Abstract
Introduction
The prevalence of stroke in SCD patients was reported to be around 4%; however, the pediatric category was among the higher risk group for stroke compared to young and middle age adults. Furthermore, the risk of OSA increases in SCD children. The objective of this study is to calculate the prevalence of stroke in children with SCD with and without obstructive sleep apnea.
Method
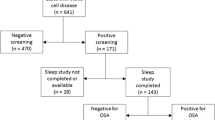
This is a cross-sectional study held at two major tertiary hospitals in Jeddah, Saudi Arabia. Inclusion criteria included patients aged between 2 and 18 at the time of enrollment with confirmed SCD. The primary outcome of the study was at least one documented episode of stroke over the last 3 years. OSA was assessed using PSQ.
Results
A total of 150 children with SCD were included in the study. The mean age was 9.6 (±4.3). Most of the sample (85.3%) were sickle-cell anemia with HbSS. Children who were positive for OSA were at higher odds of having a stroke [OR 2.97; 95% CI 1.13–7.75 (P = 0.02)]. The relationship between OSA and stroke was not significant in the multivariant analysis.
Conclusion
Patients who had OSA had a higher prevalence of stroke compared to non-OSA patients by 16% with almost three times higher odds. The difference was statistically significant in bivariant but not multivariant analysis. The rate of hospitalization, emergency visit, and blood transfusion were not affected by OSA status. Screening for OSA in high-risk patients such as SCD children and early management could prevent the risk of SCD complications.



Similar content being viewed by others
Availability of data and materials
All study is available upon request.
Code availability
STATA version 20.
Abbreviations
- SCD:
-
Sickle cell disease
- OSA:
-
Obstructive sleep apnea
- PSQ:
-
Pediatric sleep questionnaire
- PSG:
-
Polysomnography
- CVA:
-
Cerebral vascular accident
- Hb:
-
Hemoglobin
- AHI:
-
Apnea/Hypopnea Index
References
Piel FB et al (2013) Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet 381(9861):142–151
McGann PT, Hernandez AG, Ware RE (2017) Sickle cell anemia in sub-Saharan Africa: advancing the clinical paradigm through partnerships and research. Blood Jo Am Soc Hematol 129(2):155–161
Ware RE et al (2017) Sickle cell disease. Lancet 390(10091):311–323
Jastaniah W (2011) Epidemiology of sickle cell disease in Saudi Arabia. Ann Saudi Med 31:289–293
Zaini R (2016) Sickle-cell anemia and consanguinity among the Saudi Arabian population. Arch Med 8(3):3–15
Ambrose EE et al (2018) High birth prevalence of sickle cell disease in Northwestern Tanzania. Pediatr Blood Cancer 65(1):e26735
Oppong M et al (2020) Prevalence of sickle cell disorders and malaria infection in children aged 1–12 years in the Volta Region, Ghana: a community-based study. Malar J 19(1):426–426
Ndeezi G et al (2016) Burden of sickle cell trait and disease in the Uganda Sickle Surveillance Study (US3): a cross-sectional study. Lancet Glob Health 4(3):e195-200
Streetly A et al (2009) Implementation of universal newborn bloodspot screening for sickle cell disease and other clinically significant haemoglobinopathies in England: screening results for 2005–7. J Clin Pathol 62(1):26–30
Bouva MJ et al (2010) Implementing neonatal screening for haemoglobinopathies in the Netherlands. J Med Screen 17(2):58–65
Grosse R et al (2016) The prevalence of sickle cell disease and its implication for newborn screening in Germany (Hamburg metropolitan area). Pediatr Blood Cancer 63(1):168–170
Bardakdjian-Michau J et al (2009) Neonatal screening for sickle cell disease in France. J Clin Pathol 62(1):31–33
Alkot M et al (2018) Prevalence of complications of sickle cell disease at Makkah Al-Mukaramah, Saudi Arabia, 2017. Ann Clin Lab Res 6(1):226
Hawasawi ZM et al (1998) Sickle cell disease in childhood in Madina. Ann Saudi Med 18(4):293–295
De Montalembert M, Wang W (2013) Cerebrovascular complications in children with sickle cell disease. Handb Clin Neurol 113:1937–1943
Sundd P, Gladwin MT, Novelli EM (2019) Pathophysiology of sickle cell disease. Annu Rev Pathol 14:263–292
Ruhl AP et al (2019) Identifying clinical and research priorities in sickle cell lung disease. An official American Thoracic Society Workshop Report. Ann Am Thorac Soc 16(9):e17–e32
Ohene-Frempong K et al (1998) Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood 91(1):288–294
Mrad C et al (2017) Cerebrovascular accidents among african american adults with sickle cell disease: a nationwide outcomes and trend analysis over two decades. American Society of Hematology, Washington
