Abstract
Purpose
The significant pathogens associated with paediatric cervical suppurative lymphadenitis (CSL) are unclarified, and there is a lack of clinical evaluations of antibiotic regimens in paediatric CSL. We aimed to (1) explore the bacterial findings and the associated primary sites of infection in paediatric cases of CSL and (2) evaluate the clinical outcomes in patients treated with different antibiotic regimens.
Methods
All children (< 18 years) treated for non-mycobacterium CSL at the Department of Otorhinolaryngology, Aarhus University Hospital, from 2001 to 2018 were retrospectively evaluated.
Results
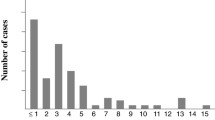
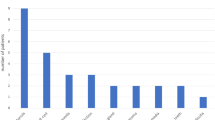
Eighty-five patients were included in the study. The prevalent isolates were S. aureus (57%), S. pyogenes (17%), non-haemolytic streptococci (11%), and F. necrophorum (3%). The primary sites of infection were identified in 30 (35%) patients. The most common sites were the oropharynx (n = 15), the middle ear (n = 10), and the skin (n = 5). All patients were treated with surgical incision and antibiotics. No statistically significant differences were found between patients treated with antibiotics covering streptococci (n = 60) versus antibiotics covering streptococci and S. aureus (n = 25) in terms of duration of hospitalisation (median 4 vs 4 days, p = 0.26), altered antibiotic treatment because of insufficient clinical or biochemical progress (7% vs 12%, p = 0.41), and abscess recurrence (8% vs 12%, p = 0.69).
Conclusion
S. aureus was the predominant pathogen in paediatric CSL at all cervical levels, and even in cases with evidence of primary site infection not normally associated with S. aureus. We were unable to underscore the importance of antibiotic treatment covering S. aureus based on evaluation of the clinical outcomes.
Similar content being viewed by others
Availability of data
Anonymized data can be obtained from the corresponding author upon request.
Code availability
Not applicable.
References
Cherry JD, Harrison GJ, Kaplan S et al (2018) Feigin and Cherry’s textbook of pediatric infectious diseases, vol 8. Elsevier, Philadelphia, PA
Gosche JR, Vick L (2006) Acute, subacute, and chronic cervical lymphadenitis in children. Semin Pediatr Surg 15:99–106. https://doi.org/10.1053/j.sempedsurg.2006.02.007
Larsson LO, Bentzon MW, Berg Kelly K et al (1994) Palpable lymph nodes of the neck in Swedish school children. Acta Paediatr Int J Paediatr 83:1091–1094. https://doi.org/10.1111/j.1651-2227.1994.tb12992.x
Courtney MJ, Miteff A, Mahadevan M (2007) Management of pediatric lateral neck infections: does the adage “... never let the sun go down on undrained pus …” hold true? Int J Pediatr Otorhinolaryngol 71:95–100. https://doi.org/10.1016/j.ijporl.2006.09.009
Hieber JP, Davis AT (1976) Staphylococcal cervical adenitis in young infants. Pediatrics 57:424–426
Lindquist NR, Patro A, Gitomer SA, Cañadas KT (2019) Pediatric acute unilateral suppurative lymphadenitis: the role of antibiotic susceptibilities at a large tertiary pediatric care center. Int J Pediatr Otorhinolaryngol 120:11–14. https://doi.org/10.1016/j.ijporl.2019.01.024
Guss J, Kazahaya K (2007) Antibiotic-resistant Staphylococcus aureus in community-acquired pediatric neck abscesses. Int J Pediatr Otorhinolaryngol 71:943–948. https://doi.org/10.1016/j.ijporl.2007.03.006
Lang S, Kansy B (2014) Cervical lymph node diseases in children. GMS Curr Top Otorhinolaryngol Head Neck Surg. https://doi.org/10.3205/cto000111
Rusan M, Klug TE, Ovesen T (2009) An overview of the microbiology of acute ear, nose and throat infections requiring hospitalisation. Eur J Clin Microbiol Infect Dis 28:243–251. https://doi.org/10.1007/s10096-008-0619-y
