Abstract
Objectives
To analyze the risk factors for synchronous lung metastases (LM) in patients with major salivary gland mucoepidermoid carcinoma (MaSG-MEC).
Methods
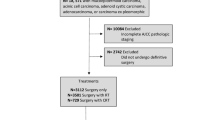
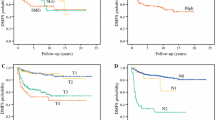
MaSG-MEC patients were extracted from the Surveillance, Epidemiology and End Results (SEER) database between 2010 and 2014. Descriptive statistics were used to examine the baseline characteristics of the patients. We examined the association between risk factors and synchronous LM using Chi-squared tests. The primary study outcomes were overall survival (OS) and cancer-specific survival (CSS). Kaplan–Meier survival curves were compared using the log-rank test. Hazard analysis was conducted using the Cox proportional hazards model. Results: A total of 701 patients were analyzed, which including 8 patients (1.1%) with synchronous LM, and 693 patients without synchronous LM (98.9%). Lower T or N classification, and highly differentiated disease were associated with a significantly lower risk of LM and multivariate logistic regression analysis showed that lower T classification were associated with a significantly lower risk of LM (P < 0.05, respectively). Elderly Caucasian male patients with poorly differentiated disease, multiple sites of metastases and no surgical therapy to primary tumor were more likely to reduce life expectancy.
Conclusion
By analyzing data from a large cohort, lower T or N classification and highly differentiated disease were associated with a significantly lower risk of LM. Elderly Caucasian male patients with poorly differentiated disease, multiple sites of metastases and no surgical therapy to primary tumor were more likely to reduce life expectancy. More accurate assessments of LM will be imperative for early diagnosis and treatment in patients who harbored with higher T or N classification and poorly differentiated disease.

Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Akbaba S, Heusel A, Mock A, Held T, Lang K, Hoerner-Rieber J, Forster T, Katayama S, Kargus S, Rieken S, Plinkert P, Herfarth K, Debus J, Adeberg S (2019) The impact of age on the outcome of patients treated with radiotherapy for mucoepidermoid carcinoma (MEC) of the salivary glands in the head and neck: A 15-year single-center experience. Oral Oncol 97:115–123. https://doi.org/10.1016/j.oraloncology.2019.08.018
Benchetrit L, Mehra S, Mahajan A, Rahmati RW, Judson BL, Edwards HA (2021) Major salivary gland cancer with distant metastasis upon presentation: patterns, outcomes, and imaging implications. Otolaryngol Head Neck Surg: 68848306. Doi: https://doi.org/10.1177/01945998211058354
Brandwein MS, Ivanov K, Wallace DI, Hille JJ, Wang B, Fahmy A, Bodian C, Urken ML, Gnepp DR, Huvos A, Lumerman H, Mills SE (2001) Mucoepidermoid carcinoma: a clinicopathologic study of 80 patients with special reference to histological grading. Am J Surg Pathol 25(7):835–845
Chen AM, Lau VH, Farwell DG, Luu Q, Donald PJ (2013) Mucoepidermoid carcinoma of the parotid gland treated by surgery and postoperative radiation therapy: clinicopathologic correlates of outcome. Laryngoscope 123(12):3049–3055. https://doi.org/10.1002/lary.24238
Eveson JW, Cawson RA (1985) Salivary gland tumours A review of 2410 cases with particular reference to histological types, site, age and sex distribution. J Pathol 146(1):51–58. https://doi.org/10.1002/path.1711460106
Hocwald E, Korkmaz H, Yoo GH, Adsay V, Shibuya TY, Abrams J, Jacobs JR (2001) Prognostic factors in major salivary gland cancer. Laryngoscope 111(8):1434–1439. https://doi.org/10.1097/00005537-200108000-00021
Iqbal H, Bhatti ABH, Hussain R, Jamshed A (2014) Ten Year Experience with Surgery and Radiation in the Management of Malignant Major Salivary Gland Tumors. Asian Pac J Cancer Prev 15(5):2195–2199. https://doi.org/10.7314/APJCP.2014.15.5.2195
