Abstract
Objectives of review
To review the literature for the evidence base for the aetiology and management of referred otalgia, looking particularly at non-malignant, neuralgic, structural and functional issues.
Type of review
Systematic review.
Search strategy
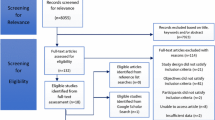
A systematic literature search was undertaken from the databases of EMBASE, CINAHL, MEDLINE®, BNI, and Cochrane Library according to predefined inclusion and exclusion criteria.
Evaluation method
All relevant titles, abstracts and full text articles were reviewed by three authors who resolved any differences by discussion and consultation with senior author.
Results
44 articles were included in our review. The overall quality of evidence was low, with the vast majority of the studies being case-series with three cohort and four randomised-controlled trials included. The prime causes and management strategies were focussed on temporomandibular joint dysfunction (TMJD), Eagle syndrome and neuralgia. Our meta-analyses found no difference on the management strategies for the interventions found.
Conclusions
Referred otalgia is common and treatment should be aimed at the underlying pathology. Potential aetiologies are vast given the extensive sensory innervation of the ear. An understanding of this and a structured approach to patient assessment is important for optimal patient management.



Similar content being viewed by others
References
Norris CD, Koontz NA (2020) Secondary otalgia: referred pain pathways and pathologies. AJNR Am J Neuroradiol 41(12):2188–2198. https://doi.org/10.3174/ajnr.A6808
Earwood JS, Rogers TS, Rathjen NA (2018) Ear pain: diagnosing common and uncommon causes. Am Fam Physician 97(1):20–27. https://auth.elsevier.com/ShibAuth/institutionLogin?entityID=https://idp.eng.nhs.uk/openathens&appReturnURL=https%3A%2F%2Fwww.clinicalkey.com%2Fcontent%2FplayBy%3Fissn%3D0002-838X%26vol%3D97%26issue%3D1%26pgfirst%3D20
Normand SL (1999) Meta-analysis: formulating, evaluating, combining, and reporting. Stat Med 18(3):321–359. https://doi.org/10.1002/(sici)1097-0258(19990215)18:3%3c321::aid-sim28%3e3.0.co;2-p
Brazzelli M, Cruickshank M, Tassie, McNamee P, Robertson CE (2015) Appendix 4 risk-of-bias checklist: non-randomised comparative studies. Collagenase clostridium histolyticum for the treatment of Dupuytren’s Contracture: systematic review and economic evaluation. Health Technol Assess (Rockv)
OCEBM Levels of Evidence Working Group (2011) The Oxford 2011 Levels of Evidence. Oxford Cent Evidence-Based Med. http://www.cebm.net/index.aspx?o=5653
Lam DK, Lawrence HP, Tenenbaum HC (2001) Aural symptoms in temporomandibular disorder patients attending a craniofacial pain unit. J Orofac Pain 15(2):146–157
Kuttila S, Kuttila M, Le Bell Y, Alanen P, Suonpää J (2004) Characteristics of subjects with secondary otalgia. J Orofac Pain 18(3):226–234
Sumitha R, Joseph NA (2015) Referred otalgia—a case series. Asian J Pharm Clin Res 8(2):343–345
Ferendiuk E, Zajdel K, Pihut M (2014) Incidence of otolaryngological symptoms in patients with temporomandibular joint dysfunctions. Biomed Res Int 2014:824684. https://doi.org/10.1155/2014/824684
Macedo J, Doi M, Oltramari-Navarro PV et al (2014) Association between ear fullness, earache, and temporomandibular joint disorders in the elderly. Int Arch Otorhinolaryngol. 18(4):383–386. https://doi.org/10.1055/s-0034-1385844
Tuz HH, Onder EM, Kisnisci RS (2003) Prevalence of otologic complaints in patients with temporomandibular disorder. Am J Orthod Dentofacial Orthop 123(6):620–623. https://doi.org/10.1016/s0889-5406(03)00153-7
Cooper BC, Kleinberg I (2007) Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio 25(2):114–126. https://doi.org/10.1179/crn.2007.018
Silveira AM, Feltrin PP, Zanetti RV, Mautoni MC (2007) Prevalence of patients harboring temporomandibular disorders in an otorhinolaryngology department. Braz J Otorhinolaryngol 73(4):528–532. https://doi.org/10.1016/s1808-8694(15)30105-1
