Abstract
Purpose
To explore the diagnostic auditory indicators of high noise exposure and combine them into a diagnostic model of high noise exposure and possible development of hidden hearing loss (HHL).
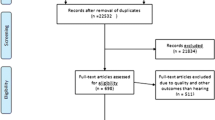
Methods
We recruited 101 young adult subjects and divided them according to noise exposure history into high-risk and low-risk groups. All subjects completed demographic characteristic collection (including age, noise exposure, self-reported hearing status, and headset use) and related hearing examination.
Results
The 8 kHz (P = 0.039) and 10 kHz (P = 0.005) distortion product otoacoustic emission amplitudes (DPOAE) (DPs) in the high-risk group were lower than those in the low-risk group. The amplitudes of the summating potential (SP) (P = 0.017) and action potential (AP) (P = 0.012) of the electrocochleography (ECochG) in the high-risk group were smaller than those in the low-risk group. The auditory brainstem response (ABR) wave III amplitude in the high-risk group was higher than that in the low-risk group. When SNR = − 7.5 dB (P = 0.030) and − 5 dB (P = 0.000), the high-risk group had a lower speech discrimination score than that of the low-risk group. The 10 kHz DPOAE DP, ABR wave III amplitude and speech discrimination score under noise with SNR = − 5 dB were combined to construct a combination diagnostic indicator. The area under the ROC curve was 0.804 (95% CI 0.713–0.876), the sensitivity was 80.39%, and the specificity was 68.00%.
Conclusions
We expect that high noise exposure can be detected early with this combined diagnostic indicator to prevent HHL or sensorineural hearing loss (SNHL).
Trial registration number/date of registration
ChiCTR2200057989, 2022/3/25.



Similar content being viewed by others
Data availability
The data used to support the findings of this study are available on request to the corresponding author: Lian-Jun Lu, E-mail: lulianj@fmmu.edu.cn.
References
World report on hearing. ISBN 978-92-4-002048-1. https://www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/highlighting-priorities-for-ear-and-hearing-care
Nordvik Ø, LaugenHeggdal PO, Brännström J, Vassbotn F, Aarstad AK, Aarstad HJ (2018) Generic quality of life in persons with hearing loss: a systematic literature review. BMC Ear Nose Throat Disord 18:1. https://doi.org/10.1186/s12901-018-0051-6
Olusanya BO, Neumann KJ, Saunders JE (2014) The global burden of disabling hearing impairment: a call to action. Bull World Health Organ 92:367–373. https://doi.org/10.2471/blt.13.128728
Masterson EA, Themann CL, Luckhaupt SE, Li J, Calvert GM (2016) Hearing difficulty and tinnitus among U.S. workers and non-workers in 2007. Am J Ind Med 59:290–300. https://doi.org/10.1002/ajim.22565
Kujawa SG, Liberman MC (2009) Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci 29:14077–14085. https://doi.org/10.1523/jneurosci.2845-09.2009
Schaette R, McAlpine D (2011) Tinnitus with a normal audiogram: physiological evidence for hidden hearing loss and computational model. J Neurosci 31:13452–13457. https://doi.org/10.1523/jneurosci.2156-11.2011
Spankovich C, Gonzalez VB, Su D, Bishop CE (2018) Self reported hearing difficulty, tinnitus, and normal audiometric thresholds, the National Health and Nutrition Examination Survey 1999–2002. Hear Res 358:30–36. https://doi.org/10.1016/j.heares.2017.12.001
Liberman MC, Epstein MJ, Cleveland SS, Wang H, Maison SF (2016) Toward a differential diagnosis of hidden hearing loss in humans. PLoS ONE 11:e0162726. https://doi.org/10.1371/journal.pone.0162726
Grose JH, Buss E, Hall JW 3rd (2017) Loud music exposure and cochlear synaptopathy in young adults: isolated auditory brainstem response effects but no perceptual consequences. Trends Hear 21:2331216517737417. https://doi.org/10.1177/2331216517737417
Lokwani P, Prabhu P (2022) Efficacy of behavioral audiological tests in identifying cochlear synaptopathy: a systematic review. Eur Arch Otorhinolaryngol 279:577–594. https://doi.org/10.1007/s00405-021-06927-x
