Abstract
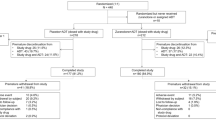
Given that antidepressants (ADs) work slowly, there is interest in means to accelerate their therapeutic effect and to reduce side effects. In this regard, thiamine (vitamin B1) is attracting growing interest. Thiamine is an essential nutrient, while thiamine deficiency leads to a broad variety of disorders including irritability and symptoms of depression. Here, we tested the hypothesis that adjuvant thiamine would reduce depression, compared to placebo. A total of 51 inpatients (mean age: 35.2 years; 53 % females) with MDD (Hamilton Depression Rating Scale score (HDRS) at baseline: >24) took part in the study. A standardized treatment with SSRI was introduced and kept at therapeutic levels throughout the study. Patients were randomly assigned either to the thiamine or the placebo condition. Experts rated (HDRS) symptoms of depression at baseline, and after 3, 6, and 12 weeks (end of the study). Between baseline and the end of the study, depression had reduced in both groups. Compared to placebo, adjuvant thiamine improved symptoms of depression after 6 week of treatment, and improvements remained fairly stable until the end of the study, though mean differences at week 12 were not statistically significant anymore. No adverse side effects were reported in either group. Results suggest that among younger patients with MDD adjuvant thiamine alleviated symptoms of depression faster compared to placebo. Importantly, improvements were observed within 6 weeks of initiation of treatment. Thus, thiamine might have the potential to counteract the time lag in the antidepressant effects of ADs.

Similar content being viewed by others
References
Adler AD, Strunk DR, Fazio RH (2015) What changes in cognitive therapy for depression? An examination of cognitive therapy skills and maladaptive beliefs. Behav Ther 46:96–109
Akhondzadeh S, Gerbarg PL, Brown RP (2013) Nutrients for prevention and treatment of mental health disorders. Psychiatr Clin North Am 36:25–36
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Publishing, Arlington
Bauer M, Pfennig A, Severus E, Whybrow PC, Angst J, Möller HJ, World Federation of Societies of Biological Psychiatry (2013) Task Force on unipolar depressive disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: update 2013 on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry 14:334–385
Bauer M, Severus E, Köhler S, Whybrow PC, Angst J, Möller HJ, Wfsbp Task Force on Treatment Guidelines for Unipolar Depressive Disorders (2015) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders. Part 2: maintenance treatment of major depressive disorder-update. World J Biol Psychiatry 16:76–95
Benton D, Griffiths R, Haller J (1997) Thiamine supplementation mood and cognitive functioning. Psychopharmacology 129:66–71
Biesheuvel-Leliefeld KE, Kok GD, Bockting CL, Cuijpers P, Hollon SD, van Marwijk HW, Smit F (2015) Effectiveness of psychological interventions in preventing recurrence of depressive disorder: meta-analysis and meta-regression. J Affect Disord 174:400–410
Bockting CL, Hollon SD, Jarrett RB, Kuyken W, Dobson K (2015) A lifetime approach to major depressive disorder: The contributions of psychological interventions in preventing relapse and recurrence. Clin Psychol Rev 41:16–26
Botez MI, Young SN (2001) Biogenic amine metabolites and thiamine in cerebrospinal fluid in heredo-degenerative ataxias. Can J Neurol Sci 28:134–140
Bourre JM (2006) Effects of nutrients (in food) on the structure and function of the nervous system: update on dietary requirements for brain. Part 1: micronutrients. J Nutr Health Aging 10:377–385
Bourre JM (2006) Effects of nutrients (in food) on the structure and function of the nervous system: update on dietary requirements for brain. Part 2: macronutrients. J Nutr Health Aging 10:386–399
Butterworth RF (1982) Neurotransmitter function in thiamine-deficiency encephalopathy. Neurochem Int 4:449–464
Carney MW, Williams DG, Sheffield BF (1979) Thiamine and pyridoxine lack newly-admitted psychiatric patients. Br J Psychiatry 135:249–254
Cassano P, Fava M (2002) Depression and public health e an overview. J Psychosom Res 53:849–857
Castrén E (2005) Is mood chemistry? Nat Rev Neurosci 6:241–246
Cooney G, Dwan K, Mead G (2014) Exercise for depression. JAMA 311(23):2432–2433
Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR et al (2013) Exercise for depression. Cochrane Database Syst Rev 9:CD004366
