Abstract
Purpose
Compared with other types of thyroid carcinoma, patients with medullary thyroid carcinoma (MTC) are more likely to develop cervical lymph node metastasis. This study was conducted to clarify the risk factors for cervical lymph node metastasis (central lymph node metastasis or lateral cervical lymph node metastasis) in MTC by meta-analysis, and to provide evidence-based basis for the treatment and prognosis of MTC.
Methods
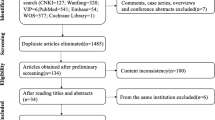
The literatures related to cervical lymph node metastasis in medullary thyroid carcinoma were searched in PubMed, Embase, Web of Science, Cochrane, CNKI and Wanfang databases, and statistical analysis was performed using Revman 5.3 and Stata 14.0 software.
Results
A total of 28 papers were included in this paper, and meta-analysis showed that the occurrence of central lymph node metastasis (CLNM) in MTC patients was significantly associated with tumor size (OR = 3.07, 95%CI: 2.04–4.63, P < 0.00001), multifocality (OR = 0.29, 95%CI: 0.19–0.44, P < 0.00001), bilaterality (OR = 3.75, 95% CI: 1.95–7.14, P < 0.0001), capsular invasion (OR = 9.88, 95% CI: 5.93–16.45, P < 0.00001) and extrathyroidal extension (OR = 5.48, 95% CI: 2.61–11.51, P < 0.00001). While the occurrence of lateral cervical lymph node metastasis (LLNM) in MTC patients was strongly correlated with gender (OR = 2.97, 95%CI: 2.46–3.58, P < 0.00001), tumor size (OR = 3.88, 95%CI: 1.90–7.92, P = 0.0002 < 0.05), multifocality (OR = 0.43, 95%CI: 0.35–0.51, P < 0.00001), bilaterality (OR = 2.93, 95% CI: 1.72–4.98, P < 0.0001), capsular invasion (OR = 8.44, 95% CI: 6.11–11.64, P < 0.00001), extrathyroidal extension (OR = 7.04, 95% CI: 5.54–8.94, P < 0.00001), margin of the tumor (OR = 4.47, 95% CI: 2.37–8.44, P < 0.00001), shape of the tumor (OR = 6.81, 95% CI: 3.64–12.73, P < 0.00001), preoperative calcitonin level (SMD = 1.39, 95% CI: 0.98–1.80, P < 0.00001), preoperative carcinoembryonic antigen level (SMD = 0.97, 95% CI: 0.74–1.20, P < 0.00001) and CLNM (OR = 19.70, 95% CI: 14.16–27.43, P < 0.00001).
Conclusion
Tumor size, multifocality, bilaterality, capsular invasion and extrathyroidal extension are the main risk factors for developing CLNM in MTC patients; And risk factors for developing LLNM in MTC patients include: gender, tumor size, multifocality, bilaterality, capsular invasion, extrathyroidal extension, margin of the tumor, shape of the tumor, preoperative calcitonin level, preoperative carcinoembryonic antigen level and central lymph node metastasis. These risk factors can guide the individualized treatment plan and improve the prognosis of MTC patients.






Similar content being viewed by others
Data availability
All the data generated in the present study are included within the meta-analysis.
References
Wells SA Jr, Asa SL, Dralle H et al (2015) Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25:567–610
Larouche V, Akirov A, Thomas CM, Krzyzanowska MK, Ezzat S (2019) A primer on the genetics of medullary thyroid cancer. Curr Oncol 26:389–394
Randle RW, Balentine CJ, Leverson GE et al (2017) Trends in the presentation, treatment, and survival of patients with medullary thyroid cancer over the past 30 years. Surgery 161:137–146
Machens A, Lorenz K, Dralle H (2020) Prediction of biochemical cure in patients with medullary thyroid cancer. Br J Surg 107:695–704
Abraham DT, Low TH, Messina M et al (2011) Medullary thyroid carcinoma: long-term outcomes of surgical treatment. Ann Surg Oncol 18:219–225
Ganeshan D, Paulson E, Duran C et al (2013) Current update on medullary thyroid carcinoma. AJR Am J Roentgenol 201:W867–W876
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27:1785–1805
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Yan DG, Zhang B, Li ZJ, et al. Cervical lymph node metastasis in medullary thyroid carcinoma. Chinese Journal of otolaryngology Head and Neck Surgery. 2015:290–294.
