Abstract
Purpose
The purpose of our study was to investigate the impact of HPV status in oncologic outcomes in patients with T1–2 oropharyngeal SCC associated with bulky N3 nodes, and to determine progression prognosis factors aiming to define the best therapeutic strategies for these patients.
Methods
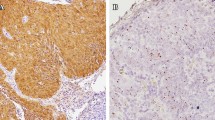
This multicenter retrospective study included patients with T1–2 oropharyngeal SCC with N3 nodes treated between 2010 and 2015 in 8 French comprehensive cancer centers. HPV status was determined with P16 hyperexpression in immunohistochemistry. HPV-positive patients were separated into 2 groups according to the associated smoking history (HPV + T +) or not (HPV + T−). We compared the oncological outcomes of patients according to HPV-status and smoking history.
Results
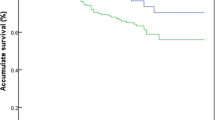
Of 67 patients with T1–2 N3 oropharyngeal SCC, 36 patients (53.7%) were HPV negative and 31 patients (46.3%) HPV positive. 2-year PFS was significantly better in HPV + T− group (p = 0.036). The risk of death or progression was significantly reduced in HPV + T− comparatively to HPV- (HR 0.25 95%CI [0.07; 0.89]). 2-year OS was significantly better in HPV + T− group than in the other two groups (p = 0.017).
Conclusion
In patients with T1–2 oropharyngeal SCC associated with bulky N3 nodes, HPV positive patients without smoking history had better OS and PFS than HPV positive patients with smoking history and HPV negative patients. Thus, HPV status is a significant prognostic factor for survival but this benefit is altered when smoking history is associated. N3 HPV positive patients with smoking history have to be classified as high-risk.


Similar content being viewed by others
References
D’cruz AK, Pantvaidya GH, Agarwal JP, Chaukar DA, Pathak KA, Deshpande MS et al (2006) Split therapy: planned neck dissection followed by definitive radiotherapy for a T1, T2 pharyngolaryngeal primary cancer with operable N2, N3 nodal metastases—a prospective study. J Surg Oncol 93(1):56–61
Cracchiolo JR, Baxi SS, Morris LG, Ganly I, Patel SG, Cohen MA et al (2016) Increase in primary surgical treatment of T1 and T2 oropharyngeal squamous cell carcinoma and rates of adverse pathologic features: National Cancer Data Base. Cancer 122(10):1523–1532
Carsuzaa F, Dufour X, Gorphe P, Righini C, Cosmidis A, Rogé M et al (2020) Locoregional control, progression-free survival and morbidity rates in N3 head and neck cancer patients with low primary tumour burden: a 301-patient study. Clin Otolaryngol 45:877–884
Jéhannin-Ligier K, Belot A, Guizard A-V, Bossard N, Launoy G, Uhry Z (2017) Incidence trends for potentially human papilloma virus-related and -unrelated head and neck cancers in France using population-based cancer registries data: 1980–2012. Int J Cancer 140(9):2032–2039
Gorphe P, ChekkouryIdrissi Y, Tao Y, Moya-Plana A, Casiraghi O, Janot F et al (2019) Smoking and papillomavirus DNA in patients with p16-positive N3 oropharyngeal squamous cell carcinoma. Head Neck 41(4):1039–1045
Lin BM, Wang H, D’Souza G, Zhang Z, Fakhry C, Joseph AW et al (2013) Long-term prognosis and risk factors among patients with HPV-associated oropharyngeal squamous cell carcinoma. Cancer 119(19):3462–3471
Arnson Y, Shoenfeld Y, Amital H (2010) Effects of tobacco smoke on immunity, inflammation and autoimmunity. J Autoimmun 34(3):J258-265
Virk JS, Ingle M, Podesta CM, Gujral DM, Awad Z (2020) Survival outcomes for head and neck cancer patients with N3 cervical nodal metastases. Clin Otolaryngol 45(3):342–349
O’Sullivan B, Huang SH, Siu LL, Waldron J, Zhao H, Perez-Ordonez B et al (2013) Deintensification candidate subgroups in human papillomavirus-related oropharyngeal cancer according to minimal risk of distant metastasis. J Clin Oncol 31(5):543–550
Zenga J, Haughey BH, Jackson RS, Adkins DR, Aranake-Chrisinger J, Bhatt N et al (2017) Outcomes of surgically treated human papillomavirus-related oropharyngeal squamous cell carcinoma with N3 disease. Laryngoscope 127(9):2033–2037
Huang SH, Xu W, Waldron J, Siu L, Shen X, Tong L et al (2015) Refining American Joint Committee on Cancer/Union for International Cancer Control TNM stage and prognostic groups for human papillomavirus-related oropharyngeal carcinomas. J Clin Oncol 33(8):836–845
Ward MJ, Mellows T, Harris S, Webb A, Patel NN, Cox HJ et al (2015) Staging and treatment of oropharyngeal cancer in the human papillomavirus era. Head Neck 37(7):1002–1013
Hong AM, Martin A, Armstrong BK, Lee CS, Jones D, Chatfield MD et al (2013) Human papillomavirus modifies the prognostic significance of T stage and possibly N stage in tonsillar cancer. Ann Oncol 24(1):215–219
