Abstract
Purpose
To determine the oncological outcomes of cervical esophageal cancer (CEC) treated primarily with surgery.
Methods
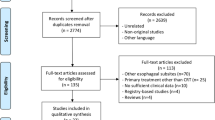
A systematic review and meta-analysis was performed according to the PRISMA guidelines.
Results
A total of 868 patients were included from 18 studies. Estimated pooled Overall Survival (OS) rates (95% Confidence Interval, CI) at 1 and 5 years were 74.4% (66.5–83.3), and 26.6% (20.3–34.7), respectively. Larynx non-preserving surgery (n = 229) showed an estimated pooled OS rates (95% CI) at 1 and 5 years of 59.3% (51.5–68.2) and 14.6% (8.8–24.3), respectively. On the other hand, larynx preserving surgery (n = 213) showed an estimated pooled OS rates (95% CI) at 1 and 5 years of 83.6% (78.2–89.4) and 35.1% (24.9–49.6), respectively.
Conclusions
Primary larynx-preserving surgery remains a valuable option for the management of CEC, with similar survival outcomes compared to primary chemoradiotherapy (CRT). On the other hand, larynx non-preserving surgery showed a significantly reduced survival, that may reflect the more advanced T classification of these tumors. Further studies are mandatory to directly compare primary surgery and primary CRT, distinguishing larynx preserving and non-preserving surgery.




Similar content being viewed by others
References
Zhang Y (2013) Epidemiology of esophageal cancer. World J Gastroenterol 19(34):5598–5606
Hoeben A, Polak J, Van De Voorde L, Hoebers F, Grabsch HI, de Vos-Geelen J (2016) Cervical esophageal cancer: a gap in cancer knowledge. Ann Oncol 27(9):1664–1674
Kato H, Nakajima M (2013) Treatments for esophageal cancer: a review. Gen Thorac Cardiovasc Surg 61(6):330–335
Buckstein M, Liu J (2019) Cervical esophageal cancers: challenges and opportunities. Curr Oncol Rep 21(5):46
Herrmann E, Mertineit N, De Bari B et al (2017) Outcome of proximal esophageal cancer after definitive combined chemo-radiation: a Swiss multicenter retrospective study. Radiat Oncol 12(1):97
McDowell LJ, Huang SH, Xu W et al (2017) Effect of intensity modulated radiation therapy with concurrent chemotherapy on survival for patients with cervical esophageal carcinoma. Int J Radiat Oncol Biol Phys 98(1):186–195
Sakanaka K, Ishida Y, Fujii K et al (2018) Long-term outcome of definitive radiotherapy for cervical esophageal squamous cell carcinoma. Radiat Oncol 13(1):7
Zenda S, Kojima T, Kato K et al (2016) Multicenter phase 2 study of cisplatin and 5-fluorouracil with concurrent radiation therapy as an organ preservation approach in patients with squamous cell carcinoma of the cervical esophagus. Int J Radiat Oncol Biol Phys 96(5):976–984
Cao CN, Luo JW, Gao L et al (2014) Primary radiotherapy compared with primary surgery in cervical esophageal cancer. JAMA Otolaryngol Head Neck Surg 140(10):918–926
Law S, Fok M, Chu KM, Wong J (1997) Thoracoscopic esophagectomy for esophageal cancer. Surgery 122(1):8–14
Cense HA, Law S, Wei W et al (2007) Pharyngolaryngoesophagectomy using the thoracoscopic approach. Surg Endosc 21(6):879–884
Law SY, Fok M, Wei WI et al (2000) Thoracoscopic esophageal mobilization for pharyngolaryngoesophagectomy. Ann Thorac Surg 70(2):418–422
Wong SKH, Chan ACW, Lee DWH, To EWH, Ng EKW, Chung SCS (2003) Minimal invasive approach of gastric and esophageal mobilization in total pharyngolaryngoesophagectomy: total laparoscopic and hand-assisted laparoscopic technique. Surg Endosc 17(5):798–802
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:579
National Institute for Health and Care Excellence (2012) Methods for the Development of NICE Public Health Guidance. National Institute for Health and Care Excellence (NICE), London
Sterne JAC, Sutton AJ, Ioannidis JPA et al (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002
McGrath S, Zhao X, Qin ZZ, Steele R, Benedetti A (2019) One-sample aggregate data meta-analysis of medians. Stat Med 38(6):969–984
Jackson D, White IR, Riley RD (2012) Quantifying the impact of between-study heterogeneity in multivariate meta-analyses. Stat Med 31(29):3805–3820
Baujat B, Mahé C, Pignon J-P, Hill C (2002) A graphical method for exploring heterogeneity in meta-analyses: application to a meta-analysis of 65 trials. Stat Med 21(18):2641–2652
Efron B (1988) Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc 83(402):414–425
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16
Combescure C, Foucher Y, Jackson D (2014) Meta-analysis of single-arm survival studies: a distribution-free approach for estimating summary survival curves with random effects. Stat Med 33(15):2521–2537