Fan W, Xiao C, Wu F (2018) Analysis of risk factors for cervical lymph node metastases in patients with sporadic medullary thyroid carcinoma. J Int Med Res 46:1982–1989
Lu QC. Clinical characteristics of medullary thyroid carcinoma and related factors of lymph node metastasis. Zhengzhou University, 2019.
Meng QY. Analysis of risk factors for cervical lymph node metastasis in medullary thyroid carcinoma. Jilin University, 2020.
Zhang L. The research of related factors of cervical lymph node metastasis on medullary thyroid carcinoma. Tianjin Medical University, 2020.
Ding JW, Zheng WH, Zhao JZ, et al. Clinical value of preoperative serum calcitonin to evaluate the lymph node metastasis in different regions of medullary thyroid carcinoma. Chinese Department of Otolaryngology Head and Neck Surgery. 2021;28:1–4.
Zhu QD. Correlation between Ultrasonic Features of Thyroid Carcinoma and Cervical Lymph Node Metastasis. Zhejiang Chinese Medicine University, 2021.
Zhang LY. Analysis of risk factors for cervical lymph node metastasis and postoperative recurrence of medullary thyroid carcinoma. Zhengzhou University. 2022.
Wang JY, Zhang B, Yan DG et al (2012) Type of Surgery for Untreated Medullary Thyroid Carcinoma: A Report of 73 Cases. Chinese oncology clinic 39:410–413
Chandeze MM, Noullet S, Faron M et al (2016) Can We Predict the Lateral Compartment Lymph Node Involvement in RET-Negative Patients with Medullary Thyroid Carcinoma? Ann Surg Oncol 23:3653–3659
Oh HS, Kwon H, Song E et al (2018) Preoperative Clinical and Sonographic Predictors for Lateral Cervical Lymph Node Metastases in Sporadic Medullary Thyroid Carcinoma. Thyroid 28:362–368
Pena I, Clayman GL, Grubbs EG et al (2018) Management of the lateral neck compartment in patients with sporadic medullary thyroid cancer. Head Neck 40:79–85
Ito Y, Miyauchi A, Kihara M et al (2018) Static Prognostic Factors and Appropriate Surgical Designs for Patients with Medullary Thyroid Carcinoma: The Second Report from a Single-Institution Study in Japan. World J Surg 42:3954–3966
Li SL, Hou XK, Dong JL et al (2019) Prediction of lateral cervical lymph node metastasis in patients with sporadic medullary thyroid carcinoma using preoperative clinical and ultrasonographic features. Chinese oncology clinic 46:1032–1035
Ding HR. Clinical and pathologic predictors of lateral cervical lymph nodemetastasis in medullary thyroid carcinoma. Dalian Medical University, 2019.
Yu SF. Analysis of predictor factors for lateral neck metastasis in medullary thyroid carcinoma. Zhejiang University, 2019.
Opsahl EM, Akslen LA, Schlichting E et al (2019) The Role of Calcitonin in Predicting the Extent of Surgery in Medullary Thyroid Carcinoma: A Nationwide Population-Based Study in Norway. Eur Thyroid J 8:159–166
Wu X, Li B, Zheng C et al (2020) Risk Factors for Lateral Lymph Node Metastases in Patients With Sporadic Medullary Thyroid Carcinoma. Technol Cancer Res Treat 19:1533033820962089
Ye L, Zhou X, Lu J et al (2020) Combining serum calcitonin, carcinoembryonic antigen, and neuron-specific enolase to predict lateral lymph node metastasis in medullary thyroid carcinoma. J Clin Lab Anal 34:e23278
Park H, Park J, Choi MS, et al. Preoperative Serum Calcitonin and Its Correlation with Extent of Lymph Node Metastasis in Medullary Thyroid Carcinoma. Cancers (Basel). 2020;12.
Liu X, Zhu QD, Shao ZY et al (2020) Analysis of correlation factors between lateral cervical lymph node metastasis and ultrasonic features of medullary thyroid carcinoma. Imaging research and medical applications 4:64–66
Ye LQ, Mao XC, Ding JW, Zheng WH, Zhou GM. Risk model of lateral lymph node metastasis in 145 cases of operable medullary thyroidcarcinoma. Chinese Department of Otolaryngology Head and Neck Surgery. 2021;28:669–673.
