Abstract
Objective
To establish a model for predicting the disease-specific survival (DSS) of patients with oral squamous cell carcinoma (OSCC).
Methods
Patients diagnosed with OSCC from the Surveillance, Epidemiology, and End Results (SEER) database were enrolled and randomly divided into development (n = 14,495) and internal validation cohort (n = 9625). Additionally, a cohort from a hospital located in Southeastern China was utilized for external validation (n = 582).
Results
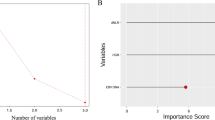
TNM stage, adjuvant treatment, surgery, tumor sites, age, grade, and gender were used for RSF model construction based on the development cohort. The effectiveness of the model was confirmed through time-dependent ROC curves in different cohorts. The risk score exhibited an almost exponential increase in the hazard ratio of death due to OSCC. In development, internal, and external validation cohorts, the prognosis was significantly worse for patients in groups with higher risk scores (all log-rank P < 0.05).
Conclusion
Based on RSF, a high-performance prediction model for OSCC prognosis was created and verified in this study.




Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
References
Goldoni R, Scolaro A, Boccalari E et al (2021) Malignancies and biosensors: a focus on oral cancer detection through salivary biomarkers. Biosensors 11(10):396
Vaidya M, Dmello C, Mogre S (2022) Utility of keratins as biomarkers for human oral precancer and cancer. Life 12(3):343
Ramos DM, But M, Regezi J et al (2002) Expression of integrin β6 enhances invasive behavior in oral squamous cell carcinoma. Matrix Biol 21(3):297–307
Brandizzi D, Gandolfo M, Velazco ML, Cabrini RL, Lanfranchi H (2008) Clinical features and evolution of oral cancer: a study of 274 cases in Buenos Aires, Argentina
Feller L, Lemmer J (2012) Oral squamous cell carcinoma: epidemiology, clinical presentation and treatment
Russo D, Mariani P, Caponio VCA et al (2021) Development and validation of prognostic models for oral squamous cell carcinoma: a systematic review and appraisal of the literature. Cancers 13(22):5755
Amin MB, Greene FL, Edge SB et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67(2):93–99
Oliveira LRD, Ribeiro-Silva A (2011) Prognostic significance of immunohistochemical biomarkers in oral squamous cell carcinoma. Int J Oral Maxillofac Surg 40(3):298–307
Massano J, Regateiro FS, Januário G, Ferreira A (2006) Oral squamous cell carcinoma: review of prognostic and predictive factors. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 102(1):67–76
Oh LJ, Asher R, Veness M et al (2021) Effect of age and gender in non-smokers with oral squamous cell carcinoma: multi-institutional study. Oral Oncol 116:105210
Yasin MM, Abbas Z, Hafeez A (2022) Correlation of histopathological patterns of OSCC patients with tumor site and habits. BMC Oral Health 22(1):1–7
Rai HC, Ahmed J (2016) Clinicopathological correlation study of oral squamous cell carcinoma in a local Indian population. Asian Pac J Cancer Prev 17(3):1251–1254
Dolens EDS, Dourado MR, Almangush A et al (2021) The impact of histopathological features on the prognosis of oral squamous cell carcinoma: a comprehensive review and meta-analysis. Front Oncol 11:784924
Zhang L, Huang T, Xu F et al (2022) Prediction of prognosis in elderly patients with sepsis based on machine learning (random survival forest). BMC Emerg Med 22(1):1–10
Frederick L, Page DL, Fleming ID et al (2002) AJCC cancer staging manual. Springer Science & Business Media, Berlin
Kwak MS, Eun YG, Lee JW, Lee YC (2021) Development of a machine learning model for the prediction of nodal metastasis in early T classification oral squamous cell carcinoma: SEER-based population study. Head Neck 43(8):2316–2324
Wang P, Guo K, Zhang A et al (2021) Survival analysis of age-related oral squamous cell carcinoma: a population study based on SEER
Chen X, Ishwaran H (2012) Random forests for genomic data analysis. Genomics 99(6):323–329
Kreppel M, Drebber U, Rothamel D et al (2011) Prognostic impact of different TNM-based stage groupings for oral squamous cell carcinoma. Head Neck 33(10):1467–1475
Huang SH, Osullivan B (2017) Overview of the 8th edition TNM classification for head and neck cancer. Curr Treat Options Oncol 18(7):1–13
Yoon AJ, Wang S, Kutler DI et al (2020) MicroRNA-based risk scoring system to identify early-stage oral squamous cell carcinoma patients at high-risk for cancer-specific mortality. Head Neck 42(8):1699–1712
