Abstract
Purpose
After the 2 years of follow-up, we aimed to evaluate at 5 years the impact of human papillomavirus (HPV) status, tobacco, and initial treatment approach on progression-free survival (PFS) and overall survival (OS) of patients with oropharyngeal cancer (OPC) in France.
Methods
Papillophar study was designed as a prospective cohort of 340 OPC patients in 14 French hospitals. HPV-positive status (21.7%) was defined with PCR (positivity for HPV DNA and E6/E7 mRNA). Cox proportional hazard models were used to assess the relationship between PFS, OS, HPV, and other prognostic factors. The combined effect of HPV status with smoking, stage, or initial treatment on PFS was also evaluated.
Results
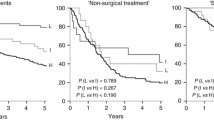
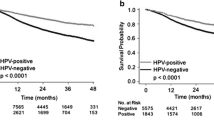
HPV-pos patients had better PFS than HPV-neg patients (HR = 0.46; 95% CI: 0.29–0.74), and worse for older patients (HR for 5-year age increase = 1.14), UICC stage 4 from the 7th TNM classification compared to stage 1–2 (HR = 2.58; CI: 1.33–5.00), and those having had radiotherapy (HR = 2.07; 95% CI: 1.36–3.16) or induction chemotherapy (HR = 2.11; 95% CI: 1.32–3.38) instead of upfront surgery. HPV-neg patients encountered a larger incidence of loco-regional disease than HPV-pos patients (31.5% and 14.0%, respectively, p = 0.0001). Distant metastases proportion was similar. HPV-neg patients developed more second primary tumor than HPV-pos patients (11.7% vs. 3.3%, p = 0.02).
Conclusions
5-year follow-up confirms the specifically improved prognosis in HPV-positive patients. The prognosis is nevertheless significantly modified through clinical and therapeutical variations.


Similar content being viewed by others
Abbreviations
- HPV:
-
Human papillomavirus
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- HPV-Pos:
-
HPV positive
- HPV-neg:
-
HPV negative
- OPC:
-
Oropharyngeal cancer
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Louie KS, Mehanna H, Sasieni P (2015) Trends in head and neck cancers in England from 1995 to 2011 and projections up to 2025. Oral Oncol 51(4):341–348. https://doi.org/10.1016/j.oraloncology.2015.01.002
Chaturvedi AK, Engels EA, Pfeiffer RM et al (2011) Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 29(32):4294–4301. https://doi.org/10.1200/JCO.2011.36.4596
Marur S, D’Souza G, Westra WH, Forastiere AA (2010) HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol 11(8):781–789. https://doi.org/10.1016/S1470-2045(10)70017-6
Ang KK, Harris J, Wheeler R et al (2010) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363(1):24–35. https://doi.org/10.1056/NEJMoa0912217
Benson E, Li R, Eisele D, Fakhry C (2014) The clinical impact of HPV tumor status upon head and neck squamous cell carcinomas. Oral Oncol 50(6):565–574. https://doi.org/10.1016/j.oraloncology.2013.09.008
Sedaghat AR, Zhang Z, Begum S et al (2009) Prognostic significance of human papillomavirus in oropharyngeal squamous cell carcinomas. Laryngoscope 119(8):1542–1549. https://doi.org/10.1002/lary.20533
Chaturvedi AK, Anderson WF, Lortet-Tieulent J et al (2013) Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol 31(36):4550–4559. https://doi.org/10.1200/JCO.2013.50.3870
Simard EP, Torre LA, Jemal A (2014) International trends in head and neck cancer incidence rates: differences by country, sex and anatomic site. Oral Oncol 50(5):387–403. https://doi.org/10.1016/j.oraloncology.2014.01.016
St Guily JL, Jacquard A-C, Prétet J-L et al (2011) Human papillomavirus genotype distribution in oropharynx and oral cavity cancer in France—The EDiTH VI study. J Clin Virol 51(2):100–104. https://doi.org/10.1016/j.jcv.2011.03.003
Chaturvedi AK, D’Souza G, Gillison ML, Katki HA (2016) Burden of HPV-positive oropharynx cancers among ever and never smokers in the US population. Oral Oncol 60:61–67. https://doi.org/10.1016/j.oraloncology.2016.06.006
Burki TK (2016) France announces tobacco legislation plan US legislation has little eff ect on chemotherapy prescribing. Lancet Oncol 15(12):e532. https://doi.org/10.1016/S1470-2045(14)70495-4
Chau NG, Rabinowits G, Haddad RI (2014) Human papillomavirus-associated oropharynx cancer (HPV-OPC): treatment options. Curr Treat Options Oncol 15(4):595–610. https://doi.org/10.1007/s11864-014-0309-1
