Abstract
Purpose
Head rotation is an effective positional therapy for obstructive sleep apnea (OSA). However, not all OSA patients benefit from head rotation. This study aimed to explore the clinical phenotype of OSA patients who can benefit from head rotation.
Methods
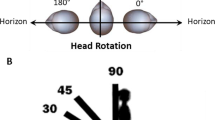
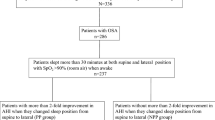
We performed a retrospective review of 184 consecutive OSA patients who underwent polysomnography. Head rotation in supine position was determined by high-quality video recording. According to the changes in apnea–hypopnea index (AHI) after head rotation, OSA patients were divided into two groups: patients with response to head rotation(HR) and patients without response to head rotation(NHR). Demographic factors and overnight polysomnography were analyzed.
Results
Compared with NHR group, HR group showed significantly lower AHI (51.8 vs 31.5, p < 0.01), time spent with oxygen saturation below 90%(5.3% vs 0.51%, p < 0.01), and higher lowest oxygen saturation(80% vs 86%, p < 0.05). Logistic regression showed that AHI was an independent factor to predict the decrease of AHI in head rotation (OR 0.985, 95% CI 0.970–0.979, p < 0.05). Among mild to moderate group (AHI < 30/h), severe group (30/h ≤ AHI < 60/h), and extremely severe group (AHI ≥ 60/h), the percentage decrease of AHI in head rotation was 18.5%, 9.5%, and 2.6%, respectively. Surprisingly, the percentage decrease of AHI of 6 responders in mild to moderate group was more than 50%.
Conclusion
OSA patients who respond well to head rotation have less severe disease, and patients with mild to moderate OSA are more likely to improve and benefit from this position. Our research provides potential strategies and insights into the individual treatment of OSA patients.




Similar content being viewed by others
Data availability
Data is not available due to ethical restrictions.
References
Benjafield AV, Ayas NT et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698. https://doi.org/10.1016/s2213-2600(19)30198-5
Vries GED, Hoekema A et al (2015) Usage of positional therapy in adults with obstructive sleep apnea. J Clin Sleep Med 11:131–137. https://doi.org/10.5664/jcsm.4458
Permut I, Diaz-Abad M et al (2010) Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med JCSM 6:238–243
Dauvilliers Y, Verbraecken J et al (2020) Pitolisant for daytime sleepiness in patients with obstructive sleep apnea who refuse continuous positive airway pressure treatment. a randomized trial. Am J Respir Crit Care Med 201:1135–1145. https://doi.org/10.1164/rccm.201907-1284OC
Joosten SA, O’Driscoll DM et al (2014) Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev 18:7–17. https://doi.org/10.1016/j.smrv.2013.01.005
Zhu K, Bradley TD et al (2017) Influence of head position on obstructive sleep apnea severity. Sleep Breath 21:821–828. https://doi.org/10.1007/s11325-017-1525-2
Tate A, Kurup V et al (2021) Influence of head flexion and rotation on obstructive sleep apnea severity during supine sleep. J Sleep Res 30:e13286. https://doi.org/10.1111/jsr.13286
Tan SN, Kim JM et al (2022) Head rotation improves airway obstruction, especially in patients with less severe obstructive sleep apnea without oropharyngeal collapse. PLoS ONE 17:e0268455. https://doi.org/10.1371/journal.pone.0268455
Safiruddin F, Koutsourelakis I, de Vries N (2014) Analysis of the influence of head rotation during drug-induced sleep endoscopy in obstructive sleep apnea. Laryngoscope 124:2195–2199. https://doi.org/10.1002/lary.24598
Bignold James J, Mercer Jeremy D et al (2011) Accurate position monitoring and improved supine-dependent obstructive sleep apnea with a new position recording and supine avoidance device. J Clin Sleep Med 07:376–383. https://doi.org/10.5664/JCSM.1194
Berry RB, Brooks R et al (2017) AASM scoring manual updates for 2017 (version 2.4). J Clin Sleep Med 13:665–666. https://doi.org/10.5664/jcsm.6576
van Kesteren ER, van Maanen JP et al (2011) Quantitative effects of trunk and head position on the apnea hypopnea index in obstructive sleep apnea. Sleep 34:1075–1081. https://doi.org/10.5665/SLEEP.1164
Randerath WJ, Verbraecken J et al (2011) Non-CPAP therapies in obstructive sleep apnoea. Eur Respir J 37:1000–1028. https://doi.org/10.1183/09031936.00099710
Safiruddin F, Koutsourelakis I, de Vries N (2015) Upper airway collapse during drug induced sleep endoscopy: head rotation in supine position compared with lateral head and trunk position. Eur Arch Otorhinolaryngol 272:485–488. https://doi.org/10.1007/s00405-014-3215-z
Sung CM, Tan SN et al (2021) The site of airway collapse in sleep apnea, its associations with disease severity and obesity, and implications for mechanical interventions. Am J Respir Crit Care Med 204:103–106. https://doi.org/10.1164/rccm.202011-4266LE
Acknowledgements
We thank all the patients and the staff from the Department of Otolaryngology and sleep medical center, Beijing Anzhen Hospital, China, who have participated in this study.
Author information
Authors and Affiliations
Contributions
JD designed the experimental apparatus, discussed the results and implications, and commented on the manuscript at all stages. JD performed the experiments. The research direction was provided by HZ and RG. HS helped to check the English.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The Medical Ethics Committee of Beijing Anzhen Hospital (No. 2017063X) approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, J., Sun, H., Zhang, H. et al. The effect of head rotation on OSA is associated with disease severity: a cross-sectional study. Eur Arch Otorhinolaryngol 280, 3279–3285 (2023). https://doi.org/10.1007/s00405-023-07860-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07860-x