Abstract
Purpose
To longitudinally evaluate the impact of the COVID-19-pandemic on the incidence of inpatient tonsil surgery and outpatient primary care of sore throat in Germany.
Methods
A retrospective interrupted time-series analysis was conducted. The national database of the Hospital Remuneration System was used to retrieve the number of operations performed between January 2019 and September 2021 including elective and non-elective cases with the exception of malign diseases. Three episodes were compared on a weekly basis: before, during, and after the first national lockdown (March 16–May 3, 2020). We also analysed the number of outpatient doctor contacts of sore throat patients in 2019 and 2020.
Results
Overall, 144,069 surgical cases were included in the analysis. The first lockdown resulted in an abrupt and significant decrease of all types of tonsil surgery (p < 0.01). The incidence of tonsillectomy decreased from 556 (before) to 111 (during) and 326 (after) cases per week (relative risk 0.24; 95% CI 0.19–0.30, and 0.82; 95% CI 0.73–0.92). After the lockdown, the incidence persisted on a lower level compared to 2019. The number of doctor contacts decreased from 2,967,322 in 2019 to 1,976,617 in 2020 (− 33.4%).
Conclusions
The first lockdown was associated with a significant decrease of all types of tonsil surgery. A return to pre-pandemic surgical activity was not identified. The findings were accompanied by a significant decrease of outpatient doctor contacts of sore throat patients in primary care, particularly in the subgroup of children and adolescents. The impact of the second lockdown, starting in December 2020, was by far not comparable.
Similar content being viewed by others
Introduction
Recent reports in the scientific literature indicate a constant decline in the number of tonsillectomies annually performed in Germany, either with (ATE) or without (TE) adenoidectomy. In contrast, the number of tonsillotomies (TOTO) performed per year had significantly increased while the total number of abscess-tonsillectomies (ABTE) and transoral incisional drainage (ID) to resolve peritonsillar abscess (PTA) had remained almost unchanged [1]. At the same time, there was an almost unchanged number of patients with a diagnosed PTA [2] and a nationwide decrease reported for the diagnosis “chronic tonsillitis” and “tonsil hypertrophy” [1].
During the first wave of the COVID-19 pandemic in March 2020, the Federal Ministry of Health in Germany has called on all hospitals to postpone elective surgical procedures and treatments [3]. A financial compensation for the resulting loss of revenue was regulated shortly afterwards in the Hospital Relief Act [4]. Only few weeks later (April 27, 2020), a step-by-step procedure for re-planning hospital bed capacities to end the restrictions on hospitals in Germany was officially recommended [5]. The result was a drastic drop in the number of surgical cases up to 70% [6, 7]. In addition, the German Federal Council (“Bundesrat”) had introduced a national lockdown and further decided that people have to wear medical face masks by April 27, 2020 [8].
Otolaryngologists were extremely affected by the political decisions since a considerable proportion of operations in the field of otorhinolaryngology is highly elective, particularly tonsil surgery. Moreover, the widespread utilization of face masks may have resulted in a decrease of sore throat and consumption of antibiotics, thus fewer candidates for tonsil surgery. Though volumes for emergent conditions have gradually returned to pre-pandemic levels, many of the volumes for chronic diseases general have not [9, 10].
This study was undertaken to longitudinally evaluate the dimension of the impact of the published government guidelines on the incidence of inpatient tonsil surgery on one hand and outpatient primary care of sore throat on the other hand in Germany. We hypothesized that in addition to political appeals on hospitals to postpone elective surgical procedures, the combination with social distancing, hygiene measures, stay-at-home orders, and fear of exposure to COVID-19 would have resulted not only in a decrease of surgical activity but also in the number of sore throat patients during the COVID-19 pandemic.
