Abstract
Purpose
Whereas chronic noise exposure (CNE) is a known risk factor for tinnitus, little is known about how a history of CNE impacts tinnitus characteristics and its comorbid symptoms.
Methods
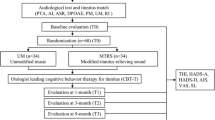
Seventy-five participants with chronic tinnitus (59m/16f, 22–78 years, 48 with sensory-neural hearing loss, and 27 with a normal audiogram) including 43 individuals with (Tin-CNE group) and 32 without (Tin group) a history of long-term occupational noise exposure were studied. Tinnitus characteristics were rated by a visual analog scale, and tinnitus comorbid symptoms were scored using self-assessment questionnaires.
Results
The Tin-CNE group showed reduced uncomfortable loudness level (ULL), sound tolerance, and quality of life (QoL), and increased tinnitus loudness, tinnitus handicap, anxiety, depression, insomnia severity, and tinnitus annoyance scores compared to the Tin group. Higher tinnitus loudness and a lower anxiety score were observed in participants with hearing loss relative to those without. Using a stepwise regression model also showed that tinnitus-related characteristics, hyperacusis, and tinnitus comorbid symptoms enhance one another.
Conclusions
The findings were in support of accumulative evidence indicating the adverse auditory and non-auditory effects of CNE, including exacerbated sound intolerance and tinnitus-related psychiatric symptoms. The results also showed that tinnitus alone can affect mental health regardless of hearing loss.




Similar content being viewed by others
Change history
09 May 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00405-022-07425-4
References
De Ridder D, Schlee W, Vanneste S, Londero A, Weisz N, Kleinjung T et al (2021) Tinnitus and tinnitus disorder: theoretical and operational definitions (an international multidisciplinary proposal). Prog Brain Res 260:1–25. https://doi.org/10.1016/bs.pbr.2020.12.002
Jafari Z, Copps T, Hole G, Kolb BE, Mohajerani MH (2021) Noise damage accelerates auditory aging and tinnitus: a Canadian population-based study. Otol Neurotol 41(10):1316–1326. https://doi.org/10.1097/mao.0000000000002848
Jafari Z, Kolb BE, Mohajerani MH (2019) Age-related hearing loss and tinnitus, dementia risk, and auditory amplification outcomes. Ageing Res Rev 56:100963. https://doi.org/10.1016/j.arr.2019.100963
Jastreboff PJ, Jastreboff MM (2003) Tinnitus retraining therapy for patients with tinnitus and decreased sound tolerance. Otolaryngol Clin N A 36(2):321–336. https://doi.org/10.1016/s0030-6665(02)00172-x
Sanchez TG, Medeiros IR, Levy CP, Ramalho JDR, Bento RF (2005) Tinnitus in normally hearing patients: clinical aspects and repercussions. Braz J Otorhinolaryngol 71(4):427–431. https://doi.org/10.1016/s1808-8694(15)31194-0
Savastano M (2008) Tinnitus with or without hearing loss: are its characteristics different? Eur Arch Otorhinolaryngol 265(11):1295–1300. https://doi.org/10.1007/s00405-008-0630-z
Martinez C, Wallenhorst C, McFerran D, Hall DA (2015) Incidence rates of clinically significant tinnitus: 10-year trend from a cohort study in England. Ear Hear 36(3):e69-75. https://doi.org/10.1097/aud.0000000000000121
Jafari Z, Baguley D, Kolb BE, Mohajerani MH (2022) A systematic review and meta-analysis of extended high-frequency hearing thresholds in tinnitus with a normal audiogram. Ear Hear (In Press)
Krog NH, Engdahl B, Tambs K (2010) The association between tinnitus and mental health in a general population sample: results from the HUNT Study. J Psychosom Res 69(3):289–298. https://doi.org/10.1016/j.jpsychores.2010.03.008
Jafari Z, Kolb BE, Mohajerani MH (2020) Noise exposure accelerates the risk of cognitive impairment and Alzheimer’s disease: adulthood, gestational, and prenatal mechanistic evidence from animal studies. Neurosci Biobehav Rev 117:110–128. https://doi.org/10.1016/j.neubiorev.2019.04.001
Eggermont JJ (2017) Epidemiology and genetics of hearing loss and tinnitus. Hearing Loss: Causes, Prevention, and Treatment. Academic Press, London, pp 209–234
Ohrstrom ESA, Svensson H, Gidlof-Gunnarsson A (2006) Effects of road traffic noise and the benefit of access to quietness. J Sound Vib 295:40–59
Eggermont JJ (2014) Non-auditory effects of noise. Noise and the brain. Academic Press,Elsevier, London, pp 266–299
WHMIS 2015–Glossary (2015) Canadian Center for Occupational Health and Safety. https://www.ccohs.ca/oshanswers/chemicals/whmis_ghs/glossary/glossary_a.htmlOSH. Accessed 1 Jan 2022.