Koul R, Dubey A, Butler J, Cooke AL, Abdoh A, Nason R (2007) Prognostic factors depicting disease-specific survival in parotid-gland tumors. Int J Radiat Oncol Biol Phys 68(3):714–718. https://doi.org/10.1016/j.ijrobp.2007.01.009
Li Y, Hu C (2020) Clinicopathological features and outcomes of major salivary gland mucoepidermoid carcinoma: do they vary in different age groups. Transl Cancer Res 9(11):6691–6699. https://doi.org/10.21037/tcr-20-2197
Lima RA, Tavares MR, Dias FL, Kligerman J, Nascimento MF, Barbosa MM, Cernea CR, Soares JR, Santos IC, Salviano S (2005) Clinical prognostic factors in malignant parotid gland tumors. Otolaryngol Head Neck Surg 133(5):702–708. https://doi.org/10.1016/j.otohns.2005.08.001
Liu S, Ow A, Ruan M, Yang W, Zhang C, Wang L, Zhang C (2014) Prognostic factors in primary salivary gland mucoepidermoid carcinoma: an analysis of 376 cases in an Eastern Chinese population. Int J Oral Max Surg 43 (6):667–673. doi: https://doi.org/10.1016/j.ijom.2014.01.008
Lukovic J, Alfaraj FA, Mierzwa ML, Marta GN, Xu W, Su J, Moraes FY, Huang SH, Bratman SV, O Sullivan B, Kim JJ, Ringash JG, Waldron J, de Almeida JR, Goldstein DP, Casper KA, Rosko AJ, Spector ME, Kowalski LP, Hope A, Hosni A (2020) Development and validation of a clinical prediction-score model for distant metastases in major salivary gland carcinoma. Ann Oncol 31 (2):295–301. doi: https://doi.org/10.1016/j.annonc.2019.10.024
Mariano FV, Da Silva SD, Chulan TC, de Almeida OP, Kowalski LP(2011)Clinicopathological factors are predictors of distant metastasis from major salivary gland carcinomas. Int J Oral Max Surg 40 (5):504–509. doi: https://doi.org/10.1016/j.ijom.2010.12.002
Masui T, Uemura H, Ota I, Kimura T, Nishikawa D, Yamanaka T, Yane K, Kitahara T(2021)A study of 24 cases of salivary gland carcinoma with distant metastasis. Molecular and Clinical Oncology 15 (3). doi: https://doi.org/10.3892/mco.2021.2345
Mimica X, McGill M, Hay A, Karassawa Zanoni D, Shah JP, Wong RJ, Ho A, Cohen MA, Patel SG, Ganly I (2020) Distant metastasis of salivary gland cancer: Incidence, management, and outcomes. Cancer-Am Cancer Soc 126 (10):2153–2162. doi: https://doi.org/10.1002/cncr.32792
Park G, Lee S (2018) Postoperative radiotherapy for mucoepidermoid carcinoma of the major salivary glands: long-term results of a single-institution experience. Radiation Oncology Journal 36 (4):317–324. doi: https://doi.org/10.3857/roj.2018.00409
Taylor ZC, Kaya EA, Bunn JD, Guss ZD, Mitchell BJ, Fairbanks RK, Lamoreaux WT, Wagner AE, Peressini BJ, Lee CM(2020)Overall and cause-specific survival for mucoepidermoid carcinoma of the major salivary glands: Analysis of 2210 patients.World Journal of Clinical Oncology 11 (12):1029–1044. 'doi:'https://doi.org/10.5306/wjco.v11.i12.1029
Wang W, Zheng L, Lv X, Cai Z, Zhang J, Zhang J (2021) Clinicopathological Factors are Predictors of Distant Metastases From Salivary Gland Carcinoma After Surgery Combined With 125I Internal Brachytherapy. J Oral Maxil Surg 79 (7):1557–1563. doi: https://doi.org/10.1016/j.joms.2021.01.005
Funding
The study was funded by the Clinical research on health industry of Shanghai Health Commission (grant numbers: 20214Y0025). The study was funded by the Clinical research of Shanghai Pudong District Health Commission (grant numbers: PW2022A-41).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of XXX Ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The experimental protocols were also approved by XXX Ethics committee. Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Y., Hu, C. Epidemiological and clinical characteristics of synchronous lung metastasis in major salivary gland mucoepidermoid carcinoma. Eur Arch Otorhinolaryngol 280, 3835–3841 (2023). https://doi.org/10.1007/s00405-023-07963-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07963-5