Abstract
Purpose
To investigate the diagnostic value of combined multi-timepoint salivary pepsin testing (MTPSPT) and hypopharyngeal–esophageal multichannel intraluminal impedance–pH monitoring (HEMII–pH) for laryngopharyngeal reflux (LPR) and whether an appropriate reduction in the duration of HEMII–pH would affect the accuracy of diagnosis of LPR.
Methods
Recruited patients were studied with both MTPSPT and HEMII–pH. The diagnosis of LPR was based on the occurrence of > 1 reflux event and/or positive results on any of the MTPSPT. The diagnostic value of combined diagnosis was studied through combining a breakdown of the 24-h HEMII–pH finding and the results of the MTPSPT. The diagnostic value was expressed in terms of sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV).
Results
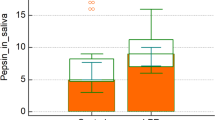
Based on 24-h HEMII–pH and MTPSPT, the positive rate of LPR was 83.33% and 74.69%, respectively. According to the combined diagnosis, the positive rate of LPR was 90.74%. The sensitivity and specificity of the combined diagnosis both were 89.51% and 100%, when the HEMII–pH intervals were 7 a.m.–6 p.m. and 7 a.m.–7 p.m., respectively. However, when the monitoring time was extended to 8 p.m. and bedtime, the sensitivity, specificity, PPV and NPV of the combined diagnosis both were 100%.
Conclusions
The combination of MTPSPT and HEMII–pH increased the sensitivity and accuracy of diagnosis of LPR. For patients with positive MTPSPT results, the duration of HEMII–pH can be appropriately shortened to reduce patient sufferings.
Similar content being viewed by others

References
Xiao S, Li J, Zheng H et al (2020) An epidemiological survey of laryngopharyngeal reflux disease at the otorhinolaryngology-head and neck surgery clinics in China. Eur Arch Otorhinolaryngol 277:2829–2838. https://doi.org/10.1007/s00405-020-06045-0
Wang J, Li J, Li X, Zhang S (2020) Is the pepsin immunohistochemical staining of laryngeal lesions an available way for diagnosing laryngopharyngeal reflux. Acta Otolaryngol 140:702–705. https://doi.org/10.1080/00016489.2020.1758774
Wang G, Qu C, Wang L et al (2019) Utility of 24-hour pharyngeal pH monitoring and clinical feature in laryngopharyngeal reflux disease. Acta Otolaryngol 139:299–303. https://doi.org/10.1080/00016489.2019.1571280
Li J, Wang J, Wu M, Zhao J, Guo H (2020) The role of nonacid reflux in laryngopharyngeal reflux diseases. Eur Arch Otorhinolaryngol 277:2813–2819. https://doi.org/10.1007/s00405-020-06015-6
Zhang M, Chia C, Stanley C, Phyland DJ, Paddle PM (2021) Diagnostic utility of salivary pepsin as compared with 24-hour dual pH/impedance probe in laryngopharyngeal reflux. Otolaryngol Head Neck Surg 164:375–380. https://doi.org/10.1177/0194599820951183
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16:274–277. https://doi.org/10.1016/s0892-1997(02)00097-8
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111:1313–1317. https://doi.org/10.1097/00005537-200108000-00001
Lee YJ, Kwon J, Shin S, Eun YG, Shin JH, Lee GJ (2020) Optimization of saliva collection and immunochromatographic detection of salivary pepsin for point-of-care testing of laryngopharyngeal reflux. Sensors (Basel). https://doi.org/10.3390/s20010325
Bor S, Capanoglu D, Vardar R, Woodcock AD, Fisher J, Dettmar PW (2019) Validation of peptest in patients with gastro-esophageal reflux disease and laryngopharyngeal reflux undergoing impedance testing. J Gastrointestin Liver Dis 28:383–387. https://doi.org/10.15403/jgld-335
