Abstract
Purpose
This study aimed to analyze the clinical characteristics, pathogen distribution, drug sensitivity, and antibiotic treatment strategies of patients with neck abscesses with or without diabetes.
Methods
A retrospective analysis was conducted on 2194 patients who underwent neck abscess surgery at our hospital over the past 13 years. Patients were grouped as NAwithDM (neck abscess with diabetes mellitus) or NAwithoutDM (neck abscess without diabetes mellitus). Clinical features, pathogen distribution, and antibiotic sensitivity were compared between the groups. Venn diagrams were used to illustrate the antibiotics effective against all three predominant pathogens.
Results
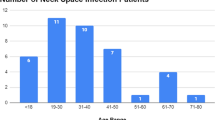
A total of 2194 patients with neck abscesses were included in this study, with 579 patients (26.43%) in the NAwithDM group and 1612 patients (73.51%) in the NAwithoutDM group. There were no significant differences in sex or age distribution between the two groups (all P > 0.05). However, there were significant differences in BMI, length of hospital stays, occurrence of laryngeal obstruction, hypertension, and hypoalbuminemia between the two groups (all P < 0.05). In the NAwithoutDM group, the top three pathogens were Streptococcus constellatus, Klebsiella pneumoniae, and Staphylococcus aureus. The antibiotics that were simultaneously effective against all three pathogens were ceftriaxone, moxifloxacin, and ampicillin/sulbactam. In the NAwithDM group, the top three pathogens were Streptococcus pyogenes, Streptococcus pneumoniae, and Streptococcus constellatus. The antibiotics that were simultaneously effective against all three pathogens were compound sulfamethoxazole, cefuroxime, levofloxacin, ciprofloxacin, vancomycin, and imipenem.
Conclusion
Neck abscess patients with diabetes have distinct clinical features. Therefore, it is crucial to pay attention to these clinical features and manage them accordingly during the treatment process. Empirical antibiotic treatment should be tailored to individual patient groups. Sulfamethoxazole-methoxazole is recommended for neck abscess patients with diabetes, while ceftriaxone or moxifloxacin is recommended for those without diabetes.



Similar content being viewed by others
Data availability
Relevant data can be obtained by contacting the first author.
References
Bal KK, Unal M, Delialioglu N, Oztornaci RO, Ismi O, Vayisoglu Y (2022) Diagnostic and therapeutic approaches in deep neck infections: an analysis of 74 consecutive patients. Braz J Otorhinolaryngol 88:511–522. https://doi.org/10.1016/j.bjorl.2020.07.002
Bigus S, Russmüller G, Starzengruber P, Reitter H, Sacher CL (2023) Antibiotic resistance of the bacterial spectrum of deep space head and neck infections in oral and maxillofacial surgery—a retrospective study. Clin Oral Investig. https://doi.org/10.1007/s00784-023-05095-y
Chung HF, Al Mamun A, Huang MC, Long KZ, Huang YF, Shin SJ, Hwang SJ, Hsu CC (2017) Obesity, weight change, and chronic kidney disease in patients with type 2 diabetes mellitus: a longitudinal study in Taiwan. J Diabetes 9:983–993. https://doi.org/10.1111/1753-0407.12514
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A (2015) Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA 313:603–615. https://doi.org/10.1001/jama.2014.18574
Gao W, Lin Y, Yue H, Chen W, Liu T, Ye J, Cai Q, Ye F, He L, Xie X (2022) Bacteriological analysis based on disease severity and clinical characteristics in patients with deep neck space abscess. BMC Infect Dis 22:280. https://doi.org/10.1186/s12879-022-07259-9
Hidaka H, Yamaguchi T, Hasegawa J, Yano H, Kakuta R, Ozawa D, Nomura K, Katori Y (2015) Clinical and bacteriological influence of diabetes mellitus on deep neck infection: systematic review and meta-analysis. Head Neck 37:1536–1546. https://doi.org/10.1002/hed.23776
