Abstract
Objective
To compare clinical traits of suicidal vulnerability among in-patients with suicidal behavior disorder (SBD) with and without borderline personality disorder (BPD).
Method
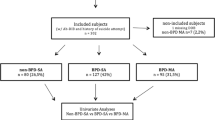
we recruited adult patients with SBD, consecutively and voluntarily hospitalized in a specialized unit for affective disorders and suicidal behavior between July and October 2016. Ninety-two inpatients having attempted suicide within the past 2 years were divided into two subgroups according to the presence or absence of BPD. Clinical vulnerability traits for suicidal behavior were assessed.
Results
Half of the patients with SBD also had BPD. Patients with BPD were nine times more likely to be major suicide repeaters compared to those without. They were also more likely to display clinical and psychological vulnerability traits for suicidal behavior, even after considering potential confounders. Emotional dysregulation, shame-proneness, impulsiveness, preoccupied attachment pattern, and childhood trauma were high in both groups, but significantly increased in those with (vs. without) BPD status. Psychological traits remained stable in SBD-BPD patients, regardless of the time since the last suicide attempt (i.e. SBD in recent vs. early remission).
Conclusions
Clinical and psychological traits associated with suicidal vulnerability are present in all SBD patients compared to non-suicidal populations, but comorbidity with BPD is associated with particularly high scores. BPD could be considered as a specifier for SBD diagnoses.
Similar content being viewed by others
References
World Health Organization: Preventing suicide: a global imperative. 2014
American Psychiatric Association: Diagnostic and statistical manual of mental disorders, fifth edition (dsm5). 2013
Courtet P, Gottesman II, Jollant F, Gould TD: The neuroscience of suicidal behaviors: What can we expect from endophenotype strategies? Transl Psychiatry 2011;1
Turecki G, Ernst C, Jollant F, Labonte B, Mechawar N (2012) The neurodevelopmental origins of suicidal behavior. Trends Neurosci 35:14–23
Kealy D, Ogrodniczuk JS, Rice SM, Oliffe JL (2017) Alexithymia, suicidal ideation and health-risk behaviours: a survey of canadian men. Int J Psychiatry Clin Pract 16:1–3
Hastings ME, Northman LM, Tangney JP:, Joiner T, Rudd MD (2000) Shame, guilt, and suicide. Suicide science: expanding the boundaries. Kluwer Academic Publishers, New York, pp 67–79
Milligan RJ, Andrews B (2005) Suicidal and other self-harming behaviour in offender women: The role of shame, anger and childhood abuse. Leg Criminol Psychol 10:13–25
Feiring C, Taska LS (2005) The persistence of shame following sexual abuse: a longitudinal look at risk and recovery. Child Maltreatment 4:337–349
Muzik M, Brier Z, Menke RA, Davis MT, Sexton MB (2016) Longitudinal suicidal ideation across 18-months postpartum in mothers with childhood maltreatment histories. J Affect Disord 1:138–145
Agrawal HR, Gunderson J, Holmes BM, Lyons-Ruth K (2004) Attachment studies with borderline patients: a review. Harv Rev Psychiatry 12:94–104
Oldham JM (2006) Borderline personality disorder and suicidality. Am J Psychiatry 163:20–26
Rogers ML, Joiner TE Jr (2016) Borderline personality disorder diagnostic criteria as risk factors for suicidal behavior through the lens of the interpersonal theory of suicide. Arch Suicide Res 20:591–604
Scott LN, Kim Y, Nolf KA, Hallquist MN, Wright AG, Stepp SD, Morse JQ, Pilkonis PA (2013) Preoccupied attachment and emotional dysregulation: Specific aspects of borderline personality disorder or general dimensions of personality pathology? J Pers Disord 27:473–495
Linehan MM (1993) Cognitive-behavioral treatment of borderline personality disorder. Guilford, New York
Westphal M, Olfson M, Bravova M, Gameroff MJ, Gross R, Wickramaratne P, Pilowsky DJ, Neugebauer R, Shea S, Lantigua R, Weissman M, Neria Y (2013) Borderline personality disorder, exposure to interpersonal trauma, and psychiatric comorbidity in urban primary care patients. Psychiatry 76:365–380
Bouvard M, Fontaine-Buffe M, Cungi C, Adeleine P, Chapoutier C, Durafour E, Bouchard C, Cottraux J (1999) Preliminary studies of the structured diagnostic interview for personality disorders. SCID II. Encephale 25:416–421
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The mini-international neuropsychiatric interview (m.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for dsm-iv and icd-10. J Clin Psychiatry 59(Suppl 20):22–33;quiz 34–57
Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, Janavs J, Dunbar GC (1997) The mini international neuropsychiatric interview (mini). A short diagnostic structured interview: reliability and validity according to the cidi. Eur Psychiatry 12:224–231
Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ (2011) The columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 168:1266–1277
Posner K. The columbia lighthouse project.