Cuijpers P (2015) Psychotherapies for adult depression: recent developments. Curr Opin Psychiatry 28:24–29
Delgado PL, Moreno FA (2000) Role of norepinephrine in depression. J Clin Psychiatry 61(Suppl 1):5–12
Dinan TG, Cryan JF (2013) Melancholic microbes: a link between gut microbiota and depression? Neurogastroenterol Motil 25:713–719
Dinan TG, Stanton C, Cryan JF (2013) Psychobiotics: a novel class of psychotropic. Biol Psychiatry 74:720–726
Dinan TG, Stilling RM, Stanton C, Cryan JF (2015) Collective unconscious: how gut microbes shape human behavior. J Psychiatr Res 63:1–9
Farnia V, Hojatitabar S, Shakeri J, Rezaei M, Yazdchi K, Bajoghli H, Holsboer-Trachsler E, Brand S (2015) Adjuvant Rosa Damascena has a small effect on SSRI-induced sexual dysfunction in female patients suffering from MDD. Pharmacopsychiatry 48:156–163
Farnia V, Shirzadifar M, Shakeri J, Rezaei M, Bajoghli H, Holsboer-Trachsler E, Brand S (2015) Rosa damascena oil improves SSRI-induced sexual dysfunction in male patients suffering from major depressive disorders: results from a double-blind, randomized, and placebo-controlled clinical trial. Neuropsychiatr Dis Treat 11:625–635
Gibson GE, Zhang H (2002) Interactions of oxidative stress with thiamine homeostasis promote neurodegeneration. Neurochem Int 40:493–504
Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK (2003) The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry 64:1465–1475
Haghighi M, Khodakarami S, Jahangard L, Ahmadpanah M, Bajoghli H, Holsboer-Trachsler E, Brand S (2014) In a randomized, double-blind clinical trial, adjuvant atorvastatin improved symptoms of depression and blood lipid values in patients suffering from severe major depressive disorder. J Psychiatr Res 58:109–114
Haghighi M, Salehi I, Erfani P, Jahangard L, Bajoghli H, Holsboer-Trachsler E, Brand S (2013) Additional ECT increases BDNF-levels in patients suffering from major depressive disorders compared to patients treated with citalopram only. J Psychiatr Res 47:908–915
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurgery Psychiatry 23:56–62
Hasler G (2010) Pathophysiology of depression: do we have any solid evidence of interest to clinicians? World Psychiatry 9:155–161
Himmerich H, Erbguth F (2014) Nutrition and dietary supplements in psychiatric diseases. Nervenarzt 85:1512–1520
Hinze-Selch D, Weber MM, Zimmermann U, Pollmächer T (2000) Thiamine treatment in psychiatry and neurology. Fortschr Neurol Psychiatr 68:113–120
Irwin SA, Iglewicz A (2010) Oral ketamine for the rapid treatment of depression and anxiety in patients receiving hospice care. J Palliat Med 13:903–908
Josefsson T, Lindwall M, Archer T (2014) Physical exercise in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports 24:259–272
Kato T, Kato N (2000) Mitochondrial dysfunction in bipolar disorder. Bipolar Disord 2:180–190
Ke Z-J, Gibson GE (2004) Selective response of various brain cell types during neurodegeneration induced by mild impairment of oxidative metabolism. Neurochem Int 45:361–369
Kellner CH, Greenberg RM, Murrough JW, Bryson EO, Briggs MC, Pasculli RM (2012) ECT in treatment-resistant depression. Am J Psychiatry 169:1238–1244
Lakhan SE, Vieira KF (2008) Nutritional therapies for mental disorders. Nutr J 7:2
Langlais PJ, Zhang SX, Savage LM (1996) Neuropathology of thiamine deficiency: an update on the comparative analysis of human disorders and experimental models. Metab Brain Dis 11:19–37
Lovato N, Gradisar M (2014) A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev 18:521–529
Luna RA, Foster JA (2015) Gut brain axis: diet microbiota interactions and implications for modulation of anxiety and depression. Curr Opin Biotechnol 32:35–41
Marcus M, Yasamy MT, van Ommeren M, Chisholm D, Saxena S (2012) WHO Department of mental health and substance abuse. Depression: a global public health concern. Geneva, Switzerland: World Health Organization. http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf. Accessed 15 Aug 2015
Mikoteit T, Beck J, Eckert A, Hemmeter U, Brand S, Bischof R, Holsboer-Trachsler E, Delini-Stula A (2014) High baseline BDNF serum levels and early psychopathological improvement are predictive of treatment outcome in major depression. Psychopharmacol (Berl) 231:2955–2965
Mota-Pereira J, Silverio J, Carvalho S, Ribeiro JC, Fonte D, Ramos J (2011) Moderate exercise improves depression parameters in treatment-resistant patients with major depressive disorder. J Psychiatr Res 45:1005–1011
