Abstract
Introduction
Nowadays, 70% of patients in Europe and the USA are affected by a p16 + , potentially HPV driven oropharyngeal squamous cell carcinoma. However, despite the improved survival rate in this group, the quality-of-life remains low in cases which neck dissection took place. In this vein, in recent years, some surgeons have considered to avoid dissection of level IIB, proposing a supra-selective non-IIb neck dissection.
Materials and methods
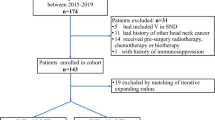
A retrospective, longitudinal, multicentric study was conducted, including patients with pathologically confirmed primary HPV + or HPV − OPSCC who went through surgical treatment for the primary lesion and neck dissection.
Results
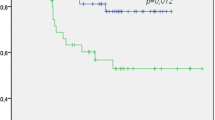
141 patients were included. Among them, 99 (70.2%) were male and 42 (29.8%) were female. The mean age was 62 ± 9 years (range 36–81). The most frequent anatomical location was the tonsil in 63 (44.7%) of patients. The most common approach was the classic transoral oropharyngectomy in 51 (36.2%) patients. Immunohistochemistry for p16 was positive in 62 (44%) patients. One-hundred and five (74.5%) patients received a unilateral ND, and a 36 (25.5%) a bilateral ND. Of those, a 12.8% (18/141) of patients were level IIb LN + . According to our results, level IIb ND should be considered in patients underwent therapeutic ND with positive LN metastasis in level IIa (OR = 9.83; 95% CI 3.463–27.917) or III (OR = 6.25; 95% CI 2.158–18.143), advanced (T3/T4) oropharyngeal primary tumors (OR = 3.38; 95% CI 1.366–8.405), and patients with ENE (OR = 6.56; 95% CI 2.182–19.770), regardless of p16 status.
Conclusions
According to our results, level IIb ND should be considered in patients who underwent therapeutic ND with positive LN metastasis in level IIa or III, advanced oropharyngeal primary tumors, and patients with ENE, independently of p16 status. Prospective data are necessary to definitively ensure the safety of omitting ipsilateral or contralateral level IIb ND in cN − patients with early stage disease.
Similar content being viewed by others
Change history
02 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00405-022-07767-z
References
Ferlito A, Rinaldo A, Robbins KT et al (2003) Changing concepts in the surgical management of the cervical node metastasis. Oral Oncol 39:429–435
Ferlito A, Rinaldo A, Devaney KO et al (2002) Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumour in the cervical lymph nodes. Oral Oncol 38:747–751
Lee SY, Lim YC, Song MH, Lee JS, Koo BS, Choi EC (2006) Level IIb lymph node metastasis in elective neck dissection of oropharyngeal squamous cell carcinoma. Oral Oncol 42:1017–1021
Moore EJ, Olsen SM, Laborde RR et al (2012) Long-term functional and oncologic results of transoral robotic surgery for oropharyngeal squamous cell carcinoma. Mayo Clin Proc 87:219–225
Van Abel KM, Moore EJ (2012) Focus issue: neck dissection for oropharyngeal squamous cell carcinoma. ISRN Surg 2012:547017
Byers RM (1985) Modified neck dissection: a study of 967 cases from 1970 to 1980. Am J Surg 150:414–421
Ferlito A, Shaha AR, Rinaldo A (2002) The incidence of lymph node micrometastases in patients pathologically staged N0 in cancer of oral cavity and oropharynx. Oral Oncol 38:3–5
Chaturvedi AK, Engles EA, Anderson WF, Gillison ML (2008) Incidence trends for human papillomavirus-related and –unrelated oral squamous cell carcinomas in the United States. J Clin Oncol 26:612–619
Sturgis EM, Cincirpini PM (2007) Trends in head and neck cancer incidence in relation to smoking prevalence: an emerging epidemic of human papillomavirus-associated cancers? Cancer 110:1429–1435
Bauwens L, Baltres A, Fiani DJ, Zrounba P, Buiret G, Fleury B, Benzerdjeb N, Grégoire V (2021) Prevalence and distribution of cervical lymph node metastases in HPV-positive and HPV-negative oropharyngeal squamous cell carcinoma. Radiother Oncol 157:122–129