Kuttila S, Kuttila M, Le Bell Y, Alanen P, Jouko S (1999) Aural symptoms and signs of temporomandibular disorder in association with treatment need and visits to a physician. Laryngoscope 109(10):1669–1673. https://doi.org/10.1097/00005537-199910000-00022
de Felício CM, de Melchior MO, Ferreira CLP, Da Silva MAMR (2008) Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. Cranio 26(2):118–125. https://doi.org/10.1179/crn.2008.016
Di Rienzo BL, Di Rienzo BA, D’Emilia M, Lauriello M, Coen TG (2004) Topical versus systemic diclofenac in the treatment of temporo-mandibular joint dysfunction symptoms. Acta Otorhinolaryngol Ital 24(5):279–283
Wright EF, Syms CA, Bifano SL (2000) Tinnitus, dizziness, and nonotologic otalgia improvement through temporomandibular disorder therapy. Mil Med 165(10):733–736
Hodges JM (1990) Managing temporomandibular joint syndrome. Laryngoscope 100(1):60–66. https://doi.org/10.1288/00005537-199001000-00013
Kuttila M, Le Bell Y, Savolainen-Niemi E, Kuttila S, Alanen P (2002) Efficiency of occlusal appliance therapy in secondary otalgia and temporomandibular disorders. Acta Odontol Scand 60(4):248–254. https://doi.org/10.1080/000163502760148034
Tozoglu S, Bayramoglu Z, Ozkan O (2015) Outcome of otologic symptoms after temporomandibular joint arthrocentesis. J Craniofac Surg 26(4):e344–e347. https://doi.org/10.1097/SCS.0000000000001808
Kef K (2021) Application of botulinum toxin in patients with secondary otalgia caused by bruxism. J Pain Res 14:1051–1059. https://doi.org/10.2147/JPR.S292550
Taziki MH, Behnampour N (2012) A study of the etiology of referred otalgia. Iran J Otorhinolaryngol 24(69):171–176. https://doi.org/10.22038/ijorl.2011.195
Anwar K, Khan S, Shahabi I, Niazi ZB (2019) The frequency of involvement of head & neck sites in referred otalgia—an experience at a tertiary care hospital. Pakistan J Med Sci 35(4):1138–1142. https://doi.org/10.12669/pjms.35.4.236
Jaber JJ, Leonetti JP, Lawrason AE, Feustel PJ (2008) Cervical spine causes for referred otalgia. Otolaryngol Head Neck Surg 138(4):479–485. https://doi.org/10.1016/j.otohns.2007.12.043
Murphy DR, Gay CW (2011) Manual therapy and ear pain: a report of four cases. J Can Chiropr Assoc 55(1):40–46
Lamer TJ (1991) Ear pain due to cervical spine arthritis: treatment with cervical facet injection. Headache 31(10):682–683. https://doi.org/10.1111/j.1526-4610.1991.hed3110682.x
Iikuni F, Nomura Y, Goto F, Murakami M, Shigihara S, Ikeda M (2013) Why do patients with fibromyalgia complain of ear-related symptoms? Ear-related symptoms and otological findings in patients with fibromyalgia. Clin Rheumatol 32(10):1437–1441. https://doi.org/10.1007/s10067-013-2287-2
Schilder AGM, Bhutta MF, Butler CC et al (2015) Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol 40(5):407–411. https://doi.org/10.1111/coa.12475
Fitzpatrick TH, Lovin BD, Magister MJ, Waltonen JD, Browne JD, Sullivan CA (2020) Surgical management of Eagle syndrome: a 17-year experience with open and transoral robotic styloidectomy. Am J Otolaryngol 41(2):102324. https://doi.org/10.1016/j.amjoto.2019.102324
Waters CM, Ho S, Luginbuhl A, Curry JM, Cognetti DM (2019) Surgical management of stylohyoid pain (Eagle’s) syndrome: a 5-year experience. Ann Otol Rhinol Laryngol 128(3):220–226. https://doi.org/10.1177/0003489418816999
Hardin FM, Xiao R, Burkey BB (2018) Surgical management of patients with Eagle syndrome. Am J Otolaryngol 39(5):481–484. https://doi.org/10.1016/j.amjoto.2018.05.003
Maru YK, Patidar K (2003) Stylalgia and its surgical management by intra oral route-clinical experience of 332 cases. Indian J Otolaryngol Head Neck Surg 55(2):87–90. https://doi.org/10.1007/BF02974610
Malik J-N, Monga S, Sharma A-P, Nabi N, Naseeruddin K (2018) Stylalgia revisited: clinical profile and management. Iran J Otorhinolaryngol 30(101):335–340. https://doi.org/10.22038/ijorl.2018.21760.1787
