Abstract
Purpose
Chronic rhinosinusitis (CRS) is a chronic disease with a high recurrence rate, and the aim of treating CRS is to maintain disease control. Recently, a series of CRS control instruments have been developed to assess the control levels. We pooled existing studies to evaluate the percentage of controlled CRS after treatment in patients with CRS.
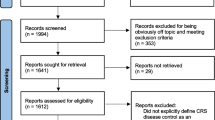
Methods
A systematic literature review and meta-analysis using PubMed, Google Scholar, Scopus, and Cochrane databases was conducted to identify studies assessing CRS control. Both comprehensive assessments and self-report of CRS control were included.
Results
9 studies with 1931 patients after treatment and 295 patients before treatment were included. CRS control assessments of the 2012 European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS 2012), EPOS 2020, and Sinus Control Test (SCT) were comprehensive assessments utilized in the clinic practice. The self-report assessment included patient-reported global level of CRS control. These existing disease control instruments categorized patients into three (uncontrolled, partly controlled, and controlled) or five (not at all, a little, somewhat, very, and completely) control categories. Only 8% (95% CI 0.05–0.11) of patients with CRS stayed well controlled before treatment assessed by comprehensive assessments. About 35% (95% CI 0.22–0.49) of patients achieved well controlled after treatment when assessed by the comprehensive measures. Meanwhile, 40% (95% CI 0.28–0.52) of patients reported well controlled after treatment when using self-report.
Conclusion
About 35–40% of patients with CRS showed well controlled after treatment, which stressed the importance of identifying these undertreated patients with CRS.




Similar content being viewed by others
Data availability
Not applicable.
References
Hastan D, Fokkens WJ, Bachert C et al (2011) Chronic rhinosinusitis in Europe: an underestimated disease. A GA (2) LEN study. Allergy 66(9):1216–1223
Palmer JN, Messina JC, Biletch R, Grosel K, Mahmoud RA (2019) A cross-sectional, population- based survey of US adults with symptoms of chronic rhinosinusitis. Allergy Asthma Proc 40:4182
Hirsch AG, Stewart WF, Sundaresan AS et al (2017) Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy 72(2):274–281
DeConde AS, Soler ZM (2016) Chronic rhinosinusitis: epidemiology and burden of disease. Am J Rhinol Allergy 30(2):134–139
Baguley C, Brownlow A, Yeung K, Pratt E, Sacks R, Harvey R (2014) The fate of chronic rhinosinusitis sufferers after maximal medical therapy: the fate of CRS sufferers after MMT. Int Forum Allergy Rhinol 4(7):525–532
Alanin MC, Hopkins C (2020) Effect of functional endoscopic sinus surgery on outcomes in chronic rhinosinusitis. Curr Allergy Asthma Rep 20(7):27
Stevens WW, Schleimer RP, Kern RC (2016) Chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol Pract 4(4):565–572
DeConde AS, Mace JC, Levy JM, Rudmik L, Alt JA, Smith TL (2017) Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis: polyp recurrence after ESS. Laryngoscope 127(3):550–555
Wu D, Bleier BS, Wei Y (2019) Current understanding of the acute exacerbation of chronic rhinosinusitis. Front Cell Infect Microbiol 9:415
Wu D, Bleier B, Wei Y (2020) Definition and characteristics of acute exacerbation in adult patients with chronic rhinosinusitis: a systematic review. J Otolaryngol Head Neck Surg 49(1):62
Banglawala SM, Schlosser RJ, Morella K et al (2016) Qualitative development of the sinus control test: a survey evaluating sinus symptom control. Int Forum Allergy Rhinol 6(5):491–499
Little RE, Schlosser RJ, Smith TL et al (2021) Disease control after surgery for chronic rhinosinusitis: prospective, multi-institutional validation of the Sinus Control Test. Int Forum Allergy Rhinol 11(2):106–114
Lourijsen ES, Reitsma S, Vleming M et al (2022) Endoscopic sinus surgery with medical therapy versus medical therapy for chronic rhinosinusitis with nasal polyps: a multicentre, randomised, controlled trial. Lancet Respir Med 10(4):337–346
van der Veen J, Seys SF, Timmermans M, Levie P et al (2017) Real-life study showing uncontrolled rhinosinusitis after sinus surgery in a tertiary referral centre. Allergy 72(2):282–290