Barona-Lleo L, Barona-De Guzman R, Krstulovic C (2019) The diagnostic usefullness of the salivary pepsin test in symptomatic laryngopharyngeal reflux. J Voice 33:923–928. https://doi.org/10.1016/j.jvoice.2018.07.008
Knight J, Lively MO, Johnston N, Dettmar PW, Koufman JA (2005) Sensitive pepsin immunoassay for detection of laryngopharyngeal reflux. Laryngoscope 115:1473–1478. https://doi.org/10.1097/01.mlg.0000172043.51871.d9
Saritas Yuksel E, Hong SK, Strugala V et al (2012) Rapid salivary pepsin test: blinded assessment of test performance in gastroesophageal reflux disease. Laryngoscope 122:1312–1316. https://doi.org/10.1002/lary.23252
Li JR, Tian SY, Zou SZ, Liu T, Yu L, Wang WJ (2017) Pepsin measurement in saliva of the healthy adults for detection of laryngopharygeal reflux. Chin J Gastroesophageal Reflux Dis (Electronic Edition) 4:7–10. https://doi.org/10.3877/cma.j.issn.1674-6899.2017.01.002
Na SY, Kwon OE, Lee YC, Eun YG (2016) Optimal timing of saliva collection to detect pepsin in patients with laryngopharyngeal reflux. Laryngoscope 126:2770–2773. https://doi.org/10.1002/lary.26018
Zhang J, Li J, Zhang Y et al (2021) Multitime point pepsin testing can double the rate of the diagnosis of laryngopharyngeal reflux. Laryngoscope Investig Otolaryngol 6:1389–1394. https://doi.org/10.1002/lio2.700
Wang J, Li J, Nie Q, Zhang R (2021) Are multiple tests necessary for salivary pepsin detection in the diagnosis of laryngopharyngeal reflux? Otolaryngol Head Neck Surg. https://doi.org/10.1177/01945998211026837
Lechien JR, Bobin F, Dapri G et al (2021) Hypopharyngeal-esophageal impedance-pH monitoring profiles of laryngopharyngeal reflux patients. Laryngoscope 131:268–276. https://doi.org/10.1002/lary.28736
Hoppo T, Sanz AF, Nason KS et al (2012) How much pharyngeal exposure is “normal”? Normative data for laryngopharyngeal reflux events using hypopharyngeal multichannel intraluminal impedance (HMII). J Gastrointest Surg 16:16–24. https://doi.org/10.1007/s11605-011-1741-1 (discussion 24–15)
Johnson LF, DeMeester TR (1986) Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol 8(Suppl 1):52–58. https://doi.org/10.1097/00004836-198606001-00008
Chen YL, Bao YY, Zhou SH, Yao HT, Chen Z (2021) Relationship between pepsin expression and dysplasia grade in patients with vocal cord leukoplakia. Otolaryngol Head Neck Surg 164:160–165. https://doi.org/10.1177/0194599820938654
Lechien JR, Saussez S, Nacci A et al (2019) Association between laryngopharyngeal reflux and benign vocal folds lesions: a systematic review. Laryngoscope 129:E329–E341. https://doi.org/10.1002/lary.27932
Wang L, Tan JJ, Wu T et al (2017) Association between laryngeal pepsin levels and the presence of vocal fold polyps. Otolaryngol Head Neck Surg 156:144–151. https://doi.org/10.1177/0194599816676471
Lechien JR, Saussez S, Harmegnies B, Finck C (2020) Laryngopharyngeal reflux as causative factor of vocal fold nodules. J Voice 34:150–151. https://doi.org/10.1016/j.jvoice.2018.06.006
Tan JJ, Wang L, Mo TT, Wang J, Wang MG, Li XP (2019) Pepsin promotes IL-8 signaling-induced epithelial-mesenchymal transition in laryngeal carcinoma. Cancer Cell Int 19:64. https://doi.org/10.1186/s12935-019-0772-7
