Abstract
Objectives
Sudden sensorineural hearing loss (SSNHL) is one of the common emergencies in otorhinolaryngology. Several studies have shown that chronic inflammation is associated with its onset and prognosis. However, the association between some inflammatory biomarkers and SSNHL is still unclear. Therefore, we conducted this meta-analysis to explore the value of inflammatory biomarkers in the occurrence and prognosis of SSNHL.
Methods
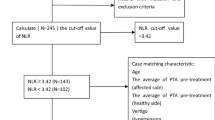
Pubmed, Embase, Cochrane and Web of Science databases were searched comprehensively, the eligible literatures were screened out by formulating the inclusion criteria and exclusion criteria. After extracting sample size, mean and standard deviation, we performed meta-analysis with standardized mean deviation (SMD) and 95% confidence interval (CI) as effect sizes.
Results
A total of 17 articles were included in this meta-analysis, including 2852 subjects, 1423 patients and 1429 healthy controls. The results of meta-analysis showed that the neutrophil-to-lymphocyte ratio (NLR) of the experimental group was significantly higher than the control group (SMD = 1.05, 95% CI 0.87–1.24, P < 0.001), the NLR of the recovery group was significantly lower than the unrecovered group (SMD = 0.68, 95% CI 0.27–1.08, P < 0.05); The platelet-to-lymphocyte ratio (PLR) of the experimental group was significantly higher than the control group (SMD = 0.55, 95% CI 0.34–0.76, P < 0.05), the PLR of the recovery group was significantly lower than the unrecovered group (SMD = 0.44, 95% CI 0.05–0.82, P < 0.05); The C-reactive protein-to-serum albumin ratio (CRP/Alb) of the experimental group was significantly higher than the control group (SMD = 0.39, 95% CI 0.04–0.74, P < 0.05).
Conclusions
The results showed that high NLR, PLR, and CRP/Alb indicated the occurrence of SSNHL, NLR and PLR could predict prognosis of SSNHL.






Similar content being viewed by others
Availability of data and materials
The data sets used and analyzed during the current study are available from references on reasonable request.
References
Chandrasekhar SS, Tsai Do BS, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA, Hollingsworth DB, Kelley DM, Kmucha ST, Moonis G, Poling GL, Roberts JK, Stachler RJ, Zeitler DM, Corrigan MD, Nnacheta LC, Satterfield L, Monjur TM (2019) Clinical practice guideline: sudden hearing loss (Update) executive summary. Otolaryngol Head Neck Surg 161(2):195–210. https://doi.org/10.1177/0194599819859883
Jeon SY, Kang DW, Kim SH, Byun JY, Yeo SG (2022) Prognostic factors associated with recovery from recurrent idiopathic sudden sensorineural hearing loss: retrospective analysis and systematic review. J Clin Med. https://doi.org/10.3390/jcm11051453
Masuda M, Kanzaki S, Minami S, Kikuchi J, Kanzaki J, Sato H, Ogawa K (2012) Correlations of inflammatory biomarkers with the onset and prognosis of idiopathic sudden sensorineural hearing loss. Otol Neurotol 33(7):1142–1150. https://doi.org/10.1097/MAO.0b013e3182635417
Chen L, Zhang G, Zhang Z, Wang Y, Hu L, Wu J (2018) Neutrophil-to-lymphocyte ratio predicts diagnosis and prognosis of idiopathic sudden sensorineural hearing loss: A systematic review and meta-analysis. Medicine (Baltimore) 97(38):e12492. https://doi.org/10.1097/md.0000000000012492
Gates GA, Mills JH (2005) Presbycusis. The lancet 366(9491):1111–1120
Fischer ME, Schubert CR, Nondahl DM, Dalton DS, Huang GH, Keating BJ, Klein BE, Klein R, Tweed TS, Cruickshanks KJ (2015) Subclinical atherosclerosis and increased risk of hearing impairment. Atherosclerosis 238(2):344–349. https://doi.org/10.1016/j.atherosclerosis.2014.12.031
