Abstract
Objectives
Peritonsillar abscess is a common complication of acute tonsillitis. However, no consensus has been reached yet on the optimal treatment of this condition. Therefore, this study aimed to compare clinical outcomes of immediate and interval abscess tonsillectomy.
Methods
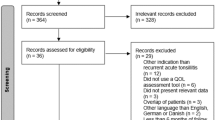
The databases of PubMed, Scopus, and Cochrane Central Register of Controlled Trials (CENTRAL) were searched for completed studies published until the 1st of November 2021. Comparative studies assessing intraoperative and postoperative outcomes of immediate and interval abscess tonsillectomy were considered, with the primary outcome being postoperative hemorrhage. Operative time, intraoperative blood loss, postoperative pain, and duration of hospital stay were classed as secondary outcomes. A random-effects pairwise meta-analysis of both randomized and non-randomized trials was conducted. Subgroup analysis linked to the randomization of trials was executed. Quality assessment was performed, utilizing the Cochrane risk of bias tool and ROBINS-I tool for randomized and non-randomized trials, respectively.
Results
Data from 265 cases stemming from six trials were pooled together. For postoperative bleeding rates, no statistically significant difference between immediate and interval tonsillectomy was detected (OR = 1.26; 95% CI 0.27, 5.86; p = 0.77). By contrast, longer hospital stay was observed for patients subjected to interval tonsillectomy (SMD = − 0.78; CI − 1.39 to− 0.17; p = 0.01). For operative time and intraoperative blood loss, no statistically significant difference was noticed between immediate and interval tonsillectomy (SMD = 1.10; 95% CI − 0.13, 2.33; p = 0.08; and SMD = 0.04; 95% CI − 0.49, 0.57; p = 0.88; respectively).
Conclusions
This study shows that quinsy tonsillectomy appears to be a safe method, providing full abscess drainage and instant relief of the symptoms. Moreover, quinsy tonsillectomy was not associated with a statistically higher postoperative hemorrhage incidence rate than immediate tonsillectomy.





Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Khan MA, Ahmed A, Khan M (2020) Comparison of early versus interval tonsillectomy in cases of peritonsillar abscess. Life Sci 1(1):5
Simon LM, Matijasec JWD, Perry AP, Kakade A, Walvekar RR, Kluka EA (2013) Pediatric peritonsillar abscess: quinsy ie versus interval tonsillectomy. Int J Pediatr Otorhinolaryngol 77(8):1355–1358
Klug TE, Rusan M, Fuursted K, Ovesen T (2016) Peritonsillar abscess: complication of acute tonsillitis or webers glands infection? Otolaryngol—Head Neck Surg (United States) 155(2):199–207
Lockhart R, Tami TA, Parker GS (1991) Role of quinsy tonsillectomy in the management of peritonsillar abscess. Ann Otol Rhinol Laryngol 100(7):569–571
Fagan JJ, Wormald PJ (1994) Quinsy tonsillectomy or interval tonsillectomy—a prospective randomised trial. S Afr Med J 84(10):689–690. PMID: 7839259
Chang B, Thamboo A, Burton M, Diamond C, Nunez D (2016) Needle aspiration versus incision and drainage for the treatment of peritonsillar abscess. Cochrane Libr. https://doi.org/10.1002/14651858.CD006287.pub4
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Higgins JPT, Altman DG (2008) Chapter 8: assessing risk of bias in included studies. In: Higgins JPT, Green S (eds) Cochrane Handbook for systematic reviews of interventions. John Wiley & Sons, Chichester (UK)
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:4–10
The Nordic Cochrane Centre, The Cochrane Collaboration (2011) Review Manager (RevMan). 5.1. The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark
Deeks JJ, Higgins JP, Altman DG (2008) Analysing data and undertaking meta-analyses. Cochrane Handb Syst Rev Interv Cochrane B Ser. https://doi.org/10.1002/9780470712184.ch9
Higgins JPT, Thompson SG (2002) No title. Stat Med 21:1539e1
Higgins JPTTS (2002) Quantifying heterogeneity in a meta-analysis. Stat Power Anal Behav Sci 21(11):1539
Reeves BC, Deeks JJ, Higgins JPTWG. (2008) Including non-randomized studies. Cochrane Handb Syst Rev Interv Chapter 13
Reeves BC, Deeks JJ, Higgins JPT WG. (2011) Including non-randomized studies. Cochrane Handb Syst Rev Interv Version 510 (updated March 2011) Cochrane Collab Chapter 13
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences, 2 edn. Routledge. https://doi.org/10.4324/9780203771587