Materials and methods
Patient population
A retrospective observational study was performed with the use of anonymous, open-access population data obtainable from the Institute for the Hospital Remuneration System in Germany [11]. The national database was used to identify the weekly number of hospital admissions between January 2019 and September 2021 (latest update) for inpatient procedures including TE (code 5–281.0), ATE (code 5–282.0), TOTO (code 5–281.5), ABTE (code 5–281.1), and ID (code 5–280.0). The retrieved data provided further information on gender and age of the patients and on the main diagnoses that were documented as the reason for inpatient treatment such as chronic tonsillitis (CT; ICD J35.0), tonsillar hypertrophy (TH; J35.1), hypertrophy of adenoids (AD; J35.2), hypertrophy of tonsils and adenoids (TH + AD; J35.3), obstructive sleep apnea (OSA; G47.31) and PTA (J36). We compared the incidence of each individual procedure before, during and after the first lockdown associated with the appeal to postpone elective surgery and treatments. The restriction was implemented on March 16th (week 12) and rescinded on May 1st, 2020 (week 19). Accordingly, three time periods adjusted to full weeks were compared: pre-restriction (1/1/2019–3/15/2020), restriction (3/16/2020–5/3/2020) post-restriction (5/4/2020–9/26/2021).
In addition, we used claims data of outpatient care for insures of the German local health care funds (Allgemeine Ortskrankenkassen, AOK), the largest sickness fund group within Germany’s statutory health insurance system. It gives access to approximately 27 m people [12] of an 82 m people nation (33%) covering the data of sore throat patients in outpatient primary care. Unfortunately, data analysis was possible only on a quarterly basis for 2019 and 2020 (latest update). The various diagnoses encompassed (either alone or in combination) acute pharyngitis (ICD J02.-), acute tonsillitis (J03.-), and chronic tonsillitis (J35.0), respectively. PTA was not included since these patients usually refer to emergency ambulances and not to primary care physicians. Due to the patient-based data material, it was also possible to investigate whether or not antibiotics had been prescribed (ATC code J01) to treat sore throat. We compared the data of the year 2020 with the matching data of the pre-COVID year 2019.
Statistical analysis
Mean number of inpatient tonsil surgery per week was calculated by time period, type of surgery, primary diagnosis, gender and age group (decades). Cases with multiple surgery types were counted in each category. Weeks of turn of year showed extremely low case numbers and were assumed to be outliers and therefore excluded. Interrupted time-series (ITS) analysis was conducted using segmented Quasi-Poisson regression models to analyze trends of inpatient caseloads between periods and approximate an effect size with the pre-COVID-19 period as the baseline. ITS is a quasi-experimental design ideal for measuring the population-level impact of healthcare interventions where random assignment is not feasible [13,14,15]. ITS controls for secular trends which are known for the incidence of tonsil surgery. Results were expressed as relative risk of patient presentation compared to pre-COVID incidence. Seasonality was factored in for all types of surgery using Fourier terms given the link between the incidence of disease and seasonality[16]. Autocorrelation was assessed by examining the plot of residuals. As sensitivity analysis start and end of the restriction period was varied by one week because hospitals may have initiated or eased restrictions prematurely or delayed. All analyses were performed using STATA 16.0 (StataCorp LP, College Station, Texas).
The recommendations for good practice in secondary data analysis developed by the German Working Group on the Collection and Use of Secondary Data were applied in full. The study was exempt from ethic approval according to the Professional Code of Conduct of the Regional Medical Association as no identifiable patient data were used.
Results
Tonsil surgery
Overall, 144,069 inpatient cases were included in the analysis. During and after the restriction period, the weekly caseloads for all types of tonsil surgery were significantly lower compared to the pre-restriction period (p < 0.01) with emphasis during the lockdown (Table 1). TE cases per week had decreased from 556.1 (standard deviation [sd] 77.9) in the pre-restriction period to 110.7 (sd 46.4) in the restriction period and 326.0 (sd 69.2) in the post-restriction period, independently from age and gender. TEs due to chronic tonsillitis dropped from 426.4 (sd 67.7) to 55.3 (sd 38.1) rising again to 238.6 (sd 59.5) cases per week in the post period which accounts for a level shift from pre- to post-restriction of − 188 cases per week (supplemental table S1).
