Abstract
Background
Lymphatic metastatic size was proved to predict prognosis in different types of carcinomas, except in head and neck squamous cell carcinoma (HNSCC) located in hypopharynx, oropharynx and supraglottic region et al. The aim of this study is to evaluate the prognostic value of lymphatic metastatic size in HNSCC, which may guide clinical decision-making in practice.
Methods
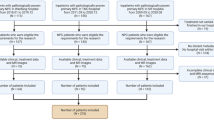
From 2008 to 2022, 171 patients, who were diagnosed as HNSCC in our center, were included. The demographic data, clinicopathological characteristics and lymphatic metastatic size were recorded and analyzed using the Kaplan–Meier method and Cox regression analysis.
Results
Among 171 patients, 107 cases were hypopharyngeal cancer, 38 cases supraglottic cancer and 26 cases oropharyngeal cancer. The median of lymphatic metastatic size was 8 mm (range 0–46). According to lymphatic metastatic size, the patients were assigned to three subgroups: Group I (0 mm), Group II ( ≤ 10 mm) and Group III (> 10 mm). Kaplan–Meier analysis with log rank test revealed that Group I and Group II had similar locoregional control rate, distant metastasis free probability, disease-free survival and overall survival (all p > 0.05), whereas Group III had significant worse prognosis. Adjusted for demographic and other clinicopathological characteristics, lymphatic metastatic size was an independent predictor of disease-free survival and overall survival in HNSCC.
Conclusions
Lymphatic metastatic size was an independently prognostic factor in HNSCC, which may assist in postoperative adjuvant treatment decisions.


Similar content being viewed by others
Data availability
The datasets used during the current study are available in Mendeley Data, V2, https://doi.org/10.17632/7pxm963y3t.2
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108. https://doi.org/10.3322/caac.21262
Shield KD, Ferlay J, Jemal A, Sankaranarayanan R, Chaturvedi AK, Bray F et al (2017) The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA Cancer J Clin 67:51–64. https://doi.org/10.3322/caac.21384
Cerezo L, Millán I, Torre A, Aragón G, Otero J (1992) Prognostic factors for survival and tumor control in cervical lymph node metastases from head and neck cancer. A multivariate study of 492 cases. Cancer 69:1224–1234. https://doi.org/10.1002/cncr.2820690526
Ho AS, Kim S, Tighiouart M, Gudino C, Mita A, Scher KS et al (2017) Metastatic lymph node burden and survival in oral cavity cancer. J Clin Oncol 35:3601–3609. https://doi.org/10.1200/jco.2016.71.1176
Yonemori A, Kondo S, Matsuno Y, Ito T, Nakanishi Y, Miyamoto M et al (2010) Prognostic impact of regional lymph node micrometastasis in patients with node-negative biliary cancer. Ann Surg 252:99–106. https://doi.org/10.1097/SLA.0b013e3181e33c0a
Barresi V, Reggiani Bonetti L, Vitarelli E, Di Gregorio C, de Leon MP, Barresi G (2012) Immunohistochemical assessment of lymphovascular invasion in stage I colorectal carcinoma: prognostic relevance and correlation with nodal micrometastases. Am J Surg Pathol 36:66–72. https://doi.org/10.1097/PAS.0b013e31822d3008
Jeon MJ, Yoon JH, Han JM, Yim JH, Hong SJ, Song DE et al (2013) The prognostic value of the metastatic lymph node ratio and maximal metastatic tumor size in pathological N1a papillary thyroid carcinoma. Eur J Endocrinol 168:219–225. https://doi.org/10.1530/eje-12-0744
Dutta SW, Volaric A, Morgan JT, Chinn Z, Atkins KA, Janowski EM (2019) Pathologic evaluation and prognostic implications of nodal micrometastases in breast cancer. Semin Radiat Oncol 29:102–110. https://doi.org/10.1016/j.semradonc.2018.11.001
Hruban RH, Westra WH, Phelps TH, Isacson C (1996) Surgical pathology dissection
Monica B. Lemos EO (2019) Atlas of surgical pathology grossing (Atlas of Anatomic Pathology) 1st ed. 2019 Edition, pp 11–2
Wang Q, Wang S, Sun Z, Cao M, Zhao X (2022) Evaluation of log odds of positive lymph nodes in predicting the survival of patients with non-small cell lung cancer treated with neoadjuvant therapy and surgery: a SEER cohort-based study. BMC Cancer 22:801. https://doi.org/10.1186/s12885-022-09908-3
