Abstract
Purpose
Aim of this study was to calculate the percentage of the Automatic Speaking Valve (ASV) use in a large cohort of laryngectomized patients with voice prosthesis (VP) and to analyze the main reasons for non-use. Subsequently, a specific rehabilitation training was proposed.
Methods
One hundred-ten laryngectomized patients with VP were enrolled in the first phase of the study (census). Among them, 57 patients were included in the second phase (intervention), in which a training based on moving phonatory exercises was proposed. Structured questionnaires were used before and after training in order to investigate ASV use rate (days/week and hours/day; reasons for impeding the ASV use), average adhesive life-time during ASV use; hands-free speech duration; skin irritation. Patients also expressed their degree of on a VAS scale from 0 to 100.
Results
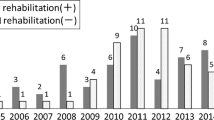
In the census phase the percentage of use of ASV (everyday, without problems) was equal to 17.27% (19/110 patients). The main causes of disuse concerned excessive fatigue and poor durability of the adhesives. The analysis of the results pre vs. post-training showed a statistically significant increase (p < 0.05) in all the investigated parameters. Patients reported a good level of treatment compliance (average frequency of performing exercises equal to 4.2 ± 2.5 days/week for 1.4 ± 1.01 h/day) and high degrees of satisfaction. After treatment, the percentage of use of AVS increased by 43% reaching a rate of 60% (66/110 patients).
Conclusion
A specific and targeted approach that simulate the phonatory and breathing difficulties of everyday life can increase the ASV usage rate.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ceachir O, Hainarosie R, Zainea V (2014) Total laryngectomy—past, present, future. Maedica (Bucur) 9(2):210–216
Longobardi Y, Parrilla C, Di Cintio G, De Corso E, Marenda ME, Mari G, Paludetti G, D’Alatri L, Passali GC (2020) Olfactory perception rehabilitation after total laryngectomy (OPRAT): proposal of a new protocol based on training of sensory perception skills. Eur Arch Otorhinolaryngol 277(7):2095–2105. https://doi.org/10.1007/s00405-020-05918-8
Debry C, Dupret-Bories A, Vrana NE, Hemar P, Lavalle P, Schultz P (2014) Laryngeal replacement with an artificial larynx after total laryngectomy: the possibility of restoring larynx functionality in the future. Head Neck 36(11):1669–1673. https://doi.org/10.1002/hed.23621
Boscolo-Rizzo P et al (2008) Long-term quality of life after total laryngectomy and postoperative radiotherapy versus concurrent chemoradiotherapy for laryngeal preservation. Laryngoscope 118:300–306
Longobardi Y, Savoia V, Bussu F, Morra L, Mari G, Nesci DA, Parrilla C, D’Alatri L (2019) Integrated rehabilitation after total laryngectomy: a pilot trial study. Support Care Cancer 27(9):3537–3544. https://doi.org/10.1007/s00520-019-4647-1
Ackerstaff AH, Fuller D, Irvin M, Maccracken E, Gaziano J, Stachowiak L (2003) Multicenter study assessing effects of heat and moisture exchanger use on respiratory symptoms and voice quality in laryngectomized individuals. Otolaryngol Head Neck Surg 129(6):705–712. https://doi.org/10.1016/S0194-59980301595-X
Mérol JC, Charpiot A, Langagne T, Hémar P, Ackerstaff AH, Hilgers FJ (2012) Randomized controlled trial on postoperative pulmonary humidification after total laryngectomy: external humidifier versus heat and moisture exchanger. Laryngoscope 122(2):275–281. https://doi.org/10.1002/lary.21841
Zuur JK, Muller SH, de Jongh FH, van Zandwijk N, Hilgers FJ (2006) The physiological rationale of heat and moisture exchangers in post-laryngectomy pulmonary rehabilitation: a review. Eur Arch Otorhinolaryngol 263(1):1–8. https://doi.org/10.1007/s00405-005-0969-3
Longobardi Y, Galli J, Di Cesare T, D’Alatri L, Settimi S, Mele D, Bussu F, Parrilla C. (2022) Optimizing pulmonary outcomes after total laryngectomy: crossover study on new heat and moisture exchangers. Otolaryngol Head Neck Surg (6):929–940. doi: https://doi.org/10.1177/01945998221086200. Epub 2022 Mar 22. Erratum in: Otolaryngol Head Neck Surg. 2022 Apr 18;:1945998221097077
Bień S, Okła S, van As-Brooks CJ, Ackerstaff AH (2010) The effect of a Heat and Moisture Exchanger (Provox HME) on pulmonary protection after total laryngectomy: a randomized controlled study. Eur Arch Otorhinolaryngol 267(3):429–435. https://doi.org/10.1007/s00405-009-1018-4
Hilgers FJ, Ackerstaff AH, Van As CJ, Balm AJ, Van den Brekel MW, Tan IB (2003) Development and clinical assessment of a heat and moisture exchanger with a multi-magnet automatic tracheostoma valve (Provox FreeHands HME) for vocal and pulmonary rehabilitation after total laryngectomy. Acta Otolaryngol 123(1):91–99. https://doi.org/10.1080/0036554021000028083
Van der Houwen EB VGJ, van der Laan BFAM. (2012) Development of a handsfree speech valve for laryngectomy patients chapter 1: p. 14-15.