Berjis N, Moeinimehr M, Hashemi SM, Hashemi SM, Bakhtiari EK, Nasiri S (2016) Endothelial dysfunction in patients with sudden sensorineural hearing loss. Adv Biomed Res 5:5. https://doi.org/10.4103/2277-9175.174978
Cao Z, Li Z, Xiang H, Huang S, Gao J, Zhan X, Zheng X, Li B, Wu J, Chen B (2018) Prognostic role of haematological indices in sudden sensorineural hearing loss: review and meta-analysis. Clin Chim Acta 483:104–111. https://doi.org/10.1016/j.cca.2018.04.025
Merchant SN, Durand ML, Adams JC (2008) Sudden deafness: is it viral? Orl 70(1):52–62
Hiramatsu M, Teranishi M, Uchida Y, Nishio N, Suzuki H, Kato K, Otake H, Yoshida T, Tagaya M, Suzuki H (2012) Polymorphisms in genes involved in inflammatory pathways in patients with sudden sensorineural hearing loss. J Neurogenet 26(3–4):387–396
Rudack C, Langer C, Junker R (2004) Platelet GPIaC807T polymorphism is associated with negative outcome of sudden hearing loss. Hear Res 191(1–2):41–48. https://doi.org/10.1016/j.heares.2004.01.002
Varol E, Aksoy F, Ozaydin M, Erdogan D, Dogan A (2013) Relationship between mean platelet volume and mitral annular calcification. Blood Coagul Fibrinolysis 24(2):189–193. https://doi.org/10.1097/MBC.0b013e32835b7296
Liao Y, Liu K, Zhu L (2022) Emerging roles of inflammasomes in cardiovascular diseases. Front Immunol 13:834289. https://doi.org/10.3389/fimmu.2022.834289
Booka E, Kikuchi H, Haneda R, Soneda W, Kawata S, Murakami T, Matsumoto T, Hiramatsu Y, Takeuchi H (2022) Neutrophil-to-lymphocyte ratio to predict the efficacy of immune checkpoint inhibitor in upper gastrointestinal cancer. Anticancer Res 42(6):2977–2987. https://doi.org/10.21873/anticanres.15781
WiraWiguna IGW, IndraniRemitha NPS, Sadvika I, Wiranata S, Putra I, Adiputra PAT, Supadmanaba IGP, Wihandani DM (2022) Pretreatment leukocyte count ratios as metastatic predictive factors in luminal type breast cancer. Asian Pac J Cancer Prev 23(5):1595–1601. https://doi.org/10.31557/apjcp.2022.23.5.1595
Leng J, Wu F, Zhang L (2022) Prognostic significance of pretreatment neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, or monocyte-to-lymphocyte ratio in endometrial neoplasms: a systematic review and meta-analysis. Front Oncol 12:734948. https://doi.org/10.3389/fonc.2022.734948
Ulu S, Ulu MS, Bucak A, Ahsen A, Yucedag F, Aycicek A (2013) Neutrophil-to-lymphocyte ratio as a new, quick, and reliable indicator for predicting diagnosis and prognosis of idiopathic sudden sensorineural hearing loss. Otol Neurotol 34(8):1400–1404. https://doi.org/10.1097/MAO.0b013e31829b57df
Taşoğlu İ, Sert D, Colak N, Uzun A, Songur M, Ecevit A (2014) Neutrophil-lymphocyte ratio and the platelet-lymphocyte ratio predict the limb survival in critical limb ischemia. Clin Appl Thromb Hemost 20(6):645–650. https://doi.org/10.1177/1076029613475474
Koçak HE, Elbistanlı MS, Acıpayam H, Alakras WME, Kıral MN, Kayhan FT (2017) Are neutrophil/lymphocyte and platelet/lymphocyte ratios related with formation of sudden hearing loss and its prognosis? Eur Ann Otorhinolaryngol Head Neck Dis 134(6):383–386. https://doi.org/10.1016/j.anorl.2016.06.005
Ha R, Lim BW, Kim DH, Park JW, Cho CH, Lee JH (2019) Predictive values of neutroph il to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), and other prognostic factors in pediatric idiopathic sudden sensorineural hearing loss. Int J Pediatr Otorhino laryngol 120:134–139. https://doi.org/10.1016/j.ijporl.2019.02.023
