Abstract
Objectives
This study aimed to determine the readmission rate after adenotonsillectomy with the diagnosis of obstructive sleep apnea (OSA) and analyze the factors associated with readmission.
Methods
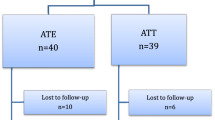
It was planned as a retrospective study conducted in a single institution that included pediatric patients who underwent adenotonsillectomy with OSA diagnosis between December 2018 and March 2021. Patients who were readmitted for bleeding or pain/dehydration were compared with those who did not require readmission.
Results
The mean postoperative admission time was 7.27 ± 3.49 days in patients with bleeding and 3.5 ± 2.27 days in patients with pain or dehydration. The mean length of stay in the hospital was 2.6 ± 1.6 days in patients with bleeding and 3.13 ± 2.03 days in patients with pain or dehydration. The postoperative admission time was 5.96 ± 3.57 days, and the hospital stay after readmission was 2.78 ± 1.73 days. No statistically significant correlation was found in terms of age, gender, surgeon's experience, use of electrocautery and seasonality factors, and readmission rates.
Conclusions
In children who underwent adenotonsillectomy for OSA, the hospitalization period of patients hospitalized due to pain/dehydration is much longer than patients admitted with bleeding. Therefore, measures to reduce pain or dehydration have the most significant potential to reduce the readmission rate and length of stay.


Similar content being viewed by others
References
Šujanská A, Ďurdík P, Rabasco J, Vitelli O, Pietropaoli N, Villa MP (2014) Surgical and non-surgıcal therapy of obstructive sleep apnea syndrome in children. Acta Medica Hradec Kralove Czech Repub 57:135–141. https://doi.org/10.14712/18059694.2015.78
Cielo CM, Gungor A (2016) Treatment options for pediatric obstructive sleep apnea. Curr Probl Pediatr Adolesc Health Care 46:27–33. https://doi.org/10.1016/j.cppeds.2015.10.006
Lloyd AM, Behzadpour HK, Schonman I, Rana MS, Espinel AG (2021) Socioeconomic factors associated with readmission following pediatric tonsillectomy. Int J Pediatr Otorhinolaryngol 151:110917. https://doi.org/10.1016/j.ijporl.2021.110917
Hession-Laband E, Melvin P, Shermont H, Murphy JM, Bukoye B, Amin M (2018) Reducing readmissions post-tonsillectomy: a quality improvement study on intravenous hydration. J Healthc Qual 40:217–227. https://doi.org/10.1097/JHQ.0000000000000143
Johnson RF, Chang A, Mitchell RB (2018) Nationwide readmissions after tonsillectomy among pediatric patients—United States. Int J Pediatr Otorhinolaryngol 107:10–13. https://doi.org/10.1016/j.ijporl.2018.01.026
Geißler K, Rippe W, Boeger D, Buentzel J, Hoffmann K, Kaftan H et al (2021) 30-day readmission rate in pediatric otorhinolaryngology inpatients: a retrospective population-based cohort study. J Otolaryngol Head Neck Surg 50:55. https://doi.org/10.1186/s40463-021-00536-8
Stafford JA, Redmann AJ, Singh E, Sarber K, Ishman SL (2021) The effect of postoperative steroid dosing on readmission rates following radiofrequency ablation tonsillectomy. Int J Pediatr Otorhinolaryngol 149:110862. https://doi.org/10.1016/j.ijporl.2021.110862
Khoury H, Azar SS, Boutros H, Shapiro NL (2021) Preoperative predictors and costs of 30-day readmission following inpatient pediatric tonsillectomy in the United States. Otolaryngol Neck Surg 165:470–476. https://doi.org/10.1177/0194599820980709
Leader BA, Wiebracht ND, Meinzen-Derr J, Ishman SL (2020) The impact of resident involvement on tonsillectomy outcomes and surgical time. Laryngoscope 130:2481–2486. https://doi.org/10.1002/lary.28427
Burckardt E, Rebholz W, Allen S, Cash E, Goldman J (2019) Predictors for hemorrhage following pediatric adenotonsillectomy. Int J Pediatr Otorhinolaryngol 117:143–147. https://doi.org/10.1016/j.ijporl.2018.11.029
Mahant S, Keren R, Localio R, Luan X, Song L, Shah SS et al (2014) Variation in quality of tonsillectomy perioperative care and revisit rates in children’s hospitals. Pediatrics 133:280–288. https://doi.org/10.1542/peds.2013-1884
Axon RN, Williams MV (2011) Hospital readmission as an accountability measure. JAMA 305:504. https://doi.org/10.1001/jama.2011.72
Payne NR, Flood A (2015) Preventing pediatric readmissions: which ones and how? J Pediatr 166:519–520. https://doi.org/10.1016/j.jpeds.2014.12.020