Choi K-K, Kim M-J, Yun P-Y et al (2006) Independent prognostic factors of 861 cases of oral squamous cell carcinoma in Korean adults. Oral Oncol 42(2):208–217
Xu Q, Wang C, Li B et al (2019) The impact of age on oral squamous cell carcinoma: a longitudinal cohort study of 2782 patients. Oral Dis 25(3):730–741
Honorato J, Rebelo M, Dias F et al (2015) Gender differences in prognostic factors for oral cancer. Int J Oral Maxillofac Surg 44(10):1205–1211
Xu Q, Wang C, Li B et al (2018) Prognostic value of pathologic grade for patients with oral squamous cell carcinoma. Oral Dis 24(3):335–346
Sklenicka S, Gardiner S, Dierks EJ, Potter BE, Bell RB (2010) Survival analysis and risk factors for recurrence in oral squamous cell carcinoma: does surgical salvage affect outcome? J Oral Maxil Surg 68(6):1270–1275
Rogers SN, Brown JS, Woolgar JA et al (2009) Survival following primary surgery for oral cancer. Oral Oncol 45(3):201–211
Weckx A, Grochau KJ, Grandoch A, Backhaus T, Zöller JE, Kreppel M (2020) Survival outcomes after surgical treatment of oral squamous cell carcinoma. Oral Dis 26(7):1432–1439
Weckx A, Riekert M, Grandoch A, Schick V, Zöller JE, Kreppel M (2019) Time to recurrence and patient survival in recurrent oral squamous cell carcinoma. Oral Oncol 94:8–13
Beltrami C, Desinan L, Rubini C (1992) Prognostic factors in squamous cell carcinoma of the oral cavity: a retrospective study of 80 cases. Pathol-Res Pract 188(4–5):510–516
Zhang Z-Q, He G, Luo Z-W et al (2021) Individual mortality risk predictive system of patients with acute-on-chronic liver failure based on a random survival forest model. Chin Med J 134(14):1701–1708
Miao F, Cai Y-P, Zhang Y-X, Li Y, Zhang Y-T (2015) Risk prediction of one-year mortality in patients with cardiac arrhythmias using random survival forest. Comput Math Methods Med 2015
Mohammed M, Mboya IB, Mwambi H, Elbashir MK, Omolo B (2021) Predictors of colorectal cancer survival using cox regression and random survival forests models based on gene expression data. PLoS ONE 16(12):e0261625
Bohannan ZS, Coffman F, Mitrofanova A (2022) Random survival forest model identifies novel biomarkers of event-free survival in high-risk pediatric acute lymphoblastic leukemia. Comput Struct Biotechnol J 20:583–597
Kattan MW, Hess KR, Beck JR (1998) Experiments to determine whether recursive partitioning (CART) or an artificial neural network overcomes theoretical limitations of Cox proportional hazards regression. Comput Biomed Res 31(5):363–373
Xiao J, Mo M, Wang Z et al (2022) The application and comparison of machine learning models for the prediction of breast cancer prognosis: retrospective cohort study. JMIR Med Inform 10(2):e33440
Lin J, Yin M, Liu L et al (2022) The development of a prediction model based on random survival forest for the postoperative prognosis of pancreatic cancer: a SEER-based study. Cancers 14(19):4667
Acknowledgements
This study was supported by Fujian Natural Science Foundation Program No., Grant/Award Numbers: 2020J01638, 2022J01235 and 2022J01239; Joint Funds for the Innovation of Science and Technology of Fujian Province, Grant/Award Number: 2021Y9015; Open Project of Key Laboratory of environmental factors and Oncology of Fujian Province (GWSZD-202001).
Author information
Authors and Affiliations
Contributions
NW, YLL and HYS: study design, data analysis and interpretation, statistical analysis, and manuscript preparation. FC, FQL, and JW: quality control of data and algorithms and manuscript editing. LLS, WHH, JYH, YQ, and BS: data acquisition. LSL and BCH: study concepts, study design, and manuscript review.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical considerations and consent
It is not necessary to get ethical consent to use patient data in the SEER database since the information is anonymous. For patients in external validation, written informed consent was obtained. This research was conducted according to the ethical standards of the Helsinki Declaration, and the ethical approval was approved by the Ethics Committees of Fujian Medical University, Fuzhou, China (Approval ID: 2011053).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, N., Lin, Y., Song, H. et al. Development and validation of a model for the prediction of disease-specific survival in patients with oral squamous cell carcinoma: based on random survival forest analysis. Eur Arch Otorhinolaryngol 280, 5049–5057 (2023). https://doi.org/10.1007/s00405-023-08087-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08087-6