Arshad A, Mazhar I, Ghulam DK, Muhammad I, Muhammad I, Najam ulHK (2021) A comparative analysis of per and post-operative complications in patients undergoing early and delayed interval tonsillectomies. Pak Postgrad Med J 31(04):190–194
Chowdhury CR, Bricknell MC (1992) The management of quinsy--a prospective study. J Laryngol Otol 106(11):986–988. https://doi.org/10.1017/s002221510012153x. PMID: 1479277
Javed M, Fazal-I-Wahid KN, Khan Q, Massemul H, Khan SI (2014) Interval tonsillectomies; comparison of per and post operative complications in patients undergoing early and delayed after peritosnisllar abscess. Prof Med J 21(5):1043–1047
Herzon F (1995) Peritonsillar abscess: incidence, current management practices and a proposal for treatment guidelines. Laryngoscope 105:1–17
Klug TE, Greve T, Hentze M (2020) Complications of peritonsillar abscess. Ann Clin Microbiol Antimicrob [Internet] 19(1):1–17. https://doi.org/10.1186/s12941-020-00375-x
Windfuhr J, Chen Y (2001) Immediate abscess tonsillectomy: a safe procedure? Auris Nasus Larynx 28(323):7
Giger R, Landis BN, Dulguerov P (2005) Hemorrhage risk after quinsy tonsillectomy. Otolaryngol—Head Neck Surg 133(5):729–734
Esposito S, Marchisio P, Capaccio P, Bellasio M, Semino M, Dusi E et al (2009) Risk factors for bacteremia during and after adenoidectomy and/or adenotonsillectomy. J Infect [Internet] 58(2):113–118. https://doi.org/10.1016/j.jinf.2008.12.003
Klug TE, Henriksen JJ, Rusan M, Fuursted K, Ovesen T (2012) Bacteremia during quinsy and elective tonsillectomy: an evaluation of antibiotic prophylaxis recommendations for patients undergoing tonsillectomy. J Cardiovasc Pharm Ther 17(3):298–302
Soldado L, Esteban F, Delgado-Rodríguez M, Solanellas J, Florez C, Martín E (1998) Bacteraemia during tonsillectomy: a study of the factors involved and clinical implications. Clin Otolaryngol Allied Sci 23(1):63–66
Suzuki M, Ueyama T, Mogi G (1998) Immediate tonsillectomy for peritonsillar abscess. Auris Nasus Larynx 26:299–304
Albertz N, Nazar G (2012) Peritonsillar abscess: treatment with immediate tonsillectomy—10 years of experience. Acta Otolaryngol 132(10):1102–1107
Baptista LAN (2018) Risk factors for peritonsillar abscess recurrence. Diss. Universidade de Coimbra
Windfuhr JP, Ulbrich T (2001) Post-tonsillectomy hemorrhage: results of a 3-month follow-up. Ear Nose Throat J 80(11):790:795–798. 800 passim. PMID: 11816891
Tugrul S, Degirmenci N, Eren SB, Dogan R, Veyseller B, Ozturan O (2015) Analgesic effect of magnesium in post-tonsillectomy patients: a prospective randomised clinical trial. Eur Arch Oto-Rhino-Laryngol 272(9):2483–2487
Leach J, Manning S, Schaefer S (1993) Comparison of two methods of tonsillectomy. Laryngoscope 103:619–622
Mitchell RB, Archer SM, Ishman SL, Rosenfeld RM, Coles S, Finestone SA et al (2019) Clinical Practice Guideline: Tonsillectomy in Children (Update)—Executive Summary. Otolaryngol—Head Neck Surg (United States) 160(2):187–205
Chung JH, Lee YC, Shin SY, Eun YG (2014) Risk factors for recurrence of peritonsillar abscess. J Laryngol Otol 57(2):1084–1088
Wang YP, Wang MC, Lin HC, Chou P (2014) The impact of prior tonsillitis and treatment modality on the recurrence of peritonsillar abscess: a nationwide cohort study. PLoS ONE 9(10):20–22
Wikstén J, Hytönen M, Pitkäranta A, Blomgren K (2012) Who ends up having tonsillectomy after peritonsillar infection? Eur Arch Oto-Rhino-Laryngol 269(4):1281–1284
Schraff S, McGinn JD, Derkay CS (2001) Peritonsillar abscess in children: a 10-year review of diagnosis and management. Int J Pediatr Otorhinolaryngol 57(3):213–218
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
AT was the primary author. AF assisted the primary author with data extraction, study selection, and literature research, whereas FD was involved in quality assessment. KG, ΙΤ, and PK reviewed the final version of the manuscript. ST and KT provided methodological advice and critically reviewed and revised the manuscript. Finally, CS and ST supervised the study and provided guidance on specific scientific issues. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tsikopoulos, A., Fountarlis, A., Tsikopoulos, K. et al. Immediate or interval abscess tonsillectomy? A systematic review and meta-analysis. Eur Arch Otorhinolaryngol 279, 2245–2257 (2022). https://doi.org/10.1007/s00405-022-07294-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07294-x