Zhou TH, Zhao LQ, Zhang Y et al (2021) The Prediction of Metastases of Lateral Cervical Lymph Node in Medullary Thyroid Carcinoma. Front Endocrinol (Lausanne) 12:741289
Zhao J, Hao WJ, Mao YR et al (2021) Early diagnosis and prediction for lateral cervical lymph node metastases of medullarythvroid microcarcinoma. Chinese Journal of General Surgery 36:416–420
Zhang CS, Reng M, Meng DL, Wang P, Wang Y (2022) Risk factors analysis of lateral cervical lymph node metastasis in medullary thyroid carcinoma. Journal of Clinical Surgery 30:230–233
Huang SJ, Zhong JN, Chen H (2022) Nomograms for prediction of cervical lymph node metastasis in medullary thyroid carcinoma. Modern oncology 30:416–421
Li C, Zhang H, Li S et al (2022) Prognostic Impact of Inflammatory Markers PLR, LMR, PDW, MPV in Medullary Thyroid Carcinoma. Front Endocrinol (Lausanne) 13:861869
Wu X, Li B, Zheng C (2022) Clinical Characteristics, Surgical Management, and Prognostic Factors of Medullary Thyroid Carcinoma: A Retrospective. Single-Center Study Technol Cancer Res Treat 21:15330338221078436
Meng K, Luo H, Chen H, Guo H, Xia W (2019) Prognostic value of numbers of metastatic lymph node in medullary thyroid carcinoma: A population-based study using the SEER 18 database. Medicine (Baltimore) 98:e13884
Mathiesen JS, Kroustrup JP, Vestergaard P et al (2019) Survival and Long-Term Biochemical Cure in Medullary Thyroid Carcinoma in Denmark 1997–2014: A Nationwide Study. Thyroid 29:368–377
Contarino A, Dolci A, Maggioni M et al (2022) Is Encapsulated Medullary Thyroid Carcinoma Associated With a Better Prognosis? A Case Series and a Review of the Literature. Front Endocrinol (Lausanne) 13:866572
Ye LQ, Xu XJ, Ding JW et al (2017) Significance of serum calcitonin and carcinoembryonic antigen in clinical evaluation of medullary thyroid carcinoma. Chinese Journal of Health Inspection 27:201–204
Mitchell AL, Gandhi A, Scott-Coombes D, Perros P (2016) Management of thyroid cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 130:S150–S160
Xu N, Jian Y, Wang Y, Tian W (2018) Evaluation of neutrophil-to-lymphocyte ratio and calcitonin concentration for predicting lymph node metastasis and distant metastasis in patients with medullary thyroid cancer. Mol Clin Oncol 9:629–634
Guo YP, Huang CW, Zhou RL, Wang ML, Liu YY (2022) Correlation Between Ultrasonographic Features and Tumor Size of Medullary ThyroidCarcinoma and Analysis of Causes of Misdiagnosis. Evid Based Med 22:286–290
Haddad RI, Nasr C, Bischoff L, et al. NCCN Guidelines Insights: Thyroid Carcinoma, Version 2.2018. J Natl Compr Canc Netw. 2018;16:1429–1440.
Kaliszewski K, Zubkiewicz-Kucharska A, Wojtczak B, Strutynska-Karpinska M (2016) Multi- and Unifocal Thyroid Microcarcinoma: Are There Any Differences? Adv Clin Exp Med 25:485–492
Feng JW, Wu WX, Hu J et al (2020) Influence of Tumor Number on Clinicopathologic Features and Outcomes of Patients With Papillary Thyroid Carcinoma. Am J Clin Pathol 154:848–858
Tran B, Roshan D, Abraham E, et al. An Analysis of The American Joint Committee on Cancer 8th Edition T Staging System for Papillary Thyroid Carcinoma. J Clin Endocrinol Metab. 2018;103:2199–2206.
Shaha AR (2018) Clinical significance of extrathyroidal extension according to size of papillary thyroid carcinoma. Eur J Surg Oncol 44:1669–1670
Zhou J, Ma WT (2019) The value of ultrasound in the diagnosis of medullary thyroid carcinoma. Imaging research and medical applications 3:19–21
Maia AL, Wajner SM, Vargas CV (2017) Advances and controversies in the management of medullary thyroid carcinoma. Curr Opin Oncol 29:25–32
Acknowledgements
We would like to thank all the reviewers who participated in the review.
Funding
This work was supported by the Natural Science Foundation of Hebei Province (H2020307028).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical statement
N.A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, X., Huo, J., Su, H. et al. Risk factors for cervical lymph node metastasis in the central or lateral cervical region in medullary thyroid carcinoma: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 281, 547–561 (2024). https://doi.org/10.1007/s00405-023-08249-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08249-6