Maxwell C (1978) Sensitivity and accuracy of the visual analogue scale: a psycho-physical classroom experiment. Br J Clin Pharmacol 6(1):15–24. https://doi.org/10.1111/j.1365-2125.1978.tb01676.x
Khalfa S, Dubal S, Veuillet E, Perez-Diaz F, Jouvent R, Collet L (2002) Psychometric normalization of a hyperacusis questionnaire. ORL J Otorhinolaryngol Relat Spec 64(6):436–442. https://doi.org/10.1159/000067570
Newman CW, Jacobson GP, Spitzer JB (1996) Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg 122(2):143–148. https://doi.org/10.1001/archotol.1996.01890140029007
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Bastien CH, Vallieres A, Morin CM (2001) Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2(4):297–307
Katz J, Chasin M, English K, Hood LJ, Tillery KL (2015) Handbook of clinical audiology, 7th edn. Wolters Kluwer Health, Philadelphia
Aazh H, Moore BCJ (2017) Factors related to uncomfortable loudness levels for patients seen in a tinnitus and hyperacusis clinic. Int J Audiol 56(10):793–800. https://doi.org/10.1080/14992027.2017.1335888
Deng XF, Shi GQ, Guo LL, Zhu CA, Chen YJ (2019) Analysis on risk factors of depressive symptoms in occupational noise-induced hearing loss patients: a cross-sectional study. Noise Health 21(98):17–24. https://doi.org/10.4103/nah.NAH_16_18
Kujawa SG, Liberman MC (2009) Adding insult to injury: cochlear nerve degeneration after “temporary” noise-induced hearing loss. J Neurosci 29(45):14077–14085. https://doi.org/10.1523/jneurosci.2845-09.2009
Eggermont JJ (2017) Effects of long-term non-traumatic noise exposure on the adult central auditory system. Hearing problems without hearing loss. Hear Res 352:12–22. https://doi.org/10.1016/j.heares.2016.10.015
Eggermont JJ, Roberts LE (2012) The neuroscience of tinnitus: understanding abnormal and normal auditory perception. Front Syst Neurosci 6:53. https://doi.org/10.3389/fnsys.2012.00053
Chen GD, Sheppard A, Salvi R (2016) Noise trauma induced plastic changes in brain regions outside the classical auditory pathway. Neuroscience 315:228–245. https://doi.org/10.1016/j.neuroscience.2015.12.005
Auerbach BD, Rodrigues PV, Salvi RJ (2014) Central gain control in tinnitus and hyperacusis. Front Neurol 5:206. https://doi.org/10.3389/fneur.2014.00206
Tyler RS, Pienkowski M, Roncancio ER, Jun HJ, Brozoski T, Dauman N et al (2014) A review of hyperacusis and future directions: part I. Definitions and manifestations. Am J Audiol 23(4):402–419. https://doi.org/10.1044/2014_aja-14-0010
Adams B, Sereda M, Casey A, Byrom P, Stockdale D, Hoare DJ (2021) A Delphi survey to determine a definition and description of hyperacusis by clinician consensus. Int J Audiol 60(8):607–613. https://doi.org/10.1080/14992027.2020.1855370
Knipper M, Van Dijk P, Nunes I, Rüttiger L, Zimmermann U (2013) Advances in the neurobiology of hearing disorders: recent developments regarding the basis of tinnitus and hyperacusis. Prog Neurobiol 111:17–33. https://doi.org/10.1016/j.pneurobio.2013.08.002
Liberman MC, Kujawa SG (2017) Cochlear synaptopathy in acquired sensorineural hearing loss: manifestations and mechanisms. Hear Res 349:138–147. https://doi.org/10.1016/j.heares.2017.01.003
Radziwon K, Auerbach BD, Ding D, Liu X, Chen GD, Salvi R (2019) Noise-induced loudness recruitment and hyperacusis: insufficient central gain in auditory cortex and amygdala. Neuroscience 422:212–227. https://doi.org/10.1016/j.neuroscience.2019.09.010
Chen F, Zhao F, Mahafza N, Lu W (2021) Detecting noise-induced Cochlear synaptopathy by auditory brainstem response in tinnitus patients with normal hearing thresholds: a meta-analysis. Front Neurosci 15:778197. https://doi.org/10.3389/fnins.2021.778197