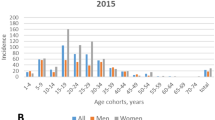
The restriction period resulted in a 76% decrease of TE cases (relative risk [RR] 0.236; 95% CI 0.187–0.298; Table 2, adjusted for overall weekly trend and seasonality). Although the number of operations increased thereafter, the incidence remained 18% below the pre-pandemic level (RR 0.824; 95% CI 0.734–0.924). The incidence of all types of tonsil surgery clearly correlated to the political announcements surrounding the first lockdown in March 2020 (Fig. 1). During the whole study period, the number of TE cases had decreased by 0.4% per week (RR 0.996; 95% CI 0.994–0.997), particularly in the young age group (10–17 years; RR 0.707, 95% CI 0.555–0.901). Supplemental figures S1 and S2 show the impact models by type of surgery, gender, age group and primary diagnosis.
The impact of the first lockdown on the incidence of ATE and TOTO were comparable despite of the fact that there was no weekly and no post period decrease for patients ≥ 50 years with ATE and for patients ≥ 17 years with TOTO (supplemental Fig. 1). In contrast, the weekly incidence of TOTO in elder (≥ 50 years) patients significantly increased by 0.3% (RR 1.003; 95% CI 1.000–1.005). Surprisingly, the incidence of emergency cases including ABTE and ID had decreased sharply with the beginning of the first lockdown and remained unchanged in the post-restriction period on a lower level compared to the pre-restriction period (RR 0.607; 95% CI 0.560–0.658 vs. RR 0.629; 95% CI 0.567–0.697, respectively). After adjusting for the restriction periods and the corresponding level shift, there was no change in weekly case numbers of ABTE und ID.
Primary care for sore throat
The analysis of the quarterly data on outpatient care revealed a significant decrease of doctor contacts in 2020 for sore throat not treated with antibiotics after the first quarter followed by almost no compensatory incline in this year (Fig. 2). The number of doctor contacts due to sore throat had decreased from 2,967,322 in 2019 to 1,976,617 in 2020 (− 33.4%). The comparison of the corresponding four quarters in 2019 and 2020 showed a decrease by 4.3%, 59.6%, 33.8%, 47.9% (male) and 2.8%, 57.9%, 30.4% and 46.5% (female), respectively. The reduction rate was even stronger when antibiotic prescriptions were considered: 7.5%, 67.2%, 48.3%, and 60.5% in male and 6.1%, 66.5%, 45.2%, 58.9% in female patients, respectively (Table 3). Doctor contacts with antibiotic prescription had decreased from 1,750,235 in 2019 to 1,015,409 in 2020 (− 42.0%).
Gender-specific reduction of doctor contacts in 2020 with or without antibiotic prescription compared to 2019. The diagram delineates a female preponderance and a significant reduction after the first lockdown (March 2020), particularly when antibiotic prescriptions were considered. Thereafter, the number of doctor contacts remained on a lower level. m male f female, w/o without, /w with, AB antibiotics
In every quarter, more doctors contacts were documented for female patients, whether antibiotics had been prescribed or not. The reduction rates were clearly related to young age, particularly, when antibiotic prescriptions were considered (Table 3).
Discussion
On December 31, 2019 a regional cluster of cases of pneumonia was reported in Wuhan in China probably deriving from a novel coronavirus, now acknowledged as SARS-CoV-2. The speed of the virus transmission resulted in a statement of the WHO on March 11, 2020 that Corona Virus disease (COVID-19) can be characterized as a pandemic [17]. The first case in Germany was published on January 27, 2020. Particularly in the community of otolaryngologists, there was a rapidly growing awareness of the high risk of virus transmission during diagnostic and therapeutic procedures [18]. This resulted in publication of recommendations and guidelines for clinical and endoscopic examination, surgical procedures and personal protection equipment of various societies in Germany[19]. Ongoing political discussions resulted in an appeal of the German Health Minister to postpone elective medical treatments (March 16th until May 1st 2020), accompanied by national lockdowns (March until May 2020; December 2020 until May 2021), introduction of social distancing, use of face masks and hand washing (June 2020). Schools, kindergartens and public indoor premises were closed, and daycare was recommended to be arranged at home. Gatherings were limited to two persons, and avoiding traveling was recommended. The various measurements resulted not only in a decreased number of COVID-cases but also in a reduction in the number of airway infections in general [20] and particularly in children [21].