Ck D, Wan G, Cassinotti L, Corfas G (2020) Hidden hearing loss: a disorder with multiple etiologies and mechanisms. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a035493
Bal N, Derinsu U (2021) The possibility of cochlear synaptopathy in young people using a personal listening device. Auris Nasus Larynx 48:1092–1098. https://doi.org/10.1016/j.anl.2021.03.015
Marmel F, Cortese D, Kluk K (2020) The ongoing search for cochlear synaptopathy in humans: masked thresholds for brief tones in Threshold Equalizing Noise. Hear Res 392:107960. https://doi.org/10.1016/j.heares.2020.107960
Yamashita D, Jiang HY, Schacht J, Miller JM (2004) Delayed production of free radicals following noise exposure. Brain Res 1019:201–209. https://doi.org/10.1016/j.brainres.2004.05.104
Gorga MP, Neely ST, Bergman B, Beauchaine KL, Kaminski JR, Peters J, Jesteadt W (1993) Otoacoustic emissions from normal-hearing and hearing-impaired subjects: distortion product responses. J Acoust Soc Am 93:2050–2060. https://doi.org/10.1121/1.406691
Gorga MP, Neely ST, Ohlrich B, Hoover B, Redner J, Peters J (1997) From laboratory to clinic: a large scale study of distortion product otoacoustic emissions in ears with normal hearing and ears with hearing loss. Ear Hear 18:440–455. https://doi.org/10.1097/00003446-199712000-00003
Pappa AK, Hutson KA, Scott WC, Wilson JD, Fox KE, Masood MM, Giardina CK, Pulver SH, Grana GD, Askew C et al (2019) Hair cell and neural contributions to the cochlear summating potential. J Neurophysiol 121:2163–2180. https://doi.org/10.1152/jn.00006.2019
Mulders W, Chin IL, Robertson D (2018) Persistent hair cell malfunction contributes to hidden hearing loss. Hear Res 361:45–51. https://doi.org/10.1016/j.heares.2018.02.001
Patuzzi RB, Yates GK, Johnstone BM (1989) Changes in cochlear microphonic and neural sensitivity produced by acoustic trauma. Hear Res 39:189–202. https://doi.org/10.1016/0378-5955(89)90090-7
Barbee CM, James JA, Park JH, Smith EM, Johnson CE, Clifton S, Danhauer JL (2018) Effectiveness of auditory measures for detecting hidden hearing loss and/or cochlear synaptopathy: a systematic review. Semin Hear 39:172–209. https://doi.org/10.1055/s-0038-1641743
Bramhall NF, Konrad-Martin D, McMillan GP, Griest SE (2017) Auditory brainstem response altered in humans with noise exposure despite normal outer hair cell function. Ear Hear 38:e1–e12. https://doi.org/10.1097/aud.0000000000000370
Prendergast G, Guest H, Munro KJ, Kluk K, Léger A, Hall DA, Heinz MG, Plack CJ (2017) Effects of noise exposure on young adults with normal audiograms I: Electrophysiology. Hear Res 344:68–81. https://doi.org/10.1016/j.heares.2016.10.028
Lauter JL, Loomis RL (1988) Individual differences in auditory electric responses: comparisons of between-subject and within-subject variability. II. Amplitude of brainstem Vertex-positive peaks. Scand Audiol 17:87–92. https://doi.org/10.3109/01050398809070696
Nam GS, Kim JY, Hong SA, Kim SG, Son EJ (2021) Limitation of conventional audiometry in identifying hidden hearing loss in acute noise exposure. Yonsei Med J 62:615–621. https://doi.org/10.3349/ymj.2021.62.7.615
Hall JW (2007) New handbook of auditory evoked responses. Pearson Boston, Mass., London
Acknowledgements
We would like to thank all participants for their time during this study.
Funding
This work was supported by funding from the Military Logistics Research Project of China [18CXZ015].
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by P-WM, J-WC, W-LW, WG, P-HL, X-RD, Y-QL. The first draft of the manuscript was written by HY, P-WM, J-WC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of Tangdu Hospital of Air Force Military Medical University (No. K202112-16).
Consent
All information is anonymized and the submission does not include images that may identify the person.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuan, H., Ma, PW., Chen, JW. et al. Development of an audiological assessment and diagnostic model for high occupational noise exposure. Eur Arch Otorhinolaryngol 280, 2763–2772 (2023). https://doi.org/10.1007/s00405-022-07787-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07787-9