Gillison ML, D’Souza G, Westra W, Sugar E, Xiao W, Begum S et al (2008) Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst 100(6):407–420
Tuyns AJ, Péquignot G, Jensen OM (1978) Nutrition, alcohol and oesophageal cancer (author’s transl). Bull Cancer 65(1):58–64
Blanchard D, Barry B, De Raucourt D, Choussy O, Dessard-Diana B, Hans S et al (2015) Guidelines update: post-treatment follow-up of adult head and neck squamous cell carcinoma: screening for metastasis and metachronous esophageal and bronchial locations. Eur Ann Otorhinolaryngol Head Neck Dis 132(4):217–221
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363(1):24–35
Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H et al (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100(4):261–269
Maxwell JH, Kumar B, Feng FY, Worden FP, Lee J, Eisbruch A et al (2010) Tobacco use in HPV-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res 16(4):1226
Gorphe P, Classe M, Ammari S, Garcia G, Even C, Casiraghi O et al (2022) Patterns of disease events and causes of death in patients with HPV-positive versus HPV-negative oropharyngeal carcinoma. Radiother Oncol 168:40–45
Bodelon C, Untereiner ME, Machiela MJ, Vinokurova S, Wentzensen N (2016) Genomic characterization of viral integration sites in HPV-related cancers. Int J Cancer 139(9):2001–2011
Jackson R, Rosa BA, Lameiras S, Cuninghame S, Bernard J, Floriano WB et al (2016) Functional variants of human papillomavirus type 16 demonstrate host genome integration and transcriptional alterations corresponding to their unique cancer epidemiology. BMC Genom 17(1):851
Hong A, Zhang X, Jones D, Veillard A-S, Zhang M, Martin A et al (2016) Relationships between p53 mutation, HPV status and outcome in oropharyngeal squamous cell carcinoma. Radiother Oncol 118(2):342–349
Ragin CCR, Taioli E (2007) Survival of squamous cell carcinoma of the head and neck in relation to human papillomavirus infection: review and meta-analysis. Int J Cancer 121(8):1813–1820
Seo YJ, Shin H, Lee HW, Jung HR (2021) Causes of necrotic features in fine-needle aspirates from cervical lymph nodes. J Pathol Transl Med 55(1):60–67
Santini L, Favier V, Benoudiba F, Garcia G, Abgral R, Zerdoud S et al (2020) Cystic form of cervical lymphadenopathy in adults. Guidelines of the French Society of Otorhinolaryngology (short version). Part 2-etiological diagnosis procedure: clinical and imaging assessment. Eur Ann Otorhinolaryngol Head Neck Dis 137(2):117–121
Sharma SD, Stimpson P (2016) Assessment and management of presumed branchial cleft cysts: our experience. B-ENT 12(4):291–296
Gourin CG, Johnson JT (2000) Incidence of unsuspected metastases in lateral cervical cysts. Laryngoscope 110(10 Pt 1):1637–1641
Paver EC, Currie AM, Gupta R, Dahlstrom JE (2020) Human papilloma virus related squamous cell carcinomas of the head and neck: diagnosis, clinical implications and detection of HPV. Pathology 52(2):179–191
Lewis JS, Beadle B, Bishop JA, Chernock RD, Colasacco C, Lacchetti C et al (2018) Human papillomavirus testing in head and neck carcinomas: guideline from the College of American Pathologists. Arch Pathol Lab Med 142(5):559–597
Marur S, Li S, Cmelak AJ, Gillison ML, Zhao WJ, Ferris RL et al (2017) E1308: phase II trial of induction chemotherapy followed by reduced-dose radiation and weekly cetuximab in patients with HPV-associated resectable squamous cell carcinoma of the oropharynx—ECOG-ACRIN Cancer Research Group. J Clin Oncol 35(5):490–497
Philouze P, Céruse P, Thariat J (2018) Surgery or radiotherapy for oropharyngeal HPV-positive tumours? Cancer Radiother 22(6–7):481–486
Tsai CJ, McBride SM, Riaz N, Kang JJ, Spielsinger DJ, Waldenberg T et al (2022) Evaluation of substantial reduction in elective radiotherapy dose and field in patients with human papillomavirus-associated oropharyngeal carcinoma treated with definitive chemoradiotherapy. JAMA Oncol 8:364
Mirghani H, Amen F, Moreau F, Guigay J, Ferchiou M, Melkane AE et al (2014) Human papilloma virus testing in oropharyngeal squamous cell carcinoma: what the clinician should know. Oral Oncol 50(1):1–9
Mirghani H, Casiraghi O, Guerlain J, Amen F, He M-X, Ma X-J et al (2016) Diagnosis of HPV driven oropharyngeal cancers: comparing p16 based algorithms with the RNAscope HPV-test. Oral Oncol 62:101–108
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hurel, C., Carsuzaa, F., Salleron, J. et al. Impact of HPV status in T1–2 oropharyngeal squamous cell carcinoma with bulky N3 nodes: a multicenter GETTEC study. Eur Arch Otorhinolaryngol 280, 847–853 (2023). https://doi.org/10.1007/s00405-022-07637-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07637-8