This is strongly confirmed by the findings of our study revealing a significantly reduced number doctor contacts with antibiotic prescriptions, particularly in the second quarter (Table 3; Fig. 2). Interestingly, this phenomenon affected strongly young male and female patients (< 20 years of age) in the second and fourth quarter. We have no scientific explanation for this age-related phenomenon. It should be emphasized that children under the age of six still do not have to wear face masks in Germany and the protective value of face masks appears questionable in children and adolescents either due to inadequate fittings of the masks or discontinuous utilization in peer groups. Fewer doctor contacts resulted at least in part by the fact that patients or parents did not present their children or adolescents in fear of infection. The introduction of getting a sick leave by phone call on March 9, 2020 to avoid doctor contacts (ended on May 31, 2020 but was later resumed October 19, 2020) is a likely contributing factor. However, our study provides sound information concerning antibiotic prescriptions which requires a physician who needs to be contacted. Thus, we assume that there was a true reduction in the number of sore throat patients. Fewer doctor contacts without antibiotic prescriptions in the fourth quarter can hardly be explained as having resulted from a lockdown, since the second lockdown started by December 16, 2020 (Table 3). Our findings favorably compare with the results of a recent publication [22] analysing contacts of otolaryngologists and pediatricians over time. There was a stronger compensation in the subgroup of pediatricians after each lockdown had ended compared to otolaryngologists.
The decrease of tonsil surgery in Germany in the last decades continued during the pandemic overall but was emphasised sharply by the aforementioned political appeal. These restrictions resulted in a huge decrease in the incidence of tonsil surgery up to 82%. While specialists in German Hospitals had to re-organize operation lists and their professional environment, social distancing in the general population had become one of the main tasks, included fewer doctor contacts. This by itself resulted in fewer referrals from primary care physicians to the hospitals. However, social distancing in its entire dimensions obviously contributed to fewer infections resulting in sore throat.
Our study reveals that most cases in tonsil surgery were indicated to resolve chronic tonsillitis followed by upper airway obstruction due to tonsil hypertrophy. It is noteworthy that none of the different surgical interventions ever reached the quantitative level of pre-COVID time period. Instead our study shows—adjusting for seasonality—a significant level shift in surgical cases before and after the restriction period. Depending on type of surgery case numbers reduced from 18 to 39%.
One of the most surprising findings of our study was the fact that the total number of patients presenting with PTA requiring surgical interventions such as ABTE and ID had decreased, too, sharply with the introduction of the first lockdown and remained stable on a lower level compared to the pre-pandemic episode. Since the design of our study is unable to clarify causal factors for this phenomenon, it can only be speculated that this may have resulted mainly from social distancing [23].
Our study reveals that the number of surgical interventions to resolve upper airway obstruction due to TH had decreased. While the origin of TH is currently not fully understood, [24] we have no explanation how the lockdowns might have contributed to this finding. However, since there was no compensatory increase in this indication for surgery there must have been a spontaneous resolution taken place.
Haapanen et al. reported a decrease in the total number of tonsil surgery in 2020 by 37.3% based on rather small pediatric patient population (n = 568 vs. 106.526 of our study) in Finland [21]. The findings compare well to our study (− 34.0%) concerning elective surgery but our update for the first 5 months of the year 2021 revealed a stronger effect (− 54.5%). Emergency operations like in our study were not studied. Waiting times were not retrievable from the database of our study but had doubled in Finland for tonsil surgery.
Carrè et al. from France reported a number of only 350 emergency cases in 2020 compared to pre-COVID years in a tertiary pediatric emergency center (− 54%) including only one case with PTA [25]. The authors stated that there was a 54% drop in consultations, which is hardly comparable with the reduction of doctor contacts in primary care.