Culié D, Garrel R, Viotti J et al (2018) Impact of HPV-associated p16-expression and other clinical factors on therapeutic decision-making in patients with oropharyngeal cancer: a GETTEC multicentric study. Eur J Surg Oncol 44(12):1908–1913. https://doi.org/10.1016/j.ejso.2018.05.022
Kamran SC, Qureshi MM, Jalisi S, Salama A, Grillone G, Truong MT (2017) Primary surgery-versus primary radiation-based treatment for locally advanced oropharyngeal cancer. Laryngoscope. https://doi.org/10.1002/lary.26903
Roden DF, Schreiber D, Givi B (2017) Triple-modality treatment in patients with advanced stage tonsil cancer. Cancer 123(17):3269–3276. https://doi.org/10.1002/cncr.30728
Gillison ML, Trotti AM, Harris J et al (2019) Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet 393(10166):40–50. https://doi.org/10.1016/S0140-6736(18)32779-X
Mehanna H, Robinson M, Hartley A et al (2019) Articles Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet 393:51–60. https://doi.org/10.1016/S0140-6736(18)32752-1
Lacau GJ, Rousseau A, Baujat B et al (2017) Oropharyngeal cancer prognosis by tumour HPV status in France: the multicentric Papillophar study. Oral Oncol 67:29–36. https://doi.org/10.1016/j.oraloncology.2017.01.012
Cubie HA, Cuschieri K (2013) Understanding HPV tests and their appropriate applications. Cytopathology 24(5):289–308. https://doi.org/10.1111/cyt.12083
Jung AC, Rickman D, Briolat J et al (2009) Biological and clinical relevance of transcriptionally active human papillomavirus (HPV) infection in oropharynx squamous cell carcinoma. Int J Cancer 126(8):1882–1894. https://doi.org/10.1002/ijc.24911
Fakhry C, Zhang Q, Nguyen-Tân F et al (2017) Development and validation of nomograms predictive of overall and progression-free survival in patients with oropharyngeal cancer. J Clin Oncol 35:4057–4065. https://doi.org/10.1200/JCO
Rodrigo JP, Heideman DAM, García-Pedrero JM et al (2014) Time trends in the prevalence of HPV in oropharyngeal squamous cell carcinomas in northern Spain (1990–2009). Int J Cancer 134(2):487–492. https://doi.org/10.1002/ijc.28355
Bozec A, Culie D, Poissonnet G, Dassonville O (2019) Current role of primary surgical treatment in patients with head and neck squamous cell carcinoma. Curr Opin Oncol. https://doi.org/10.1097/CCO.0000000000000531
Kelly JR, Park HS, An Y et al (2017) Upfront surgery versus definitive chemoradiotherapy in patients with human Papillomavirus-associated oropharyngeal squamous cell cancer. Oral Oncol 2018(79):64–70. https://doi.org/10.1016/j.oraloncology.2018.02.017
Seikaly H, Biron VL, Zhang H et al (2015) Role of primary surgery in the treatment of advanced oropharyngeal cancer. Head Neck 1:571–579
O’Sullivan B, Huang SH, Su J et al (2016) Development and validation of a staging system for HPV-related oropharyngeal cancer by the International Collaboration on Oropharyngeal cancer Network for Staging (ICON-S): a multicentre cohort study. Lancet Oncol 17(4):440–451. https://doi.org/10.1016/S1470-2045(15)00560-4
Mirghani H, Lacroix L, Rossoni C et al (2018) Does smoking alter the mutation profile of human papillomavirusedriven head and neck cancers? Eur J Cancer. https://doi.org/10.1016/j.ejca.2018.02.013
Huang SH, Perez-Ordonez B, Weinreb I et al (2013) Natural course of distant metastases following radiotherapy or chemoradiotherapy in HPV-related oropharyngeal cancer. Oral Oncol. https://doi.org/10.1016/j.oraloncology.2012.07.015
Fakhry C, Zhang Q, Nguyen-Tan F et al (2014) Human papillomavirus and overall survival after progression of oropharyngeal squamous cell carcinoma. J Clin Oncol. https://doi.org/10.1200/JCO.2014.55.1937
Faraji F, Eisele DW, Fakhry C (2017) Emerging insights into recurrent and metastatic human papillomavirus-related oropharyngeal squamous cell carcinoma. Laryngoscope Investig Otolaryngol. https://doi.org/10.1002/lio2.37
Martel M, Alemany L, Taberna M et al (2017) The role of HPV on the risk of second primary neoplasia in patients with oropharyngeal carcinoma. Oral Oncol 64:37–43. https://doi.org/10.1016/j.oraloncology.2016.11.011
IARC France (2007) Tobacco control: reversal of risk after. 11.