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Cao C-N, Liu S-Y, Luo J-W et al (2014) Pattern of failure in surgically treated patients with cervical esophageal squamous cell carcinoma. Otolaryngol Head Neck Surg 151(2):260–264
Chen L, Liu X, Wang R et al (2017) Minimally invasive esophagectomy for esophageal cancer according to the location of the tumor: experience of 251 patients. Ann Med Surg (Lond) 17:54–60
Chou S-H, Li H-P, Lee J-Y, Huang M-F, Lee C-H, Lee K-W (2010) Radical resection or chemoradiotherapy for cervical esophageal cancer? World J Surg 34(8):1832–1839
Chow VLY, Chan JYW, Law SYK (2019) Esophagogastric preservation in the surgical management of proximal esophageal cancer. Ann Thorac Surg 108(4):1029–1036
Daiko H, Hayashi R, Saikawa M et al (2007) Surgical management of carcinoma of the cervical esophagus. J Surg Oncol 96(2):166–172
Jiang M, He X, Wu D, Han Y, Zhang H, Wang M (2015) Reconstruction techniques for hypopharyngeal and cervical esophageal carcinoma. J Thorac Dis 7(3):449–454
Makino T, Yamasaki M, Miyazaki Y et al (2016) Short- and long-term outcomes of larynx-preserving surgery for cervical esophageal cancer: analysis of 100 consecutive cases. Ann Surg Oncol 23(Suppl 5):858–865
Nakajima Y, Kawada K, Tokairin Y et al (2017) “Larynx-preserving surgery” for cervical esophageal carcinoma can preserve the vocal function and improve the clinical outcome. Esophagus 14(1):76–83
Nikbakhsh N, Saidi F, Fahimi H (2012) A new technical approach to cancers of the cervical esophagus. Arch Iran Med 15(5):298–302
Ott K, Lordick F, Molls M, Bartels H, Biemer E, Siewert JR (2009) Limited resection and free jejunal graft interposition for squamous cell carcinoma of the cervical oesophagus. Br J Surg 96(3):258–266
Saeki H, Tsutsumi S, Yukaya T et al (2017) Clinicopathological Features of Cervical Esophageal Cancer: Retrospective Analysis of 63 Consecutive Patients Who Underwent Surgical Resection. Ann Surg 265(1):130–136
Saito R, Suzuki H, Motoyama S et al (2000) A clinical study of surgical treatment of patients with carcinoma of the cervical esophagus extending to the thoracic esophagus. Jpn J Thorac Cardiovasc Surg 48(7):417–423
Sun F, Li X, Lei D et al (2014) Surgical management of cervical esophageal carcinoma with larynx preservation and reconstruction. Int J Clin Exp Med 7(9):2771–2778
Takebayashi K, Tsubosa Y, Matsuda S et al (2017) Comparison of curative surgery and definitive chemoradiotherapy as initial treatment for patients with cervical esophageal cancer. Dis Esophagus 30(2):1–5
Tong DKH, Law S, Kwong DLW, Wei WI, Ng RWM, Wong KH (2011) Current management of cervical esophageal cancer. World J Surg 35(3):600–607
Ullah R, Bailie N, Kinsella J, Anikin V, Primrose WJ, Brooker DS (2002) Pharyngo-laryngo-oesophagectomy and gastric pull-up for post-cricoid and cervical oesophageal squamous cell carcinoma. J Laryngol Otol 116(10):826–830
Wang H-W, Chu P-Y, Kuo K-T et al (2006) A reappraisal of surgical management for squamous cell carcinoma in the pharyngoesophageal junction. J Surg Oncol 93(6):468–476
Watanabe A, Taniguchi M, Kimura Y, Kikkawa T, Hosokawa M (2020) Larynx-preserving hybrid surgery with endoscopic laryngopharyngeal surgery and open surgery for cervical esophageal cancer invading pharynx. Dis Esophagus 33(12):020
De Virgilio A, Costantino A, Festa BM et al (2022) Oncological outcomes of squamous cell carcinoma of the cervical esophagus treated with definitive (chemo-)radiotherapy: a systematic review and meta-analysis. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-022-03965-8
Yang H, Liu H, Chen Y et al (2018) Neoadjuvant chemoradiotherapy followed by surgery versus surgery alone for locally advanced squamous cell carcinoma of the esophagus (NEOCRTEC5010): a phase III multicenter, randomized, open-label clinical trial. J Clin Oncol 36(27):2796–2803
Costantino A, Festa BM, Ferreli F et al (2022) Circumferential pharyngeal reconstruction after total laryngopharyngectomy: a systematic review and network meta-analysis. Oral Oncol 127:105809
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De Virgilio, A., Costantino, A., Festa, B. et al. Oncological outcomes of cervical esophageal cancer treated primarily with surgery: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 280, 373–390 (2023). https://doi.org/10.1007/s00405-022-07589-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07589-z