Switzer JA et al (2006) Pathophysiology and treatment of stroke in sickle-cell disease: present and future. Lancet Neurol 5(6):501–512
El Sayed MM et al (1999) Characteristics of stroke in Hofuf, Saudi Arabia. Ann Saudi Med 19(1):27–31
Padmos M et al (1991) Two different forms of homozygous sickle cell disease occur in Saudi Arabia. Br J Haematol 79(1):93–98
El Mouzan M et al (1989) Variability of sickle cell disease in the Eastern Province of Saudi Arabia. J Pediatr 114(6):973–976
Katz ES, D’Ambrosio CM (2008) Pathophysiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc 5(2):253–262
Rosen CL et al (2014) Obstructive sleep apnea and sickle cell anemia. Pediatrics 134(2):273–281
Strauss T et al (2012) Upper airway lymphoid tissue size in children with sickle cell disease. Chest 142(1):94–100
Al-Otaibi T et al (2017) Prevalence of obstructive sleep apnea in children with sickle cell disease at a tertiary hospital in Saudi Arabia. Saudi Med J 38(6):616–620
Fonsah JY et al (2013) Obstructive sleep apnea in sickle-cell disease patients in Cameroon. J Neurol Sci 333:e717–e717
Yadav A, Strak JM, Hashmi S, Corrales-Medina FF, Brown DL (2014) Pediatric sleep and sleep medicine: presence of sleep disturbances in children with sickle cell disease using the Pediatric Sleep Questionnaire (psq). Am J Respir Crit Care Med 189:1
Jehan S et al (2018) Obstructive sleep apnea and stroke. Sleep Med Disord 2(5):120–125
Dyken ME, Im KB (2009) Obstructive sleep apnea and stroke. Chest 136(6):1668–1677
Katz T, Schatz J, Roberts CW (2018) Comorbid obstructive sleep apnea and increased risk for sickle cell disease morbidity. Sleep Breath 22(3):797–804
Robertson PL et al (1988) Stroke associated with obstructive sleep apnea in a child with sickle cell anemia. Ann Neurol 23(6):614–616
Goldstein NA et al (2011) Sleep-disordered breathing and transcranial Dopplers in sickle cell disease. Arch Otolaryngol Head Neck Surg 137(12):1263–1268
Alotaibi W et al (2018) Pediatric sickle cell disease and obstructive sleep apnea: a cross-sectional study in a tertiary pediatric center in Saudi Arabia. J Fam Commun Med 25(3):183–187
Chervin RD et al (2007) Pediatric sleep questionnaire. Arch Otolaryngol-Head Neck Surg 133(3):216–216
Peña-Zarza JA et al (2012) Utility of the pediatric sleep questionnaire and pulse oximetry as screening tools in pediatric patients with suspected obstructive sleep apnea syndrome. Sleep Disord 2012:1–6
Marks LJ et al (2018) Stroke prevalence in children with sickle cell disease in sub-saharan africa: a systematic review and meta-analysis. Glob Pediatr Health 5:2333794X18774970
Munube D et al (2016) Prevalence of stroke in children admitted with sickle cell anaemia to Mulago Hospital. BMC Neurol 16(1):175
Lagunju I, Sodeinde O (2012) Prospective measurement of stroke incidence in childhood sickle cell disease. Arch Dis Child 97(Suppl 1):A45–A45
Hermann DM, Bassetti CL (2016) Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery. Neurology 87(13):1407–1416
Sidman JD, Fry TL (1988) Exacerbation of sickle cell disease by obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 114(8):916–917
Kirkham FJ et al (2001) Nocturnal hypoxaemia and central-nervous-system events in sickle-cell disease. Lancet 357(9269):1656–1659
Reckley LK, Fernandez-Salvador C, Camacho M (2018) The effect of tonsillectomy on obstructive sleep apnea: an overview of systematic reviews. Nat Sci Sleep 10:105–110
Farrell AN et al (2018) Adenotonsillectomy in children with sickle cell disease and obstructive sleep apnea. Int J Pediatr Otorhinolaryngol 111:158–161
Finch P et al (2013) Effects of adenotonsillectomy on polysomnographic parameters in children with sickle cell disease. Pediatr Blood Cancer 60(7):E26–E28
Funding
This project had not been funded by any organization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I approve that I and other authors have no conflict of interest producing this work. No personal benefits will be gained publishing this paper.
Ethical approval
The project was approved by the unit of biological ethics in the Faculty of Medicine at King Abdulaziz University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abulhamail, A., Selati, S. & Alasqah, R. The association between obstructive sleep apnea and stroke in sickle-cell disease children. Eur Arch Otorhinolaryngol 279, 843–851 (2022). https://doi.org/10.1007/s00405-021-07125-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07125-5