Abstract
Purpose
To investigate the discriminant ability of the eating assessment tool-10 (EAT-10) to detect postswallow residue and aspiration for different consistencies.
Methods
Seventy-two consecutive patients with mixed etiology of dysphagia (42 males and 30 females, mean ± sd age of 60.42 ± 15.82) were included. After completing the EAT-10, Fiberoptic Endoscopic Evaluation of Swallowing (FEES) was performed to assess the efficiency and safety of swallowing for the following consistencies: thin liquid, nectar thick, yogurt, and solid. While swallowing efficiency was evaluated using the Yale Pharyngeal Residue Severity Rating Scale (YPRSRS), the Penetration–Aspiration Scale (PAS) was used to evaluate swallowing safety.
Results
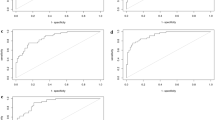
The EAT-10 questionnaire significantly identified the patients with residue from those without residue for the following consistencies and anatomic locations: thin liquid residue in the pyriform sinus (cutoff score ≥ 10, p = 0.009), nectar thick residue in the vallecula (cutoff score ≥ 15, p = 0.001), yogurt residue in the vallecula (cutoff score ≥ 15, p = 0.009), yogurt residue in the pyriform sinus (cutoff score ≥ 9, p = 0.015), and solid residue in the vallecula (cutoff score ≥ 13, p = 0.016). However, the same discriminant ability of EAT-10 was not found for detecting aspiration in any consistency.
Conclusions
The EAT-10 questionnaire can be used as an assessment tool to judge swallowing efficiency in patients with mixed etiology of dysphagia, but the same is not evident for swallowing safety.

Similar content being viewed by others
References
Roden DF, Altman KW (2013) Causes of dysphagia among different age groups: a systematic review of the literature. Otolaryngol Clin North Am 46(6):965–987
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P (2002) Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia 17(2):139–146
Pizzorni N (2017) Social and psychologic impact of dysphagia. dysphagia. Springer, pp 873–886
Altman KW, Yu G-P, Schaefer SD (2010) Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg 136(8):784–789
Blackwell Z, Littlejohns P (2010) A review of the management of dysphagia: a South African perspective. J Neurosci Nurs 42(2):61–70
Kamal RM, Ward E, Cornwell P (2012) Dysphagia management practices among speech-language pathologists in Malaysia. Asia Pac J Speech Lang Hear 15(2):111–128
Rangarathnam B, Desai RV (2020) A preliminary survey of dysphagia practice patterns among speech-language pathologists in India. J Indian Speech Lang Hear Assoc 34(2):259
Gölaç H, İncebay Ö, Aydınlı FE (2022) Investigation of dysphagia education and practice among the speech and language therapists in Turkey: a descriptive cross-sectional Study. Turk Klin J Health Sci 7(3):712–725
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ (2008) Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol 117(12):919–924
Demir N, Arslan SS, İnal Ö, Karaduman AA (2016) Reliability and validity of the Turkish eating assessment tool (T-EAT-10). Dysphagia 31(5):644–649
Plowman EK, Tabor L, Robison R, Gaziano J, Dion C, Watts SA, Vu T, Gooch C (2016) Discriminant ability of the eating assessment tool-10 to detect aspiration in individuals with amyotrophic lateral sclerosis. Neurogastroenterol Motil 28(1):85–90
Shapira-Galitz Y, Yousovich R, Halperin D, Wolf M, Lahav Y, Drendel M (2019) Does the Hebrew eating assessment tool-10 correlate with pharyngeal residue, penetration and aspiration on fiberoptic endoscopic examination of swallowing? Dysphagia 34(3):372–381
Dewan K, Clarke JO, Kamal AN, Nandwani M, Starmer HM (2021) Patient reported outcomes and objective swallowing assessments in a multidisciplinary dysphagia clinic. Laryngoscope 131(5):1088–1094
Florie M, Pilz W, Kremer B, Verhees F, Waltman G, Winkens B, Winter N, Baijens L (2021) EAT-10 scores and Fiberoptic endoscopic evaluation of swallowing in head and neck cancer patients. Laryngoscope 131(1):E45–E51
Neubauer PD, Rademaker AW, Leder SB (2015) The yale pharyngeal residue severity rating scale: an anatomically defined and image-based tool. Dysphagia 30(5):521–528
Atar Y, Atar S, Ilgin C, Anarat MEA, Uygan U, Uyar Y (2022) Validity and reliability of the turkish translation of the yale pharyngeal residue severity rating scale. Dysphagia 37(3):655–663
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL (1996) A penetration-aspiration scale. Dysphagia 11(2):93–98
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37(5):360–363
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47(4):458–472
Arslan SS, Demir N, Kılınç HE, Karaduman AA (2017) The ability of the Eating Assessment Tool-10 to detect aspiration in patients with neurological disorders. J Neurogastroenterol Motil 23(4):550
Cheney DM, Siddiqui MT, Litts JK, Kuhn MA, Belafsky PC (2015) The ability of the 10-item eating assessment tool (EAT-10) to predict aspiration risk in persons with dysphagia. Ann Otol Rhinol Laryngol 124(5):351–354
Printza A, Boziki M, Triaridis S, Kiousi V, Arnaoutoglou M, Constantinidis J, Grigoriadis N (2021) Tongue strength, dysphagia questionnaire, pharyngeal secretions and FEES findings in dysphagia management in amyotrophic lateral sclerosis. Auris Nasus Larynx 48(4):672–682
Donohue C, Tabor Gray L, Anderson A, DiBiase L, Chapin J, Wymer JP, Plowman EK (2022) Discriminant ability of the eating assessment tool-10 to detect swallowing safety and efficiency impairments. Laryngoscope 132(12):2319–2326
Funding
The authors received no financial support for the publication of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest regarding the publication of this manuscript.
Ethical approval
The current study was conducted in accordance with the Declaration of Helsinki, and approved by the Gazi University Clinical Research Ethics Committee (Decision number: 728).
Informed consent
Broad informed consent was obtained from all participants before enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gölaç, H., Atalık, G., Gülaçtı, A. et al. The discriminant ability of the eating assessment tool-10 questionnaire to detect residue and aspiration in patients with mixed etiology of dysphagia. Eur Arch Otorhinolaryngol 280, 3757–3763 (2023). https://doi.org/10.1007/s00405-023-07987-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07987-x