Yang J, Huang H, Li W, Ran S, Hu J, Zhang Y et al (2022) A prognostic nomogram based on log odds of positive lymph nodes to predict overall survival for non-metastatic bladder cancer patients after radical cystectomy. Curr Oncol (Toronto, Ont) 29:6834–6846. https://doi.org/10.3390/curroncol29100539
Cao ZX, Weng X, Huang JS, Long X (2022) Prognostic value of LODDS in medullary thyroid carcinoma based on competing risk model and propensity score matching analysis. Updates Surg 74:1551–1562. https://doi.org/10.1007/s13304-022-01320-7
Machens A, Lorenz K, Weber F, Dralle H (2022) Superiority of metastatic lymph node ratio over number of node metastases and TNM/AJCC N classification in predicting cancer-specific survival in medullary thyroid cancer. Head Neck 44:2717–2726. https://doi.org/10.1002/hed.27181
Wang J, Liu Y, Shayan G, Ma Y, Yi J (2022) Lymph node ratio-dependent prognosis stratification and postoperative radiotherapy utilization in T1–2N1 oral cavity carcinoma. Radiother Oncol 172:83–90. https://doi.org/10.1016/j.radonc.2022.05.009
Sato F, Shimada Y, Li Z, Watanabe G, Maeda M, Imamura M (2001) Lymph node micrometastasis and prognosis in patients with oesophageal squamous cell carcinoma. Br J Surg 88:426–432. https://doi.org/10.1046/j.1365-2168.2001.01687.x
Tojima Y, Nagino M, Ebata T, Uesaka K, Kamiya J, Nimura Y (2003) Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Ann Surg 237:201–207. https://doi.org/10.1097/01.Sla.0000048446.18118.Fc
Lang BH, Tang AH, Wong KP, Shek TW, Wan KY, Lo CY (2012) Significance of size of lymph node metastasis on postsurgical stimulated thyroglobulin levels after prophylactic unilateral central neck dissection in papillary thyroid carcinoma. Ann Surg Oncol 19:3472–3478. https://doi.org/10.1245/s10434-012-2385-4
Dhar DK, Yoshimura H, Kinukawa N, Maruyama R, Tachibana M, Kohno H et al (2005) Metastatic lymph node size and colorectal cancer prognosis. J Am Coll Surg 200:20–28. https://doi.org/10.1016/j.jamcollsurg.2004.09.037
Lee YM, Park JH, Cho JW, Hong SJ, Yoon JH (2019) The definition of lymph node micrometastases in pathologic N1a papillary thyroid carcinoma should be revised. Surgery 165:652–656. https://doi.org/10.1016/j.surg.2018.09.015
Andersson Y, Bergkvist L, Frisell J, de Boniface J (2018) Long-term breast cancer survival in relation to the metastatic tumor burden in axillary lymph nodes. Breast Cancer Res Treat 171:359–369. https://doi.org/10.1007/s10549-018-4820-0
Choi KH, Song JH, Hong JH, Lee YS, Kang JH, Sun DI et al (2022) Importance of lymph node ratio in HPV-related oropharyngeal cancer patients treated with surgery and adjuvant treatment. PLoS ONE 17:e0273059. https://doi.org/10.1371/journal.pone.0273059
Kouka M, Al-Ahmar E, Büntzel J, Kaftan H, Böger D, Müller A et al (2022) The log odds of positive neck lymph nodes is a superior lymph node predictor for overall survival in head and neck cancer: a population-based analysis in Germany. Eur Arch Oto-rhino-laryngol 279:3587–3595. https://doi.org/10.1007/s00405-021-07176-8
van den Brekel MW (2000) Lymph node metastases: CT and MRI. Eur J Radiol 33:230–238. https://doi.org/10.1016/s0720-048x(99)00145-x
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No. 82101238) and Guangzhou science and technology project (No. 202201011316).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interest to disclose.
Ethical statement
The study was carried out with approval of the Institutional Review Board (IRB) of Sun Yat-sen Memorial hospital (approval No. SYSKY-2022-449-01).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, W., Lin, P., Li, Z. et al. The prognostic value of lymphatic metastatic size in head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol 281, 387–395 (2024). https://doi.org/10.1007/s00405-023-08199-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08199-z