Seo YJ, Jeong JH, Choi JY, Moon IS (2014) Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio: novel markers for diagnosis and prognosis in patients with idiopathic sudden sensorineural hearing loss. Dis Mark. https://doi.org/10.1155/2014/702807
Liu X, Sun X, Liu J, Kong P, Chen S, Zhan Y, Xu D (2015) Preoperative C-reactive protein/albumin ratio predicts prognosis of patients after curative resection for gastric cancer. Transl Oncol 8(4):339–345. https://doi.org/10.1016/j.tranon.2015.06.006
Kaplan M, Ates I, Akpinar MY, Yuksel M, Kuzu UB, Kacar S, Coskun O, Kayacetin E (2017) Predictive value of C-reactive protein/albumin ratio in acute pancreatitis. Hepatobil Pancreat Dis Int 16(4):424–430. https://doi.org/10.1016/s1499-3872(17)60007-9
Öçal R, Akın Öçal FC, Güllüev M, Alataş N (2020) Is the C-reactive protein/albumin ratioa prognostic and predictive factor in sudden hearing loss? Braz J Otorhinolaryngol 86(2):180–184. https://doi.org/10.1016/j.bjorl.2018.10.007
Özler GS (2014) Increased neutrophil-lymphocyte ratio in patients with idiopathic sudden sensorineural hearing loss. J Craniofac Surg 25(3):e260-263. https://doi.org/10.1097/scs.0000000000000565
İkincioğulları A, Köseoğlu S, Kılıç M, Atan D, Özcan KM, Çetin MA, Ensari S, Dere HH (2014) New inflammation parameters in sudden sensorineural hearing loss: neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. Int Adv Otol 10(3):197–200
Kum RO, Ozcan M, Baklaci D, Yurtsever Kum N, Yilmaz YF, Unal A, Avci Y (2015) Investigation of neutrophil-to-lymphocyte ratio and mean platelet volume in sudden hearing loss. Braz J Otorhinolaryngol 81(6):636–641. https://doi.org/10.1016/j.bjorl.2015.08.009
Durmuş K, Terzi H, Karataş TD, Doğan M, Uysal I, Şencan M, Altuntaş EE (2016) Assessment of hematological factors involved in development and prognosis of idiopathic sudden sensorineural hearing loss. J Craniofac Surg 27(1):e85-91. https://doi.org/10.1097/scs.0000000000002241
Nonoyama H, Tanigawa T, Shibata R, Nakao Y, Horibe Y, Katahira N, Nishimura K, Murotani K, Murohara T, Ueda H (2016) Red blood cell distribution width predicts prognosis in idiopathic sudden sensorineural hearing loss. Acta Otolaryngol 136(11):1137–1140. https://doi.org/10.1080/00016489.2016.1195919
Lee JS, Hong SK, Kim DH, Lee JH, Lee HJ, Park B, Choi HG, Kong IG, Song HJ, Kim HJ (2017) The neutrophil-to-lymphocyte ratio in children with sudden sensorineural hearing loss: a retrospective study. Acta Otolaryngol 137(1):35–38. https://doi.org/10.1080/00016489.2016.1217561
Bulğurcu S, Dikilitaş B, Arslan İB, Çukurova İ (2017) Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in pediatric patients with idiopathic sudden hearing loss. J Int Adv Otol 13(2):217–220. https://doi.org/10.5152/iao.2017.3404
Qiao XF, Li X, Wang GP, Bai YH, Zheng W, Li TL (2019) Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with sudden sensorineural hearing loss. Med Princ Pract 28(1):23–27. https://doi.org/10.1159/000494556
Sancaktar ME, Ağrı İ, Çeçen AB, Akgül G, Çelebi M (2020) The prognostic value of circulating inflammatory cell counts in sudden sensorineural hearing loss and the effect of cardiovascular risk factors. Ear Nose Throat J 99(7):464–469. https://doi.org/10.1177/0145561320920968
Cayir S, Kayabasi S, Hizli O (2021) Predictor parameters for poor prognosis in patients with sudden sensorineural hearing loss: fibrinogen to albumin ratio vs C-reactive protein to albumin ratio. Braz J Otorhinolaryngol 87(4):457–461. https://doi.org/10.1016/j.bjorl.2020.06.010
Çiçek T, ÖzbilenAcar G, Özdamar O (2021) Evaluation of neutrophil/lymphocyte and platelet/lymphocyte ratios in sudden sensorineural hearing loss and relationship with hyperbaric oxygen therapy. J Int Adv Otol 17(2):96–102. https://doi.org/10.5152/iao.2020.7943
