB (2018) Influence of task instructions and stimuli on the neural network of face processing: an ALE meta-analysis. Cortex 103:240–255
Van OF, Baetens K, Mariën P, Vandekerckhove M (2014) Social cognition and the cerebellum: a meta-analysis of over 350 fMRI studies. Neuroimage 86:554–572
Van OF, Mariën P (2016) Functional connectivity between the cerebrum and cerebellum in social cognition: a multi-study analysis. Neuroimage 124:248–255
Van OF, Van de Steen F, van Dun K, Heleven E (2020) Connectivity between the cerebrum and cerebellum during social and non-social sequencing using dynamic causal modelling. Neuroimage 206:116326
Kim H (2016) Default network activation during episodic and semantic memory retrieval: a selective meta-analytic comparison. Neuropsychologia 80:35–46
Shamay-Tsoory SG, Judith AP, Daniella P (2009) Two systems for empathy: a double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain A J Neurol 132:617
Arnone D, Cavanagh J, Gerber D et al (2009) Magnetic resonance imaging studies in bipolar disorder and schizophrenia: meta-analysis. Br J Psychiatry 195:194–201
Yucel K, McKinnon MC, Taylor VH et al (2007) Bilateral hippocampal volume increases after long-term lithium treatment in patients with bipolar disorder: a longitudinal MRI study. Psychopharmacology 195:357–367
Bodnar A, Rybakowski JK (2017) Increased affective empathy in bipolar patients during a manic episode. Rev Bras Psiquiatr 39:342–345
Liang Y, Yang H, Zhang Y et al (2020) Validation of the questionnaire of cognitive and affective empathy in patients with schizophrenia, major depressive disorder and bipolar disorder. Cogn Neuropsychiatry 25:466–479
Acknowledgements
This study was supported by grants from Beijing Municipal Science & Technology Commission Grant (Z161100000216138), Beijing Training Project for the Leading Talents in Science and Technology (Z151100000315020), Beijing Municipal Science and Technology Commission (Z171100001017086), National Natural Science Foundation of China (31871114; 31400884), and the CAS Key Laboratory of Mental Health, Institute of Psychology. These funding agents had no further role in the study design; in the collection, analysis and interpretation of the data; in the writing of the manuscript; and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
YL collected and analyzed the data, and wrote up the draft of the manuscript. SZ was responsible for imaging data protocol, collection and quality control, helped analyzed the data and interpreted the findings and commented the draft critically. YZ and XC collected data and implanted test, and commented on the manuscript critically. YW designed the study, contributed to imaging data analysis, quality control, interpreted the findings and commented critically on the manuscript. YM contributed to the funding sources, monitoring the clinical data quality, interpreted the findings and commented on the manuscript critically. EC, SL, KM and XY interpreted the findings and commented on the manuscript critically. RC generated the idea and designed the study, interpreted the findings and commented on the manuscript critically. All authors commented on the manuscript and agreed to the final submission.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared that there are no conflicts of interest in relation to the subject of this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liang, Ys., Zhou, Sz., Zhang, Yj. et al. Altered empathy-related resting-state functional connectivity in patients with bipolar disorder. Eur Arch Psychiatry Clin Neurosci 272, 839–848 (2022). https://doi.org/10.1007/s00406-021-01305-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-021-01305-4