Hirano T (2014) Abnormal lipoprotein metabolism in diabetic nephropathy. Clin Exp Nephrol 18:206–209. https://doi.org/10.1007/s10157-013-0880-y
Ho C-Y, Chan K-C, Wang Y-C, Chin S-C, Chen S-L (2023) Assessment of factors associated with long-term hospitalization in patients with a deep neck infection. Ear Nose Throat J. https://doi.org/10.1177/01455613231168478
Hodgson K, Morris J, Bridson T, Govan B, Rush C, Ketheesan N (2015) Immunological mechanisms contributing to the double burden of diabetes and intracellular bacterial infections. Immunology 144:171–185. https://doi.org/10.1111/imm.12394
Jicman D, Sârbu N, Rebegea L-F, Crăescu M, Niculeț E, Țuța M-D, Nechita A, Nicolescu AC, Tatu AL (2023) Principles of treatment and clinical-evolutionary peculiarities of deep cervical spaces suppurations—clinical study. Life 13:535. https://doi.org/10.3390/life13020535
Kauffmann P, Cordesmeyer R, Tröltzsch M, Sömmer C, Laskawi R (2017) Deep neck infections: a single-center analysis of 63 cases. Medicina oral, patologia oral y cirugia bucal 22:e536. https://doi.org/10.4317/medoral.21799
Lim H-K, Wang J-M, Hung S-T, Ku H-C (2021) A dangerous cause of airway obstruction: deep neck infection. Signa Vitae 17:4–9. https://doi.org/10.22514/sv.2020.16.0101
Luan C-W, Liu C-Y, Yang Y-H, Tsai M-S, Tsai Y-T, Hsu C-M, Wu C-Y, Chang P-J, Chang G-H (2021) The pathogenic bacteria of deep neck infection in patients with type 1 diabetes, type 2 diabetes, and without diabetes from Chang Gung Research Database. Microorganisms 9:2059. https://doi.org/10.3390/microorganisms9102059
Maurer FP, Christner M, Hentschke M, Rohde H (2017) Advances in rapid identification and susceptibility testing of bacteria in the clinical microbiology laboratory: implications for patient care and antimicrobial stewardship programs. Infect Dis Rep 9:6839. https://doi.org/10.3390/microorganisms9102059
McDowell RH, Hyser MJ (2017) Neck abscess. StatPearls. StatPearls Publishing, Treasure Island
Mettler J, Simcock M, Sendi P, Widmer AF, Bingisser R, Battegay M, Fluckiger U, Bassetti S (2007) Empirical use of antibiotics and adjustment of empirical antibiotic therapies in a university hospital: a prospective observational study. BMC Infect Dis 7:1–10. https://doi.org/10.1186/1471-2334-7-21
Rijal S, Romdhoni AC (2018) Bacteria pattern, results of antibiotic sensitivity test, and complications of deep neck abscess patients in Dr. Soetomo General Hospital. Biomol Health Sci J 1:124. https://doi.org/10.20473/bhsj.v1i2.9832
Schutta MH (2007) Diabetes and hypertension: epidemiology of the relationship and pathophysiology of factors associated with these comorbid conditions. J Cardiometab Syndr 2:124–130. https://doi.org/10.1111/j.1559-4564.2007.06368.x
Velhonoja J, Lääveri M, Soukka T, Irjala H, Kinnunen I (2020) Deep neck space infections: an upward trend and changing characteristics. Eur Arch Otorhinolaryngol 277:863–872. https://doi.org/10.1007/s00405-019-05742-9
Wu C-L, Tsai M-S, Lee T-J, Wang Y-T, Liu C-Y, Yang Y-H, Tsai Y-T, Hsu C-M, Wu C-Y, Chang P-J (2021) Type 2 diabetes mellitus increases peritonsillar abscess susceptibility: real-world evidence. Clin Exp Otorhinolaryngol 14:347–354. https://doi.org/10.21053/ceo.2020.02257
Huttner B et al (2010) Characteristics and outcomes of public campaigns aimed at improving the use of antibiotics in outpatient settings in high-income countries. Lancet Infect Dis 10(1):17–31. https://doi.org/10.1016/S1473-3099(09)70305-6
Acknowledgements
Hai Li and Hailing Gu for their critical advises on the publication.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kong, W., Zhang, X., Li, M. et al. Microbiological analysis and antibiotic selection strategy in neck abscesses among patients with diabetes mellitus. Eur Arch Otorhinolaryngol 281, 1515–1523 (2024). https://doi.org/10.1007/s00405-023-08396-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08396-w