Hilgers FJ, Ackerstaff AH (2006) Development and evaluation of a novel tracheostoma button and fixation system (Provox LaryButton and LaryClip adhesive) to facilitate hands-free tracheoesophageal speech. Acta Otolaryngol 126(11):1218–1224. https://doi.org/10.1080/00016480600702126
Dirven R, Hilgers FJ, Plooij JM et al (2008) 3D stereophotogrammetry for the assessment of tracheostoma anatomy. Acta Otolaryngol 128(11):1248–1254. https://doi.org/10.1080/00016480801901717
Ten Hallers EJ et al (2005) Difficulties in the fixation of prostheses for voice rehabilitation after laryngectomy. Acta Otolaryngol 125(8):804–813
Lorenz KJ, Groll K, Ackerstaff AH, Hilgers FJ, Maier H (2007) Hands-free speech after surgical voice rehabilitation with a Provox voice prosthesis: experience with the Provox FreeHands HME tracheostoma valve system. Eur Arch Otorhinolaryngol 264(2):151–157. https://doi.org/10.1007/s00405-006-0155-2
Op de Coul BM, Ackerstaff AH, van As-Brooks CJ et al (2005) Compliance, quality of life and quantitative voice quality aspects of hands-free speech. Acta Otolaryngol 125(6):629–637. https://doi.org/10.1080/00016480510031515
Leemans M, van Alphen MJA, Dirven R, Verkerke GJ, Hekman EEG, van den Brekel MWM (2021) Improving hands-free speech rehabilitation in patients with a laryngectomy: proof-of-concept of an intratracheal fixation device. Otolaryngol Head Neck Surg 165(2):317–320. https://doi.org/10.1177/0194599820982634
van der Houwen EB, van Kalkeren TA, Post WJ, Hilgers FJ, van der Laan BF, Verkerke GJ (2011) Does the patch fit the stoma? A study on peristoma geometry and patch use in laryngectomized patients. Clin Otolaryngol 36(3):235–241. https://doi.org/10.1111/j.1749-4486.2011.02307.x
Leemans M, Longobardi Y, Dirven R, Honings J, D’Alatri L, Galli J, van den Brekel M, Parrilla C, van Sluis KE (2023) Improving hands-free speech rehabilitation in laryngectomized patients with a moldable adhesive. Laryngoscope. https://doi.org/10.1002/lary.30636
Guilherme EM, Moreira RFC, de Oliveira A, Ferro AM, Di Lorenzo VAP, Gianlorenço ACL (2021) Respiratory disorders in Parkinson’s disease. J Parkinsons Dis 11(3):993–1010. https://doi.org/10.3233/JPD-212565
Hess MM, Schwenk RA, Frank W, Loddenkemper R (1999) Pulmonary function after total laryngectomy. Laryngoscope 109(6):988–994. https://doi.org/10.1097/00005537-199906000-00027
Laciuga H, Rosenbek JC, Davenport PW, Sapienza CM (2014) Functional outcomes associated with expiratory muscle strength training: narrative review. J Rehabil Res Dev 51(4):535–546. https://doi.org/10.1682/JRRD.2013.03.0076
Tillerson JL, Caudle WM, Reverón ME, Miller GW (2003) Exercise induces behavioral recovery and attenuates neurochemical deficits in rodent models of Parkinson’s disease. Neuroscience 119(3):899–911. https://doi.org/10.1016/s0306-4522(03)00096-4
Muhlack S, Welnic J, Woitalla D, Müller T (2007) Exercise improves efficacy of levodopa in patients with Parkinson’s disease. Mov Disord 22(3):427–430. https://doi.org/10.1002/mds.21346
Ramig L, Halpern A, Spielman J, Fox C, Freeman K (2018) Speech treatment in Parkinson’s disease: randomized controlled trial (RCT). Mov Disord 33(11):1777–1791. https://doi.org/10.1002/mds.27460
Tamplin J, Morris ME, Marigliani C, Baker FA, Noffs G, Vogel AP (2020) ParkinSong: outcomes of a 12-month controlled trial of therapeutic singing groups in Parkinson’s Disease. J Parkinsons Dis 10(3):1217–1230. https://doi.org/10.3233/JPD-191838
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Ylenia Longobardi and Claudio Parrilla designed the work. Ylenia Longobardi, Valentina Francesca Brandi, Giorgia Mari, Maria Raffaella Marchese and Maria Elisabetta Marenda acquired and analysed data. Ylenia Longobardi. Lucia D’Alatri and Claudio Parrilla drafted and all authors revised the manuscript. Jacopo Galli approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
All Authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The “Comitato Etico Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS—Università Cattolica del Sacro Cuore” approved this study (ID 4650).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Longobardi, Y., D’Alatri, L., Brandi, V.F. et al. Automatic speaking valve in tracheo-esophageal speech: treatment proposal for a widespread usage. Eur Arch Otorhinolaryngol 281, 3197–3205 (2024). https://doi.org/10.1007/s00405-024-08605-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-024-08605-0