Abstract
Objectives
Endoscopic balloon dilatation (EBD) offers a safe and non-invasive surgical option for the treatment of subglottic stenosis. Patient selection is important to achieve good results and to detect which patients are more prone to the development of complications. The aim of this study was to determine predictors of postoperative problems and early complications in primary EBD surgeries.
Methods
A retrospective analysis was made of patients with acquired subglottic stenosis who were operated on with the EBD technique between January 2010 and December 2019 in the Otolaryngology—Head and Neck Surgery Department of Baskent University Hospital. Demographic data including the age and sex of the patients were collected together with etiology, presence of chromosomal or craniofacial anomaly (C/CA), duration of prolonged intubation (DPI), and extubation dilatation timeframe (EDT). Intra and postoperative follow-up data were recorded of the need for intubation or tracheotomy, development of desaturation, and grade and type of stenosis.
Results
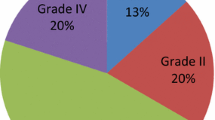
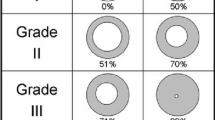
The male to female ratio was 2:1. The patients comprised 42 males and 22 females with a mean age of 296.52 ± 551.93 days. The cause of prolonged intubation was surgery for congenital heart disease in 50 (78.1%) patients and prematurity in 14 (21.9%). The type of lesion was acute granulation in 44 (72.1%) and chronic granulation in 17 (27.9%) patients. C/CA was determined in 13 patients, the mean grade of stenosis was 76.33 ± 15.21%, mean DPI was 25.25 ± 35.49 days, and mean EDT was calculated as 78.23 ± 373.82 days. Desaturation following endoscopic balloon dilatation developed in 26 (40.6%), orotracheal intubation was required in 10 (15.6%), tracheotomy in 10 (15.6%), and cardiopulmonary arrest occurred in 4 (6.25%). Prematurity, a longer duration of preoperative intubation, longer time from extubation to dilatation, older age, and higher grade of stenosis were determined as factors associated with postoperative early respiratory complications.
Conclusion
EBD indication should be carefully considered in children with acquired subglottic stenosis. To achieve better results and minimise complications, EBD should be performed without delay.

Similar content being viewed by others
References
Maunsell R, Avelino MA (2014) Balloon laryngoplasty for acquired subglottic stenosis in children: predictive factors for success. Braz J Otorhinolaryngol 80(5):409–415. https://doi.org/10.1016/j.bjorl.2014.07.012
Avelino M, Maunsell R, Jubé Wastowski I (2015) Predicting outcomes of balloon laryngoplasty in children with subglottic stenosis. Int J Pediatr Otorhinolaryngol 79:532–536
Mossad E, Youssef G (2009) Subglottic stenosis in children undergoing repair of congenital heart defects. J Cardiothorac Vasc Anesth 23:658–662. https://doi.org/10.1053/j.jvca.2008.12.018
Whigham AS, Howell R, Choi S, Peña M, Zalzal G, Preciado D (2012) Outcomes of balloon dilation in pediatric subglottic stenosis. Ann Otol Rhinol Laryngol 121:442–448
Smith MM, Cotton RT (2018) Diagnosis and management of laryngotracheal stenosis. Expert Rev Respir Med 12(8):709–717. https://doi.org/10.1080/17476348.2018.1495564
Hebra A, Powell DD, Smith CD, Othersen HB Jr (1991) Balloon tracheoplasty in children: results of a 15-year experience. J Pediatr Surg 26(8):957–961. https://doi.org/10.1016/0022-3468(91)90843-i
Jefferson ND, Cohen AP, Rutter MJ (2016) Subglottic stenosis. Semin Pediatr Surg 25(3):138–143. https://doi.org/10.1053/j.sempedsurg.2016.02.006
Lang M, Brietzke SE (2014) A systematic review and meta-analysis of endoscopic balloon dilation of pediatric subglottic stenosis. Otolaryngol Head Neck Surg 150:174–179. https://doi.org/10.1177/0194599813510867
Myer CM, O’Connor DM, Cotton RT (1994) Proposed grading system for subglottic stenosis based on endotracheal tube sizes. Ann Otol Rhinol Laryngol 103(4 Pt 1):319–323. https://doi.org/10.1177/000348949410300410
McCaffrey TV (1992) Classification of laryngotracheal stenosis. Laryngoscope 102:1335–1340
Hautefort C, Teissier N, Viala P, Van Den Abbeel T (2012) Balloon dilation laryngoplasty for subglottic stenosis in children: eight years’ experience. Arch Otolaryngol Head Neck Surg 138:235–240. https://doi.org/10.1001/archoto.2011.1439
Collins WO, Kalantar N, Rohrs HB, Silva RC (2012) The effects of balloon dilation laryngoplasty in children with congenital heart disease. Arch Otolaryngol Head Neck Surg 138:1136–1140. https://doi.org/10.1001/jamaoto.2013.676
Schweiger C, Manica D (2020) Ongoing laryngeal stenosis: conservative management and alternatives to tracheostomy. Front Pediatr 8:161. https://doi.org/10.3389/fped.2020.00161
Wentzel JL, Ahmad SM, Discolo CM, Gillespie MB, Dobbie AM, White DR (2014) Balloon laryngoplasty for pediatric laryngeal stenosis: case series and systematic review. Laryngoscope 124:1707–1712. https://doi.org/10.1002/lary.24524
Lee JC, Kim MS, Kim DJ, Park DH, Lee IW, Roh HJ, Lee BJ, Kim YA, Ko S, Sung ES (2019) Subglottic stenosis in children: our experience at a pediatric tertiary center for 8 years in South Korea. Int J Pediatr Otorhinolaryngol 121:64–67
Durden F, Sobol SE (2007) Balloon laryngoplasty as a primary treatment for subglottic stenosis. Arch Otolaryngol Head Neck Surg 133:772–775
Kurdi A, Alkhatib T, Malas M, Alshehri S, Alnori I (2019) Balloon laryngoplasty in pediatric population with subglottic stenosis: 5 years experience in King Abdulaziz University Hospital a Tertiary Center. Indian J Otolaryngol Head Neck Surg 71(2):186–189. https://doi.org/10.1007/s12070-019-01608-y
Avelino MG, Fernandes EJ (2014) Balloon laryngoplasty for subglottic stenosis caused by orotracheal intubation at a tertiary care pediatric hospital. Int Arch Otorhinolaryngol 18:39–42. https://doi.org/10.1055/s-0033-1358577
Acknowledgements
The authors have no conflict of interests to declare. This study is funded by Baskent University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tuzuner, A., Bas, C., Jafarov, S. et al. Respiratory problems and associated factors following endoscopic balloon dilatation procedure in children with acquired subglottic stenosıs. Eur Arch Otorhinolaryngol 279, 2493–2500 (2022). https://doi.org/10.1007/s00405-021-07208-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07208-3