Mura G, Moro MF, Patten SB, Carta MG (2014) Exercise as an add-on strategy for the treatment of major depressive disorder: a systematic review. CNS Spectr 19:496–508
Murray CJL, Lopez AD (1997) Global mortality, disability, and the contribution of risk factors: global burden of disease study. Lancet 349:1436–1442
Nardone R, Höller Y, Storti M, Christova M, Tezzon F, Golaszewski S, Trinka E, Brigo F (2013) Thiamine deficiency induced neurochemical, neuroanatomical, and neuropsychological alterations: a reappraisal. Sci World J 2013:309143
Ng TP, Feng L, Niti M, Kua EH, Yap KB (2009) Folate, vitamin B12, homocysteine, and depressive symptoms in a population sample of older Chinese adults. J Am Geriatr Soc 57:871–876
Paul IA, Skolnick P (2003) Glutamate and depression: clinical and preclinical studies. Ann N Y Acad Sci 1003:250–272
Penninx BW, Milaneschi Y, Lamers F, Vogelzangs N (2013) Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med 11:129
Pepersack T, Garbusinski J, Robberecht J, Beyer I, Willems D, Fuss M (1999) Clinical relevance of thiamine status amongst hospitalized elderly patients. Gerontology 45:96–101
Plaitakis A, Hwang EC, Woert MH, Szilagyi PE, Berl S (1982) Effect of thiamin deficiency on brain neurotransmitter systems. Ann N Y Acad Sci 378:367–381
Reichenpfader U, Gartlehner G, Morgan LC, Greenblatt A, Nussbaumer B, Hansen RA et al (2014) Sexual dysfunction associated with second-generation antidepressants in patients with major depressive disorder: results from a systematic review with network meta-analysis. Drug Saf 37:19–31
Salehi I, Hosseini SM, Haghighi M, Jahangard L, Bajoghli H, Gerber M et al (2014) Electroconvulsive therapy and aerobic exercise training increased BDNF and ameliorated depressive symptoms in patients suffering from treatment resistant major depressive disorder. J Psychiatr Res 57:117–124
Saltiel PF, Silvershein DI (2015) Major depressive disorder: mechanism-based prescribing for personalized medicine. Neuropsychiatr Dis Treat 11:875–888
Sapolsky RM (2000) The possibility of neurotoxicity in the hippocampus in major depression: a primer on neuron death. Biol Psychiatry 48:755–765
Singleton CK, Martin PR (2001) Molecular mechanisms of thiamine utilization. Curr Mol Med 1:197–207
Smidt LJ, Cremin FM, Grivetti LE, Clifford AJ (1991) Influence of thiamin supplementation on the health and general well-being of an elderly Irish population with marginal thiamin deficiency. J Gerontol 146:16–22
Stanton R, Reaburn P (2014) Exercise and the treatment of depression: a review of the exercise program variables. J Sci Med Sport 17:177–182
Vigil FA, Oliveira-Silva Ide F, Ferreira LF, Pereira SR, Ribeiro AM (2010) Spatial memory deficits and thalamic serotonergic metabolite change in thiamine deficient rats. Behav Brain Res 210:140–142
Wurtman RJ, Wurtman JJ (1995) Brain serotonin, carbohydrate-craving, obesity and depression. Obes Res 3(Suppl 4):S477–S480
Zempleni J, Rucker RB, McCormick DB, Suttie JW (2007) Handbook of vitamins, 4th edn. CRC Press, Boca Raton, pp 253–287
Zhang G, Ding H, Chen H, Ye X, Li H, Lin X, Ke Z (2013) Thiamine nutritional status and depressive symptoms are inversely associated among older Chinese adults. J Nutr 143:53–58
Acknowledgments
The present study is the doctoral thesis of Dr. Hassan Davari. We thank Nick Emler (University of Surrey, UK) for proofreading the manuscript.
Role of funding source
The entire study has been conducted without external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical statement
The Review Board of the Hamadan University of Medical Sciences (Hamadan, Iran) approved the study, which was performed in accordance with the ethical standards laid down in the Declaration of Helsinki. Patients were fully informed about the study aims and procedure, and about the confidential nature of data selection and data handling, and gave written informed consent.
Rights and permissions
About this article
Cite this article
Ghaleiha, A., Davari, H., Jahangard, L. et al. Adjuvant thiamine improved standard treatment in patients with major depressive disorder: results from a randomized, double-blind, and placebo-controlled clinical trial. Eur Arch Psychiatry Clin Neurosci 266, 695–702 (2016). https://doi.org/10.1007/s00406-016-0685-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-016-0685-6