Heward et al. from the UK investigated the clinical courses of 44 pediatric patients during the lockdown period and identified a significant reduction in the number of episodes of acute tonsillitis and antibiotic treatment [26] which is confirmed by the findings of our study. The authors stated that 70% of parents wanted to proceed with their child’s TE during the coronavirus outbreak which demonstrates the impact tonsillitis has on the child and their family [26].
Gelardi et al. from Italy investigated the clinical courses in 162 children by telephone interviews two months after the first lockdown had started [27]. The parents reported a significant improvement of various symptoms resulting from tonsillitis or upper airway obstruction due to AD and/or TH. Grossly, the findings are confirmed by our study including a decrease of PTA since our patient population was not limited by age.
Smith from the UK reported changes in practice during the peak of the pandemic for the management of tonsillitis and PTA to avoid hospital admissions including iv-administration of cortisone and antibiotics [28]. Fewer patients (n = 1.181) had presented to 83 emergency departments with acute tonsillitis or PTA which complies with the findings of our study.
In the study of Li et al. from the UK, no difference was identified in antibiotic prescribing behavior comparing face-to-face and remote consultations [29]. The multicenter observational study was carried out in five general practice surgeries in North West Wales and encompassed 170 patients presenting with sore throat. Surprisingly, score systems like FeverPain or Centor-Score were rarely used (10% remote vs. 0% F2F). The findings support the idea that the findings of our study are unlikely to be biased by remote consultations.
Our study is not capable to estimate by which extent the decrease in the number of elective surgical cases was influenced by the financial compensation according to the Hospital Relief Act [4]. However, the assumption is challenged by the simultaneous decrease of ABTE and ID to resolve PTA and needs further research. The underlying trigger for the decreases is likely multifactorial.
Limitations
First, although the hospital data analysed are a complete survey on inpatient tonsil surgery in Germany, data of outpatient procedures are not provided in the survey. However, only a small proportion of patients scheduled for TOTO or AD is scheduled for an outpatient procedure in Germany which therefore appears not to confound our findings. Furthermore, given the enormous decrease in outpatient care, it is unlikely that inpatient procedures where substituted in ambulatory care. Second, there was no adjustment for comorbidities, socio-economic factors or place of residence because these items are missing on patient level in the hospital data. Third, coding problems may have occurred for the various diagnoses, which we estimated not as a significant confounding factor in the light of the population size. Although not recommended by the current guideline [29], we cannot exclude that some institutions may have performed a secondary TE after incision and drainage to resolve a PTA. However, we estimate the number to be insignificant. Fourth, the patient-based claims database of the AOK Research Institute used for investigating outpatient care captures data only on patients insured by the local health care funds. But the local health funds AOK provides statutory health insurance for roughly 33% of the German population and membership is open to anyone regardless of factors such as professional affiliation, income, age or comorbidities. So this database appears strong enough to draw firm estimations for the entire nation. Finally, we do not know how factors such as home-schooling or home office erased the necessity of doctor contacts. However, we assume that this did not impede the number of antibiotic prescribing.
Conclusions
This study found that lockdown measures were associated with considerable lower hospital incidence rates of elective and emergency tonsil surgery and fewer doctor contacts of sore throat patients in outpatient primary care. The considerable decrease in elective tonsil surgery cases was not associated with an increase of ABTE or ID for treatment of PTA. The decrease in doctor contacts was clearly related to young age and showed a female preponderance throughout 2020. This phenomenon was emphasized in the subgroup of patients with antibiotic prescriptions indicating fewer bacterial infections in sore throat patients. Children and patients presenting with PTA appear to benefit the most from tonsil surgery compared to TE. Social distancing during the lockdown appears to include positive side effects on the population suffering from sore throat and its complications in terms of PTA. The long-term effects of patient volume reductions on patient outcomes remain to be seen.