Weiss MH, Harrison LB, Isaacs RS (1994) Use of decision analysis in planning a management strategy for the stage N0 neck. Arch Otolaryngol Head Neck Surg 120:699–702
Crile G III (1906) On the technique of operations upon the head and neck. Ann Surg 44:842–850
Bocca E, Pignataro O (1967) A conservation technique in radical neck dissection. Ann Otol Rhinol Laryngol 76:975–987
Chiesa-Estomba CM, Soriano-Reixach M, Thomas-Arrizabalaga I, Sistiaga-Suarez JA, González-García JA, Larruscain E, Altuna X (2021) Complications after functional neck dissection in head and neck cancer patients: an observational, retrospective, single-centre study. ORL J Otorhinolaryngol Relat Spec 83:372–380
Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB, Pruet CW (1991) Standardizing neck dissection terminology: official report of the Academy’s Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg 117:601–605
Shah JP (1990) Patterns of cervical lymph node metastasis from squamous carcinomas of the upper aerodigestive tract. Am J Surg 160:405–409
Lindberg R (1972) Distribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 29:1446–1449
Nahum AM, Mullally W, Marmor L (1961) A syndrome resulting from radical neck dissection. Arch Otolaryngol 74:424–428
Leipzig B, Suen JY, English JL, Barnes J, Hooper M (1983) Functional evaluation of the spinal accessory nerve after neck dissection. Am J Surg 146:526–530
Sobol S, Jensen C, Sawyer W Jr, Costiloe P, Thong N (1985) Objective comparison of physical dysfunction after neck dissection. Am J Surg 150:503–509
Terrell JE, Welsh DE, Bradford CR et al (2000) Pain, quality of life, and spinal accessory nerve status after neck dissection. Laryngoscope 110:620–626
Bradley PJ, Ferlito A, Silver CE et al (2011) Neck treatment and shoulder morbidity: still a challenge. Head Neck 33:1060–1067
Schiefke F, Akdemir M, Weber A, Akdemir D, Singer S, Frerich B (2009) Function, postoperative morbidity, and quality of life after cervical sentinel node biopsy and after selective neck dissection. Head Neck 31:503–512
Celik B, Coskun H, Kumas FF et al (2009) Accessory nerve function after level 2b-preserving selective neck dissection. Head Neck 31:1496–1501
Koybasioglu A, Bora Tokcaer A, Inal E, Uslu S, Kocak T, Ural A (2006) Accessory nerve function in lateral selective neck dissection with undissected level IIb. ORL J Otorhinolaryngol Relat Spec 68:88–92
Parikh S, Tedman BM, Scott B, Lowe D, Rogers SN (2012) A double blind randomized trial of IIb or not IIb neck dissections on electromyography, clinical examination, and questionnaire-based outcomes: a feasibility study. Br J Oral Maxillofac Surg 50:394–403
Mehanna H, Beech T, Nicholson T, El-Hariry I, McConkey C, Paleri V et al (2013) Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer—systematic review and meta-analysis of trends by time and region. Head Neck 35:747–755
Gross BC, Olsen SM, Lewis JE, Kasperbauer JL, Moore EJ, Olsen KD et al (2013) Level IIB lymph node metastasis in oropharyngeal squamous cell carcinoma. Laryngoscope 123:2700–2705
Sharma A, Méndez E, Yueh B, Lohavanichbutr P, Houck J, Doody DR et al (2012) Human papillomavirus-positive oral cavity and oropharyngeal cancer patients do not have better quality-of life trajectories. Otolaryngol Head Neck Surg 146:739–745
Mehanna H, Evans M, Beasley M, Chatterjee S, Dilkes M, Homer J et al (2016) Oropharyngeal cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 130(S2):S90–S96
Cannon RB, Houlton JJ, Patel S, Raju S, Noble A, Futran ND et al (2018) Patterns of cervical node positivity, regional failure rates, and fistula rates for HPV+ oropharyngeal squamous cell carcinoma treated with transoral robotic surgery (TORS). Oral Oncol 86:296–300
Meccariello G, Maniaci A, Bianchi G, Cammaroto G, Iannella G, Catalano A, Sgarzani R, De Vito A, Capaccio P, Pelucchi S, Vicini C (2021) Neck dissection and trans oral robotic surgery for oropharyngeal squamous cell carcinoma. Auris Nasus Larynx 49:117–125