Marchisio P, Ghisalberti E, Fusi M et al (2007) Paranasal sinuses and middle ear infections: what do they have in common? Pediatr Allergy Immunol 18:31–34. https://doi.org/10.1111/j.1399-3038.2007.00630.x
Arguedas A, Dagan R, Soley C et al (2003) Microbiology of otitis media in Costa Rican children, 1999 through 2001. Pediatr Infect Dis J 22:1063–1068. https://doi.org/10.1097/01.inf.0000101189.81501.e9
Nielsen HUK, Konradsen HB, Lous J, Frimodt-Møller N (2004) Nasopharyngeal pathogens in children with acute otitis media in a low-antibiotic use country. Int J Pediatr Otorhinolaryngol 68:1149–1155. https://doi.org/10.1016/j.ijporl.2004.04.008
Brook I (2007) Microbiology and principles of antimicrobial therapy for head and neck infections. Infect Dis Clin North Am 21:355–391. https://doi.org/10.1016/j.idc.2007.03.014
Clebak KT, Malone MA (2018) Skin infections. Primary Care Clin Office Pract 45:433–454. https://doi.org/10.1016/j.pop.2018.05.004
Simo R, Hartley C, Rapado F et al (1998) Microbiology and antibiotic treatment of head and neck abscesses in children. Clin Otolaryngol Allied Sci 23:164–168. https://doi.org/10.1046/j.1365-2273.1998.00120.x
Yamauchi T, Ferrieri P, Anthony BF (1980) The aetiology of acute cervical adenitis in children: serological and bacteriological studies. J Med Mircrobiol 13:37–43. https://doi.org/10.1099/00222615-13-1-37
Serour F, Gorenstein A, Somekh E (2002) Needle aspiration for suppurative cervical lymphadenitis. Clin Pediatr 41:471–474. https://doi.org/10.1177/000992280204100703
Cengiz AB, Kara A, Kanra G et al (2004) Acute neck infections in children. Turkish J Pediatr 46:153–158
Baek MY, Park KH, We JH, Park SE (2010) Needle aspiration as therapeutic management for suppurative cervical lymphadenitis in children. Korean J Pediatr 53:801–804. https://doi.org/10.3345/kjp.2010.53.8.801
Georget E, Gauthier A, Brugel L et al (2014) Acute cervical lymphadenitis and infections of the retropharyngeal and parapharyngeal spaces in children. BMC Ear, Nose Throat Disord 14:1–7. https://doi.org/10.1186/1472-6815-14-8
Worley ML, Seif JM, Whigham AS et al (2015) Suppurative cervical lymphadenitis in infancy: microbiology and sociology. Clin Pediatr 54:629–634. https://doi.org/10.1177/0009922815584548
Kimia AA, Rudloe TF, Aprahamian N et al (2019) Predictors of a drainable suppurative adenitis among children presenting with cervical adenopathy. Am J Emerg Med 37:109–113. https://doi.org/10.1016/j.ajem.2018.05.004
Brook I (1980) Aerobic and anaerobic bacteriology of cervical adenitis in children. Clin Pediatr 19:693–696. https://doi.org/10.1177/000992288001901010
Robbins KT, Clayman G, Levine PA et al (2002) Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg 128:751–758. https://doi.org/10.1001/archotol.128.7.751
European Society of Clinical Microbiology and Infectious Diseases (2019) EUCAST: clinical breakpoints and dosing of antibiotics. In: EUCAST, European committee on antimicrobial susceptibility testing. http://www.eucast.org/clinical_breakpoints/. Accessed 12 Sep 2021
Zimmermann P, Tebruegge M, Curtis N, Ritz N (2015) The management of non-tuberculous cervicofacial lymphadenitis in children: asystematic review and meta-analysis. J Infect 71:9–18. https://doi.org/10.1016/j.jinf.2015.02.010
Barton LL, Feigin RD (1974) Childhood cervical lymphadenitis: a reappraisal. J Pediatr 84:846–852. https://doi.org/10.1016/S0022-3476(74)80761-4
Konno M, Baba S, Mikawa H et al (2006) Study of upper respiratory tract bacterial flora: First report. Variations in upper respiratory tract bacterial flora in patients with acute upper respiratory tract infection and healthy subjects and variations by subject age. J Infect Chemother 12:83–96. https://doi.org/10.1007/s10156-006-0433-3
Bluestone CD, Stephenson JS, Martin LM (1992) Ten-year review of otitis media pathogens. Pediatr Inf Dis J 11:S7-11. https://doi.org/10.1097/00006454-199208001-00002