References
Windfuhr JP (2016) Specified data for tonsil surgery in Germany. GMS Curr Top Otorhinolaryngol Head Neck Surg. https://doi.org/10.3205/cto000135
Windfuhr JP, Chen YS (2019) Is the number of tonsillectomies and tonsillotomies a relevant issue? German version. HNO. https://doi.org/10.1007/s00106-019-00796-x
Osterloh F (2020) Coronavirus: Krankenhäuser verschieben planbare Eingriffe. Dtsch Arztebl International 117(12):575–577
Gesetz zum Ausgleich COVID-19 bedingter finanzieller Belastungen der Krankenhäuser und weiterer Gesundheitseinrichtungen (COVID-19-Krankenhausentlastungsge setz) vom 27. März 2020. Bundesgesetzblatt. 2020;Teil I Nr. 14
Winkelmann J (2020) Transition measures: maintaining essential services. https://eurohealthobservatory.who.int/monitors/hsrm/all-updates/hsrm/germany/transition-measures-maintaining-essential-services. Accessed 9 Nov 2021
Günster C, Drogan D, Hentschker C, Klauber J, Malzahn J, Schillinger G et al (2020) WIdO-report: Entwicklung der Krankenhausfallzahlen während des Coronavirus-Lockdowns. Nach ICD-Diagnosekapiteln und ausgewählten Behandlungsanlässen
Kuhlen R, Winklmair C, Schmithausen D, Schick J, Scriba P (2020) The effects of the COVID-19 pandemic and lockdown on routine hospital care for other illnesses. Dtsch Arztebl International 117(27–28):488–489. https://doi.org/10.3238/arztebl.2020.0489
Bundesrat (2020) Viertes Gesetz zum Schutz der Bevölkerung bei einer epidemischen Lage von nationaler Tragweite.Drucksache 315/21 (Beschluss) 22.04.2020. https://www.bundesrat.de/SharedDocs/beratungsvorgaenge/2021/0301-0400/0315-21.html. Accessed 11 Nov 2021
Karaca O, Rüggeberg J-A, Schuster M (2021) Zweite Pandemiewelle: Rückgang der Operationen variiert. Deutsches Ärzteblatt 118(16):A-824-B-689
Blecker S, Jones SA, Petrilli CM, Admon AJ, Weerahandi H, Francois F et al (2021) Hospitalizations for chronic disease and acute conditions in the time of COVID-19. JAMA Intern Med 181(2):269–271. https://doi.org/10.1001/jamainternmed.2020.3978
Institut für das Entgeltsystem im Krankenhaus. InEK DatenBrowser—Unterjährige Datenlieferung DRG. https://www.g-drg.de/Datenlieferung_gem._21_KHEntgG/InEK_DatenBrowser. Accessed 08 Jun 2021
Bundesministerium für Gesundheit (2021) Gesetzliche Krankenversicherung. Mitglieder, mitversicherte Angehörige und Krankenstand. Jahresdurchschnitt. https://www.bundesgesundheitsministerium.de/themen/krankenversicherung/zahlen-und-fakten-zur-krankenversicherung/mitglieder-und-versicherte.html. Accessed 11 Nov 2021
Bernal JL, Cummins S, Gasparrini A (2017) Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 46(1):348–355. https://doi.org/10.1093/ije/dyw098
Yu JS, Rodrigues AJ, Bovonratwet P, Shen T, Premkumar A, Sehgal R et al (2021) Changes in orthopaedic diagnoses during the COVID-19 pandemic. J Clin Orthop Trauma 22:101603. https://doi.org/10.1016/j.jcot.2021.101603
Penfold RB, Zhang F (2013) Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 13(6 Suppl):S38-44. https://doi.org/10.1016/j.acap.2013.08.002
Krüger K, Topfner N, Berner R, Windfuhr J, Oltrogge JH (2021) Clinical practice guideline: sore throat. Dtsch Arztebl Int. https://doi.org/10.3238/arztebl.m2021.0121 (forthcoming)
WHO (2020) Archived: WHO timeline—COVID-19. https://www.who.int/news/item/27-04-2020-who-timeline---covid-19. Accessed 11 Nov 2021
