Abstract
Introduction
The universal newborn hearing screening (UNHS) allows for early detection of hearing impairment (HI). The goal of this current study was to evaluate the impact of cultural background involving consanguineous marriage on newborn HI diagnosed using UNHS, and compliance with hearing rehabilitation.
Materials and methods
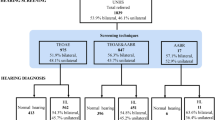
This is a retrospective cohort study that included all children born at a single tertiary medical center between 2011 and 2017 who did not pass the UNHS (oto-acoustic emission and auditory brainstem response), and were diagnosed with HI. The study group included children from consanguineous marriage cultural background which were compared to a control group—all other children. Data were retrieved from the computerized medical charts and included epidemiological, audiological, and pregnancy/delivery-related data, and known risk factors for congenital HI.
Results
A total of 238 (196 study and 42 control) neonates were diagnosed with HI. Family history of HI was significantly more prevalent in the study group in mild–severe and profound HI subgroups (p = 0.03 and 0.01, respectively). Study group demonstrated lower rates of cochlear implantation (CI) compliance (p = 0.079), performed at a significantly older age (23 months (IQR 17–36.5) vs. 16 (IQR 12–26) months, p = 0.021). When recommended, bilateral CI compliance was significantly lower in the study group (94.1 vs.48.9%, p < 0.001).
Conclusion
UNHS allows for early HI detection among minority populations at higher risk for CI, yet compliance rates remain lower compared with control. Familiarity of families with the importance of early detection and HI risk may result in higher compliance rates for cochlear implantation. Health providers should aim to improve education and communication with this unique group of patients and consider health promotion programs.
Similar content being viewed by others
Availability of data and materials
If needed, all data are available.
References
Israeli Ministry of Health. Guidelines for newborn screening for identification of congenital hearing loss (2009) [Hebrew]. http://www.health.gov.il/hozer/mr33_2009.pdf. Accessed 27 Dec 2016
Data and Statistics About Hearing Loss in Children | CDC [Internet]. [cited 2020 Feb 25]. Available from: https://www.cdc.gov/ncbddd/hearingloss/data.html
Joint Committee on Infant Hearing (2019). Year 2019 position statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J Early Hearing Detection and Intervention Programs 4:1–44. 120: 898–921.
Neonatal Hearing Screening Working Group (2013) National framework for neonatal hearing screening. Department of Health, Canberra
Matulat P, Parfitt R (2018) The newborn hearing screening programme in Germany. Int J Neonat Screen 4:29
Berrettini S, Ghirri P, Lazzerini F, Lenzi G, Forli F (2016) New Zealand Government. Universal Newborn Hearing national policy and quality standards. Ministry of Health, Wellington
Pimperton H, Blythe H, Kreppner J et al (2016) The impact of universal newborn hearing screening on long-term literacy outcomes: a prospective cohort study. Arch Dis Child 101:9–15
World Health Organization. Newborn and infant hearing screening: current issues and guiding principles [Internet]. Geneva: World Health Organization, 2009. Available at: http://www.who.int/blindness/publications/Newborn_and_Infant_Hearing_Screening_Report.pdf. (Accessed 2 Sep 2020).