Acknowledgements
The authors thank Sarah Sahli from the Clinical Research Unit of East of Paris (URC-Est), Saint Antoine University Hospital (AP-HP) for study coordination and logistics. They thank all members of the Papillophar Group: G. Agius (University Hospital, Poitiers), S. Albert (AP-HP, Bichat Hospital; University Paris 7, Paris), E. Babin (University Hospital, Caen), C. Bach (Foch Hospital, Suresnes), J.M. Badet (Jean Minjoz University Hospital, Besançon), C. Badoual (AP-HP, Georges Pompidou Hospital and University Paris 5, Paris), A.C. Baglin (Foch Hospital, Suresnes), A. Beby Defaux (University Hospital, Poitiers), C. Bertolus (AP-HP, Pitié-Salpétrière Hospital and University Paris 6, Paris), K. Blanc-Fournier (François Baclesse Regional Centre, Unicancer, Caen), E. Cassagneau (Hotel-Dieu University Hospital, Nantes), V. Dalstein (Maison Blanche University Hospital, Reims), C. Debry (Hautepierre University Hospital, Strasbourg), D. de Raucourt (François Baclesse Regional Centre, Unicancer, Caen), M.D. Diebold (Maison Blanche University Hospital, Reims), S. Hans (AP-HP, Georges Pompidou Hospital; University Paris 5, Paris), M. Hourseau (AP-HP, Bichat Hospital; University Paris 7, Paris), B. Kantelip (Jean Minjoz University Hospital, Besançon), R.Lacave (AP-HP, Tenon Hospital, Paris; UPMC-Sorbonne Universities, Paris), E. Lechapt Zalcman (University Hospital, Caen), M. Lefevre (AP-HP, Tenon Hospital, Paris; UPMCSorbonne Universities, Paris), J. Lerat (University Hospital, Limoges), P. Levillain (University Hospital, Poitiers), O. Mauvais (Jean Minjoz University Hospital, Besançon), A. Mechine (Hautepierre University Hospital, Strasbourg), J.C. Merol (Maison Blanche University Hospital, Reims), H. Mirghani (Gustave Roussy Centre, Unicancer, Villejuif), S. Morinière (Bretonneau University Hospital, Tours), C. Mougin (Jean Minjoz University Hospital, Besançon), C. Rousselot (Bretonneau University Hospital, Tours), T. Simon (AP-HP, Department of Clinical Pharmacology, Clinical Research Platform (URC-Est-CRC-CRB), Saint-Antoine Hospital, Paris; UPMC-Sorbonne Universities, Paris), P. Soussan (AP-HP, Tenon Hospital, Paris; UPMC-Sorbonne Universities, Paris), and A. Touzé (University Institute of Technology, Tours).
Funding
This work was funded by the Programme Hospitalier de Recherche Clinique, French Ministry of Health (grant numbers AOM 08104, AOM 11 293). The sponsor was Assistance Publique-Hôpitaux de Paris (Délégation à la Recherche Clinique et à l’Innovation). The funding source had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to the data and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
AR updated and analyzed the data. DC wrote the first draft. All the authors were involved in writing, review, and approval of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any potential conflicts of interest.
Ethical standards
This study (NCT00918710) was approved by a national ethical committee and the French data protection authority.
Informed consent
All participating patients provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Culié, D., Rousseau, A., Pretet, JL. et al. HPV status and therapeutic initial strategy impact on survival and oncologic outcomes: 5-year results from the multicentric prospective cohort of oropharyngeal cancers Papillophar. Eur Arch Otorhinolaryngol 279, 3071–3078 (2022). https://doi.org/10.1007/s00405-021-07117-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07117-5