Abstract
Purpose
Standard treatment for tinnitus is cognitive behavioral therapy, although level of evidence of effectiveness is low. There is need for a Goal Attainment Scale to evaluate treatment effects based on patient satisfaction. Preliminary work in a clinical sample has identified six common personal treatment goals. The purpose of this study is to determine whether the preliminary identified goals are confirmed by a heterogeneous sample of people with bothersome tinnitus and to identify any other common personal goals with the intention to construct a closed-end Goal Attainment Scale for tinnitus for use in research of effectiveness of (new) tinnitus treatments.
Methods
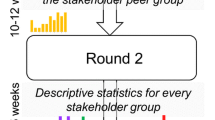
Two consecutive polls were plotted in an online peer support group form a heterogeneous sample. First, members were asked to vote for preliminary identified goals and asked to formulate additional personal goals. Corresponding goals were grouped together. Goals that were acknowledged by at least 10% of respondents were used in the second poll in which respondents could vote for statements that they recognized themselves in.
Results
The first poll (N = 180) resulted in 15 personal treatment goals. Comparison resulted in five common goals, which were confirmed in the second poll (N = 238): to gain control, to improve well-being and sleep, to reduce effects on hearing and to understand tinnitus.
Conclusions
We expect that if a patient achieves personal goals, he will be likely to reduce healthcare consumption. Based on common personal goals, validity of treatment evaluations is increased. We present a closed-end Goal Attainment Scale in tinnitus.



Similar content being viewed by others
References
Henry JA, Dennis KC, Schechter MA (2005) General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res 48(5):1204–1235
McCormack A, Edmondson-Jones M, Somerset S, Hall D (2016) A systematic review of the reporting of tinnitus prevalence and severity. Hear Res 337:70–79
De Ridder D, Vanneste S, Weisz N (2014) An integrative model of auditory phantom perception: tinnitus as a unified percept of interacting separable subnetworks. Neurosci Biobehav Rev 44:16–21
Wagenaar OVG, Schubert NMA, Van Rood YR, Rosmalen JGM (2022) Factors associated with self rated health in persons with tinnitus from the general population. J Psychosom Res 153:110693
Davis A, El Refaie A (2000) The Epidemiology of tinnitus. In: Tyler R (ed) The Handbook of Tinnitus. Singular, pp. 1–23
Kim HJ, Lee HJ, An SY et al (2015) Analysis of the prevalence and associated risk factors of tinnitus in adults. PLoS One 10(5):e0127578
Hoare DJ, Searchfield GD, El Refaie A, Henry JA (2014) Sound therapy for tinnitusmanagement: practicable options. J Am Acad Audiol 25:62–75
Cederroth CR, Kahler AK, Sullivan PF, Lopez-Escamez JA (2017) Genetics of tinnitus: time to biobank phantom sounds. Front Genet 8:110
de Ridder D, Schlee W, Vanneste S et al (2021) Tinnitus and tinnitus disorder: Theoretical and operational definitions (an international multidisciplinary proposal). Prog Brain Res 260:1–25
Mazurek B, Hesse G, Dobel C, Kratzsch V, Lahmann C, Sattel H (2022) Chronic Tinnitus. Dtsch Arztebl Int 119(13):219–225
Gilles A, Jacquemin L, Cardon E et al (2022) Long-term effects of a single psycho-educational session in chronic tinnitus patients. Eur Arch Otorhinolaryngol 279(7):3301–3307. https://doi.org/10.1007/s00405-021-07026-7
Demoen S, Chalimourdas A, Timmermans A et al (2023) Effectiveness of telerehabilitation interventions for self-management of tinnitus: systematic review. J Med Internet Res. 25:e39076. https://doi.org/10.2196/39076
Fuller T, Cima R, Langguth B et al (2020) Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 1(1):CD012614
Cima RFF, Mazurek B, Haider H, Kikidis D, Lapira A, Noreña A, Hoare DJ (2019) A multidisciplinary European guideline for tinnitus: diagnostics, assessment, and treatment. HNO 67(Suppl 1):10–42. https://doi.org/10.1007/s00106-019-0633-7
Jose Santacruz L, Arnold R, Tuinstra J, Stewart RE, van Dijk P (2021) Validation of a Dutch version of the Tinnitus Functional Index in a tertiary referral tinnitus clinic. Heliyon. 7(8):e07733. https://doi.org/10.1016/j.heliyon.2021.e07733
Henry JA, Griest S, Thielman E, McMillan G, Kaelin C, Carlson KF (2016) Tinnitus functional index: development, validation, outcomes research, and clinical application. Hear Res 334:58–64. https://doi.org/10.1016/j.heares.2015.06.004
Vanneste S, To WT, De Ridder D (2011) The psychometric properties of the Tinnitus Handicap Questionnaire in a Dutch-speaking population. Clin Otolaryngol 36(1):9–16. https://doi.org/10.1111/j.1749-4486.2010.02256.x
Newman CW, Sandridge SA, Jacobson GP (1998) Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am Acad Audiol 9(2):153–160
Medical Research Council’s Institute of Hearing Research (1981) Epidemiology of tinnitus. Ciba Found Symp 85:16–34
Kiresuk TJ, Sherman RE (1968) Goal attainment scaling: a general method for evaluating comprehensive community mental health programs. Community Ment Health J 4(6):443–453
Searchfield GD (2006) Hearing aids and tinnitus. In: Tyler R (ed) Tinnitus protocols. Thieme, New York
Dillon H, James A, Ginis J (1997) Client oriented scale of improve- ment (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. J Am Acad Audiol 8:27–43
Saunders GH, Chisolm TH, Abrams HB (2005) Measuring hearing aid outcomes not as easy as it seems. J Rehabil Res Dev 42:157–168
Searchfield GD (2019) A client oriented scale of improvement in tinnitus for therapy goal planning and assessing outcomes. J Am Acad Audiol 30:327–337
Tyler RS, Baker LJ (1983) Difficulties experienced by tinnitus sufferers. J Speech Hear Disord 48:150–154
Ross V, Echevarria KH, Robinson B (1991) Geriatric tinnitus: causes, clinical treatment, and prevention. Gerontol Nurs 17(10):6–11. https://doi.org/10.3928/0098-9134-19911001-04
Funding
This study has not been funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no competing interest.
Ethical approval
This study was not subject to the Medical Research Involving Human Subjects Act (WMO) and, therefore, did not need to undergo a review by an accredited Medical Ethics Review Committee (METC). The research involves human participants, and all procedures performed in the study involving human participants were in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards (JAMA 2000;284:3043–3049). The handling of personal data conformed with the Medical Treatment Agreement Act (WBGO), although a formal treatment relation did not occur. We also complied with the Dutch Act on Implementation of the General Data Protection Regulation (AVG).
Informed consent
All patients were provided with written information concerning the study and were informed to provide consent before their participation in the study by voluntary filling out the online questionnaire.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wagenaar, O., Gilles, A., Van Rompaey, V. et al. Goal Attainment Scale in tinnitus (GAS-T): treatment goal priorities by chronic tinnitus patients in a real-world setting. Eur Arch Otorhinolaryngol 281, 693–700 (2024). https://doi.org/10.1007/s00405-023-08134-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08134-2