Busa J, Harrison J, Chappell J, Yoshinaga-Itano C, Grimes A, Brookhouser PE et al (2007) Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 120(4):898–921
Warner-Czyz AD, Roland JT Jr, Thomas D, Uhler K, Zombek L (2022) American Cochlear Implant Alliance Task Force Guidelines for Determining Cochlear Implant Candidacy in Children. Ear Hear 43(2):268–282. https://doi.org/10.1097/AUD.0000000000001087
Armstrong M, Maresh A, Buxton C, Craun P, Wowroski L, Reilly B, Preciado D (2013) Barriers to early pediatric cochlear implantation. Int J Pediatr Otorhinolaryngol 77(11):1869–1872. https://doi.org/10.1016/j.ijporl.2013.08.031. (Epub 2013 Sep 5 PMID: 24035734)
Panda S, Sikka K, Singh V, Agarwal S, Kumar R, Thakar A, Sharma SC (2019) Comprehensive Analysis of Factors Leading to Poor Performance in Prelingual Cochlear Implant Recipients. Otol Neurotol 40(6):754–760. https://doi.org/10.1097/MAO.0000000000002237. (PMID: 31135664)
Dham R, Dharmarajan S, Kurkure R, Sampath Kumar RN, Kameswaran M (2021) Socio-demographic profile and its influences on rehabilitation in children undergoing revision cochlear implantation—MERF experience. Int J Pediatr Otorhinolaryngol 151:110919. https://doi.org/10.1016/j.ijporl.2021.110919. (Epub 2021 Sep 10 PMID: 34560572)
Goldblat E, Rivkin D, Konstantinov V (2020) Associations between ethnicity, place of residence, hearing status of family and habilitation of children with hearing impairment. Isr J Health Policy Res 9:36. https://doi.org/10.1186/s13584-020-00394-1
Na’amnih W, Romano-Zelekha O, Kabaha A, Rubin LP, Bilenko N, Jaber L et al (2014) Prevalence of consanguineous marriages and associated factors among Israeli Bedouins. J Commun Genet 5(4):395
Oren Tirosh, Dr. Yonatan Eyal (2018) Socio-Economic Measures for the Bedouin Population in the Negev [Internet]. [cited 2020 Nov 17]. Available from: https://brookdale.jdc.org.il/wp-content/uploads/2018/10/Heb_Report_774_18_update.pdf
Rudnitzky A, Ras TA (2012) The Bedouin Population in the Negev. Abraham Fund Inititatives. https://books.google.co.il/books?id=X480lwEACAAJ
Melamed Y, Bashiri A, Shoham-Vardi I, Furman B, Hackmon-Ram R, Mazor M (2000) Differences in preterm delivery rates and outcomes in Jews and Bedouins in southern Israel. Eur J Obstet Gynecol Reprod Biol 93(1):41–46
Greiner RC, Rubinstein JT, Kohlberg GD (2023) Investigating Socioeconomic Barriers to Cochlear Implantation. Otol Neurotol 44(9):e660–e666. https://doi.org/10.1097/MAO.0000000000003985. (Epub 2023 Aug 19 PMID: 37604510)
Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL (1998) Language of early- and later-identified children with hearing loss. Pediatrics 102(5):1161–1171
Yoshinaga-Itano C (2003) Early Intervention after Universal Neonatal Hearing Screening: Impact on Outcomes. Ment Retard Dev Disabil Res Rev 9(4):252–266
Kothari S, Keshree NK, Bhatnagar S (2015) Pediatric cochlear implantation—why the delay. Indian J Otolaryngol Head Neck Surg 67(2):165
Arumugam SV, Paramasivan VK, Murali S, Natarajan K, Sudhamaheswari, Kameswaran M (2015) Syndromic deafness-prevalence, distribution and hearing management protocol in Indian scenario. Ann Med Surg 4(2):143–150
Kumar RN, Kameswaran M (2017) Cochlear implantation in the developing world: perspectives from the Indian subcontinent. ENT Audiol News 26(4):1–2
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript. MD + OZ + DK + OC—wrote the paper, designed the study, wrote the Helsinki proposal. LK + RG—analyzed the audiologic data. EL + SK + YS + SES—data collection and discussion. MAT—statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interests.
Ethics approval and consent to participate
The study was approved by the institutional Helsinki approval-SOR 17-0362. The need for consent to participate was waived by the Helsinki committee.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ziv, O., Danovitch, M., Kaplan, D.M. et al. Cochlear implantation compliance among minorities at high risk for hearing impairment following universal newborn hearing screening. Eur Arch Otorhinolaryngol 281, 2877–2882 (2024). https://doi.org/10.1007/s00405-023-08371-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08371-5