Pichichero ME, Pichichero CL (1995) Persistent acute otitis media: I. Causative pathogens. Pediatr Inf Dis J 14:178–183. https://doi.org/10.1097/00006454-199503000-00002
Suzuki K, Kurono Y, Ikeda K et al (2020) The seventh nationwide surveillance of six otorhinolaryngological infectious diseases and the antimicrobial susceptibility patterns of the isolated pathogens in Japan. J Infect Chemother 26:890–899. https://doi.org/10.1016/j.jiac.2020.05.020
Suzuki K, Kurono Y, Ikeda K et al (2015) Nationwide surveillance of 6 otorhinolaryngological infectious diseases and antimicrobial susceptibility pattern in the isolated pathogens in Japan. J Infect Chemother 21:483–491. https://doi.org/10.1016/j.jiac.2015.03.005
Pelucchi C, Grigoryan L, Galeone C et al (2012) Guideline for management of acute sore throat. Clin Microbiol Inf 18:1–27. https://doi.org/10.1111/j.1469-0691.2012.03766.x
Kronman MP, Zhou C, Mangione-Smith R (2014) Bacterial prevalence and antimicrobial prescribing trends for acute respiratory tract infections. Pediatrics 134:e956–e965. https://doi.org/10.1542/peds.2014-0605
Hagelskjær Kristensen L, Prag J (2008) Lemierre’s syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis 27:779–789. https://doi.org/10.1007/s10096-008-0496-4
Klug TE, Henriksen JJ, Rusan M et al (2014) Antibody development to Fusobacterium necrophorum in patients with peritonsillar abscess. Eur J Clin Microbiol Infect Dis 33:1733–1739. https://doi.org/10.1007/s10096-014-2130-y
Klug TE, Rusan M, Fuursted K et al (2016) A systematic review of Fusobacterium necrophorum-positive acute tonsillitis: prevalence, methods of detection, patient characteristics, and the usefulness of the Centor score. Eur J Clin Microbiol Infect Dis 35:1903–1912. https://doi.org/10.1007/s10096-016-2757-y
Stergiopoulou T, Walsh TJ (2016) Fusobacterium necrophorum otitis and mastoiditis in infants and young toddlers. Eur J Clin Microbiol Infect Dis 35:735–740. https://doi.org/10.1007/s10096-016-2612-1
Brook I (2015) Fusobacterial head and neck infections in children. Int J Pediatr Otorhinolaryngol 79:953–958. https://doi.org/10.1016/j.ijporl.2015.04.045
Klug TE (2014) Incidence and microbiology of peritonsillar abscess: the influence of season, age, and gender. Eur J Clin Microbiol Infect Dis 33:1163–1167. https://doi.org/10.1007/s10096-014-2052-8
Neff L, Newland JG, Sykes KJ et al (2013) Microbiology and antimicrobial treatment of pediatric cervical lymphadenitis requiring surgical intervention. Int J Pediatr Otorhinolaryngol 77:817–820. https://doi.org/10.1016/j.ijporl.2013.02.018
Funding
The authors received no financial support to declare that are relevant to the content of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by NØN, CN and TEK. Microbiological review was performed by TG. The first draft of the manuscript was written by NØN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors received no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
The study was approved by the Danish Data Protection Agency (1-16-02-587-18) and the Danish Patient Safety Authority (3-3013-2919/1). In accordance with Danish law, the study was not reported to the Ethics Committee of Aarhus County.
Consent to participate/publication
According to Danish law, it is illegal to contact patients to obtain informed consent in retrospective studies, but permission to conduct the study was given by the Danish Patient Safety Authority.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nielsen, N.Ø., Nørlinger, C., Greve, T. et al. Cervical suppurative lymphadenitis in children: microbiology, primary sites of infection, and evaluation of antibiotic treatment. Eur Arch Otorhinolaryngol 279, 3053–3062 (2022). https://doi.org/10.1007/s00405-021-07115-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07115-7