Cumpston EC, Blumin JH, Bock JM (2016) Dual pH with multichannel intraluminal impedance testing in the evaluation of subjective laryngopharyngeal reflux symptoms. Otolaryngol Head Neck Surg 155:1014–1020. https://doi.org/10.1177/0194599816665819
Calvo-Henriquez C, Ruano-Ravina A, Vaamonde P, Martinez-Capoccioni G, Martin-Martin C (2017) Is pepsin a reliable marker of laryngopharyngeal reflux? A systematic review. Otolaryngol Head Neck Surg 157:385–391. https://doi.org/10.1177/0194599817709430
Klimara MJ, Johnston N, Samuels TL et al (2020) Correlation of salivary and nasal lavage pepsin with MII-pH testing. Laryngoscope 130:961–966. https://doi.org/10.1002/lary.28182
Hayat JO, Yazaki E, Moore AT et al (2014) Objective detection of esophagopharyngeal reflux in patients with hoarseness and endoscopic signs of laryngeal inflammation. J Clin Gastroenterol 48:318–327. https://doi.org/10.1097/mcg.0000000000000011
Borges LF, Chan WW, Carroll TL (2019) Dual pH probes without proximal esophageal and pharyngeal impedance may be deficient in diagnosing LPR. J Voice 33:697–703. https://doi.org/10.1016/j.jvoice.2018.03.008
Gupta R, Sataloff RT (2009) Laryngopharyngeal reflux: current concepts and questions. Curr Opin Otolaryngol Head Neck Surg 17:143–148. https://doi.org/10.1097/MOO.0b013e32832b2581
Weitzendorfer M, Antoniou SA, Schredl P et al (2020) Pepsin and oropharyngeal pH monitoring to diagnose patients with laryngopharyngeal reflux. Laryngoscope 130:1780–1786. https://doi.org/10.1002/lary.28320
Lechien JR, Bobin F, Muls V et al (2020) Validity and reliability of the reflux symptom score. Laryngoscope 130:E98–E107. https://doi.org/10.1002/lary.28017
Lechien JR, Rodriguez Ruiz A, Dequanter D et al (2020) Validity and reliability of the reflux sign assessment. Ann Otol Rhinol Laryngol 129:313–325. https://doi.org/10.1177/0003489419888947
Hou C, Chen M, Chen T et al (2020) Study on laryngopharyngeal and esophageal reflux characteristics using 24-h multichannel intraluminal impedance-pH monitoring in healthy volunteers. Eur Arch Otorhinolaryngol 277:2801–2811. https://doi.org/10.1007/s00405-020-05969-x
Feng G, Wang J, Zhang L, Liu Y (2014) A study to draw a normative database of laryngopharynx pH profile in Chinese. J Neurogastroenterol Motil 20:347–351. https://doi.org/10.5056/jnm13138
Bobin F, Journe F, Lechien JR (2020) Saliva pepsin level of laryngopharyngeal reflux patients is not correlated with reflux episodes. Laryngoscope 130:1278–1281. https://doi.org/10.1002/lary.28260
Johnston N, Wells CW, Samuels TL, Blumin JH (2009) Pepsin in nonacidic refluxate can damage hypopharyngeal epithelial cells. Ann Otol Rhinol Laryngol 118:677–685. https://doi.org/10.1177/000348940911800913
Johnston N, Yan JC, Hoekzema CR et al (2012) Pepsin promotes proliferation of laryngeal and pharyngeal epithelial cells. Laryngoscope 122:1317–1325. https://doi.org/10.1002/lary.23307
Johnston N, Bulmer D, Gill GA et al (2003) Cell biology of laryngeal epithelial defenses in health and disease: further studies. Ann Otol Rhinol Laryngol 112:481–491. https://doi.org/10.1177/000348940311200601
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, J., Wang, X., Wang, J. et al. Does hypopharyngeal–esophageal multichannel intraluminal impedance–pH monitoring for the diagnosis of laryngopharyngeal reflux have to be 24 h?. Eur Arch Otorhinolaryngol 279, 5323–5329 (2022). https://doi.org/10.1007/s00405-022-07554-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07554-w