Wang KH, Deng J, Yang M et al (2021) Concordant systemic and local eosinophilia relates to poorer disease control in patients with nasal polyps. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 56(10):1042–1050
Kohli P, Soler ZM, Storck KA, Shahangian A, Banglawala SM, Schlosser RJ (2017) Responsiveness and reliability of the Sinus Control Test in chronic rhinosinusitis. Rhinology 55(1):39–44
Tao X, Chen F, Sun Y et al (2018) Prediction models for postoperative uncontrolled chronic rhinosinusitis in daily practice. Laryngoscope 128(12):2673–2680
Campbell AP, Hoehle LP, Phillips KM, Caradonna DS, Gray ST, Sedaghat AR (2018) Symptom control in chronic rhinosinusitis is an independent predictor of productivity loss. Eur Ann Otorhinolaryngol Head Neck Dis 135(4):237–241
McCann AC, Trope M, Walker VL et al (2021) Olfactory dysfunction is not a determinant of patient-reported chronic rhinosinusitis disease control. Laryngoscope 131(7):E2116–E2120
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Rostom A, Dubé C, Cranney A et al (2004) Celiac disease. Agency for Healthcare, Rockville (Evidence Reports/Technology Assessments, No. 104.) Appendix D. Quality Assessment Forms)
Hu J, Dong Y, Chen X et al (2015) Prevalence of suicide attempts among Chinese adolescents: a meta-analysis of cross-sectional studies. Compr Psychiatry 61:78–89
Higgins JP, Altman DG, Gøtzsche PC et al (2011) Cochrane bias methods group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:5928
Fokkens WJ, Lund VJ, Mullol J (2012) EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50(1):1–12
Sedaghat AR, Phillips KM (2023) Defining ‘control’ of chronic rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg 31(1):17–23
Fokkens WJ, Lund VJ, Hopkins C (2020) European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58:1–464
Phillips KM, Singerman KW, Sedaghat AR (2022) Individual symptom visual analogue scale severity scores for determining EPOS guideline-based chronic rhinosinusitis disease control. Rhinology 60–3:229–235
Snidvongs K, Heller GZ, Sacks R, Harvey RJ (2014) Validity of European position paper on rhinosinusitis disease control assessment and modifications in chronic rhinosinusitis. Otolaryngol Neck Surg 150(3):479–486
Sedaghat AR, Hoehle LP, Gray ST (2018) Chronic rhinosinusitis control from the patient and physician perspectives: Understanding CRS disease control. Laryngoscope Investig Otolaryngol 3(6):419–433
Gray ST, Phillips KM, Hoehle LP, Caradonna DS, Sedaghat AR (2017) The 22-item Sino-Nasal Outcome Test accurately reflects patient-reported control of chronic rhinosinusitis symptomatology: SNOT-22 and CRS symptom control. Int Forum Allergy Rhinol 7(10):945–951
Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, Toppila-Salmi S, Bernal-Sprekelsen M, Mullol J (2020) Executive summary of EPOS 2020 including integrated care pathways. Rhinology 58(2):82–111
Guo CL, Liao B, Liu JX, Pan L, Liu Z (2021) Predicting difficult-to-treat chronic rhinosinusitis by noninvasive biological markers. Rhinology 59(1):81–90
Sedaghat AR, Singerman KW, Phillips KM (2022) Discordance of chronic rhinosinusitis disease control between EPOS guidelines and patient perspectives identifies utility of patient-rated control assessment. Rhinology 60(6):444–452
Funding
Natural Science Foundation of China (82000954), Beijing Science and Technology Nova Program (Z201100006820086), Beijing Hospitals Authority Youth Program (QML20190617), and Beijing Hospitals Authority Clinical Medicine Development of Special Funding (XMLX202136).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception, analysis, and interpretation of data in this article, approved the submitted version, and agreed to be personally accountable for our contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which we are not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest/competing interests.
Research involving human participants and/or animals
This is a meta-analysis.
Informed consent
Not available.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, T., Zhou, J., Yuan, F. et al. The percentage of controlled chronic rhinosinusitis after treatment: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 281, 2183–2194 (2024). https://doi.org/10.1007/s00405-023-08363-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08363-5