Guo Y, Liu J (2021) The roles played by blood inflammatory parameters in sudden sensorineural hearing loss. Ear Nose Throat J. https://doi.org/10.1177/0145561320960355
Shi X, Dong Y, Li Y, Zhao Z, Li H, Qiu S, Li Y, Guo W, Qiao Y (2015) Inflammasome activation in mouse inner ear in response to MCMV induced hearing loss. J Otol 10(4):143–149. https://doi.org/10.1016/j.joto.2015.12.001
Capaccio P, Pignataro L, Gaini LM, Sigismund PE, Novembrino C, De Giuseppe R, Uva V, Tripodi A, Bamonti F (2012) Unbalanced oxidative status in idiopathic sudden sensorineural hearing loss. Eur Arch Otorhinolaryngol 269(2):449–453. https://doi.org/10.1007/s00405-011-1671-2
Gul F, Muderris T, Yalciner G, Sevil E, Bercin S, Ergin M, Babademez MA, Kiris M (2017) A comprehensive study of oxidative stress in sudden hearing loss. Eur Arch Otorhinolaryngol 274(3):1301–1308. https://doi.org/10.1007/s00405-016-4301-1
Guo Y, Zhang C, Du X, Nair U, Yoo TJ (2005) Morphological and functional alterations of the cochlea in apolipoprotein E gene deficient mice. Hear Res 208(1–2):54–67. https://doi.org/10.1016/j.heares.2005.05.010
Mutlu A, Cam I, Dasli S, Topdag M (2018) Doppler ultrasonography can be useful to determine the etiology of idiopathic sudden sensorineural hearing loss. Auris Nasus Larynx 45(3):456–460. https://doi.org/10.1016/j.anl.2017.08.013
Trune DR, Nguyen-Huynh A (2012) Vascular pathophysiology in hearing disorders. Semin Hear 33(3):242–250. https://doi.org/10.1055/s-0032-1315723
Li X, Chen B, Zhou X, Ye F, Wang Y, Hu W (2021) Identification of dyslipidemia as a risk factor for sudden sensorineural hearing loss: a multicenter case-control study. J Clin Lab Anal 35(12):e24067. https://doi.org/10.1002/jcla.24067
Shao M, Xiong G, Xiang G, Xu S, Zhang L (2021) Correlation between serum lipid and prognosis of idiopathic sudden sensorineural hearing loss: a prospective cohort study. Ann Transl Med 9(8):676. https://doi.org/10.21037/atm-21-907
Hesse G (2016) [Inner ear hearing loss part II: sudden sensorineural hearing loss]. Therapeutic options. Laryngorhinootologie 95(7):461–469. https://doi.org/10.1055/s-0042-108379
Zhou T, Zhan J, Hong S, Hu Z, Fang W, Qin T, Ma Y, Yang Y, He X, Zhao Y, Huang Y, Zhao H, Zhang L (2015) Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep 5:10481. https://doi.org/10.1038/srep10481
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, Fushiya N, Koike K, Nishino H, Matsushima M (2015) The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol 22(3):803–810. https://doi.org/10.1245/s10434-014-4048-0
Ni W, Song SP, Jiang YD (2021) Association between routine hematological parameters and sudden sensorineural hearing loss: a meta-analysis. J Otol 16(1):47–54. https://doi.org/10.1016/j.joto.2020.07.006
Acknowledgements
We would like to thank Professor Zhenhua Zhong and Dr Maohua Wang for reviewing and providing advice on the final search strategy. We thank LetPub (https: //www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Funding
This work was supported by grants from Jiangsu Province Natural Science Foundation (BK20181221, BK20201220), Doctoral Startup Foundation (2021BS-ZZH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, L., Wang, M., Zhang, W. et al. The value of inflammatory biomarkers in the occurrence and prognosis of sudden sensorineural hearing loss: a meta-analysis. Eur Arch Otorhinolaryngol 280, 3119–3129 (2023). https://doi.org/10.1007/s00405-022-07806-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07806-9