Guest H, Munro KJ, Prendergast G, Howe S, Plack CJ (2017) Tinnitus with a normal audiogram: relation to noise exposure but no evidence for cochlear synaptopathy. Hear Res 344:265–274. https://doi.org/10.1016/j.heares.2016.12.002
Konig O, Schaette R, Kempter R, Gross M (2006) Course of hearing loss and occurrence of tinnitus. Hear Res 221(1–2):59–64. https://doi.org/10.1016/j.heares.2006.07.007
Hiller W, Goebel G (2006) Factors influencing tinnitus loudness and annoyance. Arch Otolaryngol Head Neck Surg 132(12):1323–1330. https://doi.org/10.1001/archotol.132.12.1323
Aazh H, Salvi R (2019) The relationship between severity of hearing loss and subjective tinnitus loudness among patients seen in a specialist tinnitus and hyperacusis therapy clinic in UK. J Am Acad Audiol 30(8):712–719. https://doi.org/10.3766/jaaa.17144
Chen YC, Zhang J, Li XW, Xia W, Feng X, Gao B et al (2014) Aberrant spontaneous brain activity in chronic tinnitus patients revealed by resting-state functional MRI. NeuroImage Clin 6:222–228. https://doi.org/10.1016/j.nicl.2014.09.011
Cai WW, Li ZC, Yang QT, Zhang T (2019) Abnormal spontaneous neural activity of the central auditory system changes the functional connectivity in the tinnitus brain: a resting-state functional MRI study. Front Neurosci 13:1314. https://doi.org/10.3389/fnins.2019.01314
Brüggemann P, Szczepek AJ, Rose M, McKenna L, Olze H, Mazurek B (2016) Impact of multiple factors on the degree of tinnitus distress. Front Hum Neurosci 10:341. https://doi.org/10.3389/fnhum.2016.00341
Wallhäusser-Franke E, Brade J, Balkenhol T, D’Amelio R, Seegmüller A, Delb W (2012) Tinnitus: distinguishing between subjectively perceived loudness and tinnitus-related distress. PLoS ONE 7(4):e34583. https://doi.org/10.1371/journal.pone.0034583
Balkenhol T, Wallhäusser-Franke E, Delb W (2013) Psychoacoustic tinnitus loudness and tinnitus-related distress show different associations with oscillatory brain activity. PLoS ONE 8(1):e53180. https://doi.org/10.1371/journal.pone.0053180
Hiller W, Goebel G (2007) When tinnitus loudness and annoyance are discrepant: audiological characteristics and psychological profile. Audiol Neuro-otol 12(6):391–400. https://doi.org/10.1159/000106482
Jastreboff PJ (2015) 25 years of tinnitus retraining therapy. HNO 63(4):307–311. https://doi.org/10.1007/s00106-014-2979-1
Asnis G, Majeed K, Henderson M, Sylvester C, Thomas M, De La Garza II R (2018) An examination of the relationship between insomnia and tinnitus: a review and recommendations. Clin Med Insights Psychiatry 9:1–8
Roth T (2009) Comorbid insomnia: current directions and future challenges. Am J Manag Care 15(Suppl):S6-13
Rosekind MR, Gregory KB (2010) Insomnia risks and costs: health, safety, and quality of life. Am Manag Care 16(8):617–626
Wallhäusser-Franke E, Schredl M (2013) Delb W (2013) Tinnitus and insomnia: is hyperarousal the common denominator? Sleep Med Rev 17(1):65–74. https://doi.org/10.1016/j.smrv.2012.04.003
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: ZJ; experimentation and data acquisition: GH, TC, ZJ; formal analysis: ZJ; writing the original draft: ZJ; review and editing: ZJ, GH, TC, BEK, MHM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to the label of figures 1, 2 was published incorrectly and corrected in this version.
Rights and permissions
About this article
Cite this article
Jafari, Z., Copps, T., Hole, G. et al. Tinnitus, sound intolerance, and mental health: the role of long-term occupational noise exposure. Eur Arch Otorhinolaryngol 279, 5161–5170 (2022). https://doi.org/10.1007/s00405-022-07362-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07362-2