Gay JC, Agrawal R, Auger KA, Del Beccaro MA, Eghtesady P, Fieldston ES et al (2015) Rates and impact of potentially preventable readmissions at children’s hospitals. J Pediatr 166:613-619.e5. https://doi.org/10.1016/j.jpeds.2014.10.052
Faul F, Erdfelder E, Lang A-G, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191. https://doi.org/10.3758/bf03193146
Faul F, Erdfelder E, Buchner A, Lang A-G (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160. https://doi.org/10.3758/BRM.41.4.1149
Tran AHL, Chin KL, Horne RSC, Liew D, Rimmer J, Nixon GM (2022) Hospital revisits after paediatric tonsillectomy: a cohort study. J Otolaryngol Head Neck Surg 51:1. https://doi.org/10.1186/s40463-021-00552-8
Odhagen E, Stalfors J, Sunnergren O (2019) Morbidity after pediatric tonsillotomy versus tonsillectomy: a population-based cohort study. Laryngoscope 129:2619–2626. https://doi.org/10.1002/lary.27665
Shay S, Shapiro NL, Bhattacharyya N (2015) Revisit rates and diagnoses following pediatric tonsillectomy in a large multistate population: Revisits after Pediatric Tonsillectomy. Laryngoscope 125:457–461. https://doi.org/10.1002/lary.24783
Hsueh W-Y, Hsu W-C, Ko J-Y, Yeh T-H, Lee C-H, Kang K-T (2018) Population-based survey of inpatient pediatric tonsillectomy and postoperative hemorrhage in Taiwan, 1997–2012. Int J Pediatr Otorhinolaryngol 108:55–62. https://doi.org/10.1016/j.ijporl.2018.02.021
Lindquist NR, Feng Z, Patro A, Mukerji SS (2019) Age-related causes of emergency department visits after pediatric adenotonsillectomy at a tertiary pediatric referral center. Int J Pediatr Otorhinolaryngol 127:109668. https://doi.org/10.1016/j.ijporl.2019.109668
Manimaran V, Mohanty S, Jayagandhi SK, Umamaheshwaran P, Jeyabalakrishnan S (2019) A retrospective analysis of peroperative risk factors associated with posttonsillectomy reactionary hemorrhage in a teaching hospital. Int Arch Otorhinolaryngol 23:e403–e407. https://doi.org/10.1055/s-0039-1696702
Harju T, Numminen J (2017) Risk factors for secondary post-tonsillectomy haemorrhage following tonsillectomy with bipolar scissors: four-year retrospective cohort study. J Laryngol Otol 131:155–161. https://doi.org/10.1017/S0022215116009518
Aldrees T, Alzuwayed A, Majed A, Alzamil A, Almutairi M, Aloqaili Y (2020) Evaluation of secondary post-tonsillectomy bleeding among children in Saudi Arabia: risk factor analysis. Ear Nose Throat J. https://doi.org/10.1177/0145561320944662
Na’ara S, Aronov M, Gil Z, Gordin A (2021) Can tonsillectomy be safely performed by residents? A comparative retrospective study. Ann Otol Rhinol Laryngol 130:1340–1344. https://doi.org/10.1177/00034894211007057
Hinton-Bayre AD, Noonan K, Ling S, Vijayasekaran S (2017) Experience is more important than technology in paediatric post-tonsillectomy bleeding. J Laryngol Otol 131:S35-40. https://doi.org/10.1017/S0022215117000755
Tomkinson A, Harrison W, Owens D, Harris S, McClure V, Temple M (2011) Risk factors for postoperative hemorrhage following tonsillectomy: hemorrhage following tonsillectomy. Laryngoscope 121:279–288. https://doi.org/10.1002/lary.21242
Saravakos P, Hartwein J (2017) Surgical technique and post-tonsillectomy hemorrhage: a single institution’s retrospective study. Eur Arch Otorhinolaryngol 274:947–952. https://doi.org/10.1007/s00405-016-4271-3
Gysin C, Dulguerov P (2013) Hemorrhage after tonsillectomy: does the surgical technique really matter? ORL 75:123–132. https://doi.org/10.1159/000342314
Cadd B, Rogers M, Patel H, Crossland G (2015) (Ton)silly seasons? Do atmospheric conditions actually affect post-tonsillectomy secondary haemorrhage rates? J Laryngol Otol 129:702–705. https://doi.org/10.1017/S0022215115001292
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical approval
This article does not contain any experimental studies with human participants or animals performed by any of the authors. Local ethics committee approval was obtained for the research (KTO Karatay University: 15.01.2021-709).
Informed consent
Formal consent is not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karatas, H.A. Readmission after OSA surgery in pediatric patients. Eur Arch Otorhinolaryngol 280, 879–884 (2023). https://doi.org/10.1007/s00405-022-07657-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07657-4