Kuhar HN, Heilingoetter A, Bergman M, Worobetz N, Chiang T, Matrka L (2020) Otolaryngology in the time of corona: assessing operative impact and risk during the COVID-19 crisis. Otolaryngol Head Neck Surg 163(2):307–315. https://doi.org/10.1177/0194599820930214
AWMF. COVID-19 Leitlinien / Handlungsempfehlungen. https://www.awmf.org/die-awmf/awmf-aktuell/aktuelle-leitlinien-und-informationen-zu-covid-19/covid-19-leitlinien.html. Accessed 1 Nov 2021
Barmer (2020) AHA-Regeln zeigen nachweislich Wirkung—Weniger Atemwegserkrankungen als im Jahr 2019. https://www.barmer.de/presse/presseinformationen/pressearchiv/2020-presse-archiv/aha-regeln-wirkung-283218. Accessed 11 Nov 2021
Haapanen M, Renko M, Artama M, Manninen IK, Mattila VM, Uimonen M et al (2021) Tympanostomies and tonsillar surgery in children during the COVID-19 pandemic in Finland. Laryngosc Investig Otolaryngol 6(4):878–884. https://doi.org/10.1002/lio2.622
Mangiapane S, Zhu L, Kretschmann J, Czihal T, von Stillfried D (2021) Veränderung der vertragsärztlichen Leistungsinanspruchnahme während der COVID‐Krise. https://www.zi.de/fileadmin/images/content/Publikationen/Trendreport_4_Leistungsinanspruchnahme_COVID_2021-04-19.pdf. Accessed 11 Nov 2021
Klug TE, Rusan M, Fuursted K, Ovesen T (2016) Peritonsillar abscess: complication of acute tonsillitis or weber’s glands infection? Otolaryngol Head Neck Surg 155(2):199–207. https://doi.org/10.1177/0194599816639551
Zagolski O (2010) Why do palatine tonsils grow back after partial tonsillectomy in children? Eur Arch Otorhinolaryngol 267(10):1613–1617. https://doi.org/10.1007/s00405-010-1261-8
Carre F, Leboulanger N, Thierry B, Simon F, Couloigner V, Denoyelle F et al (2021) Impact of COVID-19 lockdown on a tertiary center pediatric otolaryngology emergency department. Eur J Pediatr. https://doi.org/10.1007/s00431-021-04236-3
Heward E, Rocke J, Kumar N, Izzat S (2020) Recurrent tonsillitis and parental perceptions of tonsillectomy during the COVID-19 pandemic. Int J Pediatr Otorhinolaryngol 139:110463. https://doi.org/10.1016/j.ijporl.2020.110463
Gelardi M, Giancaspro R, Fiore V, Fortunato F, Cassano M (2020) COVID-19: Effects of lockdown on adenotonsillar hypertrophy and related diseases in children. Int J Pediatr Otorhinolaryngol 138:110284. https://doi.org/10.1016/j.ijporl.2020.110284
Smith ME (2020) Admission avoidance in tonsillitis and peritonsillar abscess: a prospective national audit during the initial peak of the COVID-19 pandemic. Clin Otolaryngol. https://doi.org/10.1111/coa.13680
Li C, Ong C, Morris A, Woollons I, Ashfaq A, Jagatia R (2021) Evaluating the appropriateness of antibiotic treatment of tonsillitis during COVID-19 in the North Wale primary healthcare setting. J Prim Care Community Health 12:21501327211003690. https://doi.org/10.1177/21501327211003687
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Ethical approval
According to the policy of the IRB responsible for the authors, this study was exempt from ethical approval because it was a secondary analysis of a publicly available dataset with anonymous data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Windfuhr, J.P., Günster, C. Impact of the COVID-pandemic on the incidence of tonsil surgery and sore throat in Germany. Eur Arch Otorhinolaryngol 279, 4157–4166 (2022). https://doi.org/10.1007/s00405-022-07308-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07308-8