Sundaram S, Punj J (2020) Randomized controlled trial comparing landmark and ultrasound-guided glossopharyngeal nerve in eagle syndrome. Pain Med 21(6):1208–1215. https://doi.org/10.1093/pm/pnz370
Fitzpatrick TH, Lovin BD, Magister MJ, Waltonen JD, Browne JD, Sullivan CA (2020) Surgical management of Eagle syndrome: a 17-year experience with open and transoral robotic styloidectomy. Am J Otolaryngol Head Neck Med Surg 41(2). https://go.openathens.net/redirector/nhs?url=https%3A%2F%2Fwww.clinicalkey.com%2Fcontent%2FplayBy%2Fdoi%2F%3Fv%3D10.1016%2Fj.amjoto.2019.102324
Goulin Lippi Fernandes E, van Doormaal T, de Ru S, Miller K, Han KS (2018) Microvascular decompression of the VII/VIII cranial nerve complex for the treatment of intermediate nerve neuralgia: a retrospective case series. Oper Neurosurg (Hagerstown, Md.) 15(4):378–385. https://doi.org/10.1093/ons/opx271
Pulec JL (2002) Geniculate neuralgia: long-term results of surgical treatment. Ear Nose Throat J 81(1):30–33. http://gateway.proquest.com/openurl?ctx_ver=Z39.88-2004&res_id=xri:pqm&req_dat=xri:pqil:pq_clntid=48038&rft_val_fmt=ori/fmt:kev:mtx:journal&genre=article&issn=0145-5613&volume=81&issue=1&spage=30
Clifton WE, Grewal S, Lundy L, Cheshire WP, Tubbs RS, Wharen RE (2020) Clinical implications of nervus intermedius variants in patients with geniculate neuralgia: let anatomy be the guide. Clin Anat 33(7):1056–1061. https://doi.org/10.1002/ca.23536
Holste KG, Hardaway FA, Raslan AM, Burchiel KJ (2018) Pain-free and pain-controlled survival after sectioning the nervus intermedius in nervus intermedius neuralgia: a single-institution review. J Neurosurg 131(2):352–359. https://doi.org/10.3171/2018.3.JNS172495
Peris-Celda M, Oushy S, Perry A et al (2018) Nervus intermedius and the surgical management of geniculate neuralgia. J Neurosurg 131(2):343–351. https://doi.org/10.3171/2018.3.JNS172920
Lovely TJ, Jannetta PJ (1997) Surgical management of geniculate neuralgia. Am J Otol 18(4):512–517
Rupa V, Saunders RL, Weider DJ (1991) Geniculate neuralgia: the surgical management of primary otalgia. J Neurosurg 75(4):505–511. https://doi.org/10.3171/jns.1991.75.4.0505
Ulubil SA, Eshraghi AA, Telischi FF (2009) Sectioning the sensory auricular branch of the facial nerve to treat recalcitrant otalgia. Otol Neurotol 30(4):522–524. https://doi.org/10.1097/MAO.0b013e31819e9084
Roberts DS, Yamasaki A, Sedaghat AR, Lee DJ, Reardon E (2016) Tympanic plexus neurectomy for intractable otalgia. Laryngoscope Investig Otolaryngol 1(5):135–139. https://doi.org/10.1002/lio2.31
Reddy R, Jufas N, Bance M, Patel N (2019) Endoscopic tympanic neurectomy for otic neuralgia—a case series. Aust J Otolaryngol 2(August):21–21. https://doi.org/10.21037/ajo.2019.07.01
Robblee J (2021) A pain in the ear: two case reports of nervus intermedius neuralgia and narrative review. Headache 61(3):414–421. https://doi.org/10.1111/head.14066
Teixido M, Seymour P, Kung B, Lazar S, Sabra O (2011) Otalgia associated with migraine. Otol Neurotol 32(2):322–325. https://doi.org/10.1097/MAO.0b013e318200a0c4
Mohammadi M, Ghadimi R, Saedi B (2005) Empiric therapy in otolaryngologic manifestations of gastroesophageal reflux disease. Acta Med Iran 43(1):15–18
Hagr A, Bance M (2011) An otalgia pain syndrome, the anterolateral tip of the mastoid syndrome (ATOMS): diagnosis and response to treatment. J Otolaryngol Head Neck Surg 40(5):359–366. https://doi.org/10.2310/7070.2011.100282
Birnbaum J (2015) Facial weakness, otalgia, and hemifacial spasm: a novel neurological syndrome in a case-series of 3 patients with rheumatic disease. Medicine (Baltimore) 94(40):e1445. https://doi.org/10.1097/MD.0000000000001445
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ally, M., Moinie, A., Lomas, J. et al. Aetiology and management options for secondary referred otalgia: a systematic review and meta-analyses. Eur Arch Otorhinolaryngol 280, 47–59 (2023). https://doi.org/10.1007/s00405-022-07638-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07638-7