Zenga J, Jackson RS, Graboyes EM, Sinha P, Lindberg M, Martin EJ et al (2017) Oncologic outcomes of selective neck dissection in HPV-related oropharyngeal squamous cell carcinoma. Laryngoscope 127:623–630
Plonowska KA, Strohl MP, Wang SJ, Ha PK, George JR, Heaton CM et al (2019) Human papillomavirus-associated oropharyngeal cancer: patterns of nodal disease. Otolaryngol Head Neck Surg 160:502–509
Amsbaugh MJ, Yusuf M, Cash E, Silverman C, Wilson E, Bumpous J et al (2016) Distribution of cervical lymph node metastases from squamous cell carcinoma of the oropharynx in the era of risk stratification using human papillomavirus and smoking status. Int J Radiat Oncol Biol Phys 96:349–353
Lindberg R (1972) Distribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer 29(6):1446–1449
Lim YC, Koo BS, Lee JS, Lim JY, Choi EC (2006) Distributions of cervical lymph node metastases in oropharyngeal carcinoma: therapeutic implications for the N0 neck. Laryngoscope 116:1148–1152
Wiegand S, Esters J, Muller HH et al (2009) Relevance of oropharyngeal cáncer lymph node metastases in the submandibular triangle and the posterior triangle apex. Anticancer Res 29:4785–4790
Corlette TH, Cole IE, Albsoul N, Ayyash M (2005) Neck dissection of level IIb: is it really necessary? Laryngoscope 115:1624–1626
Villaret AB, Piazza C, Peretti G et al (2007) Multicentric prospective study on the prevalence of sublevel IIb metastases in head and neck cancer. Arch Otolaryngol Head Neck Surg 133:897–903
Paleri V, Kumar Subramaniam S, Oozeer N, Rees G, Krishnan S (2008) Dissection of the submuscular recess (sublevel IIb) in squamous cell cancer of the upper aerodigestive tract: prospective study and systematic review of the literature. Head Neck 30:194–200
Smith R, Taylor SM, Trites JR, Smith A (2007) Patterns of lymph node metastases to the submuscular recess. J Otolaryngol 36:203–207
Lea J, Bachar G, Sawka AM et al (2010) Metastases to level IIb in squamous cell carcinoma of the oral cavity: a systematic review and meta-analysis. Head Neck 32:184–190
Last AS, Pipkorn P, Chen S, Kallogjeri D, Zenga J, Rich JT, Paniello R, Zevallos J, Chernock R, Adkins D, Oppelt P, Gay H, Daly M, Thorstad W, Jackson RS (2020) Risk and rate of occult contralateral nodal disease in surgically treated patients with human papillomavirus-related squamous cell carcinoma of the base of the tongue. JAMA Otolaryngol Head Neck Surg 146:50–56
Jones TA, Stell PM (1985) The preservation of shoulder function after radical neck dissection. Clin Otolaryngol Allied Sci 10:89–92
Weisberger EC (1987) The efferent supply of the trapezius muscle: a neuroanatomic basis for the preservation of shoulder function during neck dissection. Laryngoscope 97:435–445
Cappiello J, Piazza C, Giudice M, De Maria G, Nicolai P (2005) Shoulder disability after different selective neck dissections (levels II-IV versus levels II-V): a comparative study. Laryngoscope 115:259–263
Funding
No funding was used for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare don't have any conflict of interest.
Ethical approval
IRB approval—Code: HUD2105.
Informed consent
Informed consent was not required due to the retrospective nature of data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to the first and last names were swapped for the following authors “Giovanni Cammaroto, Giuditta Mannelli, Gabriele Molteni, Virginia Dallari, Jerome R Lechien, Manuel Tucciarone, Tareck Ayad, Giuseppe Meccariello” and corrected in this version
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chiesa-Estomba, C.M., Urazan, J.D., Cammaroto, G. et al. Lymph node metastasis in level IIb in oropharyngeal squamous cell carcinoma: a multicentric, longitudinal, retrospective analysis. Eur Arch Otorhinolaryngol 280, 869–876 (2023). https://doi.org/10.1007/s00405-022-07647-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07647-6