Mann JJ (1998) The neurobiology of suicide. Nat Med 4:25–30
Blasco-Fontecilla H, Fernandez-Fernandez R, Colino L, Fajardo L, Perteguer-Barrio R, de Leon J (2016) The addictive model of self-harming (non-suicidal and suicidal) behavior. Front Psychiatry 7:8
Asberg M, Traskman L, Thoren P (1976) 5-hiaa in the cerebrospinal fluid. A biochemical suicide predictor? Arch Gen Psychiatry 33:1193–1197
Giner L, Jaussent I, Olie E, Beziat S, Guillaume S, Baca-Garcia E, Lopez-Castroman J, Courtet P (2014) Violent and serious suicide attempters: one step closer to suicide? J Clin Psychiatry 75:e191–e197
Gratz KL, Roemer LR (2004) Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 26:41–54
Dan-Glauser ES, Scherer KR (2013) The difficulties in emotion regulation scale (ders): factor structure and consistency of a french translation. Swiss J Psychol 72:5–11
Tangney JP, Dearing RL, Wagner PE, Gramzow R (2000) The test of self-conscious affect-3 (tosca-3)
Nugier A, Gil S, Chekroun P (2012) Validation of the french version of the test of self-conscious affect-3 (tosca-3): a measure for the tendencies to feel ashamed and guilty. Revue européenne de psychologie appliquée 62:19–27
Rusch N, Lieb K, Gottler I, Hermann C, Schramm E, Richter H, Jacob GA, Corrigan PW, Bohus M (2007) Shame and implicit self-concept in women with borderline personality disorder. Am J Psychiatry 164:500–508
Lester D (1997) The role of shame in suicide. Suicide life-threatening behavior 27:352–361
Billieux J, Rochat L, Ceschi G, Carre A, Offerlin-Meyer I, Defeldre AC, Khazaal Y, Besche-Richard C, Van der Linden M (2012) Validation of a short french version of the upps-p impulsive behavior scale. Compr Psychiatry 53:609–615
Billieux J, Rochat L, Ceschi G, Carré A, Offerlin-Meyer I, Defeldre AC, Khazaal Y, Besche-Richard C, Van der Linden M (2012) Validation of a short french version of the upps-p impulsive behavior scale. Compr Psychiatry 53:609–615
Guédeney N, Fermanian J, Bifulco A (2010) La version franc¸aise du relationship scales questionnaire de bartholomew (rsq, questionnaire des échelles de relation): Étude de validation du construit. L’Encephale 36:69–76
Bernstein DP, Fink L (1998) Childhood trauma questionnaire: a retrospective self-report manual. The Psychological Corporation, San Antonio
Paquette D, Laporte L, Bigras M, Zoccolillo M (2004) Validation of the french version of the ctq and prevalence of the history of maltreatment. Sante Ment Que 29:201–220
Blasco-Fontecilla H, Baca-Garcia E, Courtet P, Garcia Nieto R, de Leon J (2015) Horror vacui: Emptiness might distinguish between major suicide repeaters and nonmajor suicide repeaters: a pilot study. Psychother Psychosom 84:117–119
Weintraub MJ, Van de Loo MM, Gitlin MJ, Miklowitz DJ (2017) Self-harm, affective traits, and psychosocial functioning in adults with depressive and bipolar disorders. J Nerv Ment Dis 205:896–899
Rajappa K, Gallagher M, Miranda R (2012) Emotion dysregulation and vulnerability to suicidal ideation and attempts. Cogn Ther Res 36:833–839
Arria AM, O’Grady KE, Caldeira KM, Vincent KB, Wilcox HC, Wish ED (2009) Suicide ideation among college students: a multivariate analysis. Arch Suicide Res 13:230–246
Anestis MD, Kleiman EM, Lavender JM, Tull MT, Gratz KL (2014) The pursuit of death versus escape from negative affect: an examination of the nature of the relationship between emotion dysregulation and both suicidal behavior and non-suicidal self-injury. Compr Psychiatry 55:1820–1830
Sleuwaegen E, Houben M, Claes L, Berens A, Sabbe B (2017) The relationship between non-suicidal self-injury and alexithymia in borderline personality disorder: “actions instead of words”. Compr Psychiatry 77:80–88
Rogers ML, Kelliher-Rabon J, Hagan CR, Hirsch JK, Joiner TE (2017) Negative emotions in veterans relate to suicide risk through feelings of perceived burdensomeness and thwarted belongingness. J Affect Disord 208:15–21
Oexle N, Rusch N, Viering S, Wyss C, Seifritz E, Xu Z, Kawohl W (2017) Self-stigma and suicidality: a longitudinal study. Eur Arch Psychiatry Clin Neurosci 267:359–361
Kiamanesh P, Dieserud G, Dyregrov K, Haavind H (2015) Maladaptive perfectionism: Understanding the psychological vulnerability to suicide in terms of developmental history. Omega (Westport) 71:126–145
Nathanson DL (1988) The many faces of shame, Guilford Press
Unoka Z, Vizin G (2017) To see in a mirror dimly. The looking glass self is self-shaming in borderline personality disorder. Psychiatry research
Rusch N, Corrigan PW, Bohus M, Jacob GA, Brueck R, Lieb K (2007) Measuring shame and guilt by self-report questionnaires: a validation study. Psychiatry Res 150:313–325
Brown MZ, Comtois KA, Linehan MM (2002) Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. J Abnorm Psychol 111:198–202
Nathanson DL (1994) Shame, compassion, and the “borderline” personality. Psychiatr Clin North Am 17:785–810
Wells GB, Hansen ND (2003) Lesbian shame: Its relationship to identity integration and attachment. J Homosex 45:93–110
Das P, Calhoun V, Malhi GS (2014) Bipolar and borderline patients display differential patterns of functional connectivity among resting state networks. Neuroimage 98:73–81
Bøen E, Hummelen B, Elvsåshagen T, Boye B, Andersson S, Karterud S, Malt UF (2015) Different impulsivity profiles in borderline personality disorder and bipolar ii disorder. J Affect Disord 1:104–111
Lopez-Castroman J, Jaussent I, Beziat S, Guillaume S, Baca-Garcia E, Genty C, Olié E, Courtet P (2014) Increased severity of suicidal behavior in impulsive aggressive patients exposed to familial adversities. Psychol Med 44:3059–3068
Bach B, Fjeldsted R (2017) The role of dsm-5 borderline personality symptomatology and traits in the link between childhood trauma and suicidal risk in psychiatric patients. Borderline Personal Disord Emot Dysregul 18:12
Teicher MH, Samson JA, Anderson CM, Ohashi K: The effects of childhood maltreatment on brain structure, function and connectivity. Nature reviews 2016:653
Levy KN (2005) The implications of attachment theory and research for understanding borderline personality disorder. Dev Psychopathol 959–986
Widom CS, Czaja SJ, Kozakowski SS, Chauhan P (2018) Does adult attachment style mediate the relationship between childhood maltreatment and mental and physical health outcomes? Child Abuse Negl 76:533–545
Zanarini MC (2000) Childhood experiences associated with the development of borderline personality disorder. Psychiatr Clin N Am 23:89–101
Gunderson JG (2007) Disturbed relationships as a phenotype for borderline personality disorder. Am J Psychiatry 164:1637–1640
Insel TR (2003) Is social attachment an addictive disorder? Physiol Behav 79:351–357
SAHDRA BK, SHAVER PR, BROWN KW (2010) A scale to measure nonattachment: a buddhist complement to western research on attachment and adaptive functioning. J Pers Assess 92:116–127
Stanley B, Siever LJ (2010) The interpersonal dimension of borderline personality disorder: Toward a neuropeptide model. Am J Psychiatry 167:24–39
HC (2007) K: Dsm categories and dimensions in clinical and research contexts. Int J Methods Psychiatr Res 16(Suppl 1):S8–S15
Craske MG (2012) The r-doc initiative: Science and practice. Depress Anxiety 29:253–256
Bender R, Lange S (2001) Adjusting for multiple testing—when and how? J Clin Epidemiol 54:343–349
Acknowledgements
The authors thank Andrew Porter (English native speaker), and Elisabetta Andermarcher (MD, PhD, medical writer), for their careful reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declares conflicts of interest related to this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ducasse, D., Lopez-Castroman, J., Dassa, D. et al. Exploring the boundaries between borderline personality disorder and suicidal behavior disorder. Eur Arch Psychiatry Clin Neurosci 270, 959–967 (2020). https://doi.org/10.1007/s00406-019-00980-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-00980-8