Abstract
Purpose
This study aimed to comprehensively review the literature and synthesize relevant data to examine the pooled prevalence of poor sleep quality (sleep impairment) and assess overall sleep quality in patients with tinnitus.
Methods
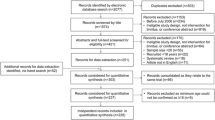
This meta-analysis systematically searched both English (PubMed, Embase, and Web of Science) and Chinese (Wanfang Data Chinese database, Veep Chinese Database, and Chinese National Knowledge Infrastructure) databases. Data extraction and quality assessment were independently performed by two authors. The pooled prevalence of sleep impairment and poor sleep quality was calculated via a random-effects model. Sub-group and sensitivity analyses were performed to explore the source of heterogeneity.
Results
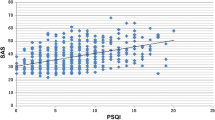
A total of seven studies were included with a total sample of 3041 tinnitus participants. The pooled prevalence of sleep impairment was 53.5% (95% confidence interval: 40.2–66.8%) and the I2 was 97.8% (Q = 7.90, p = 0.000). There were significant differences in the prevalence of poor sleep quality between males and females (39.1% vs. 44.6%, P = 0.034), between different PSQI cut-off values ≥ 7 and > 5 (53.1% vs. 53.8%, P = 0.000), and between sample sizes > 200 and ≤ 200 (54.0% vs. 52.7%, P = 0.000). In non-Asia area, the prevalence (56.6%, 95% CI: 42.6–70.5%) was lower than that in Asia areas (34.5%, 95% CI: 25.7–43.3%).
Conclusion
Sleep impairment is common among patients with tinnitus. Development of interventions for conditions associated with poor sleep quality should be recommended to offer a safe and efficacious solution for this population.




Similar content being viewed by others
Availability of data and materials
All data generated or analyzed during this study are included in the article.
Code availability
Not applicable.
References
de Almondes KM, Costa MV, Malloy-Diniz LF, Diniz BS (2016) Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res 77:109–115. https://doi.org/10.1016/j.jpsychires.2016.02.021
Liu X, Chen H, Bo Q-G et al (2017) Poor sleep quality and nightmares are associated with non-suicidal self-injury in adolescents. Eur Child Adolesc Psychiatry 26:271–279. https://doi.org/10.1007/s00787-016-0885-7
Kalmbach DA, Arnedt JT, Song PX et al (2017) Sleep disturbance and short sleep as risk factors for depression and perceived medical errors in first-year residents. Sleep. https://doi.org/10.1093/sleep/zsw073
Zhang B, Wing Y-K (2006) Sex differences in insomnia: a meta-analysis. Sleep 29:85–93. https://doi.org/10.1093/sleep/29.1.85
Mathias JL, Cant ML, Burke ALJ (2018) Sleep disturbances and sleep disorders in adults living with chronic pain: a meta-analysis. Sleep Med 52:198–210. https://doi.org/10.1016/j.sleep.2018.05.023
Roth T (2007) Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med 3:S7-10
Ratcliff R, Van Dongen HPA (2009) Sleep deprivation affects multiple distinct cognitive processes. Psychon Bull Rev 16:742–751. https://doi.org/10.3758/PBR.16.4.742
Li L, Wang Y-Y, Wang S-B et al (2018) Prevalence of sleep disturbances in Chinese university students: a comprehensive meta-analysis. J Sleep Res 27:e12648. https://doi.org/10.1111/jsr.12648
Chiu H-Y, Lee H-C, Chen P-Y et al (2018) Associations between sleep duration and suicidality in adolescents: a systematic review and dose–response meta-analysis. Sleep Med Rev 42:119–126. https://doi.org/10.1016/j.smrv.2018.07.003
Reynolds SA, Ebben MR (2017) The cost of insomnia and the benefit of increased access to evidence-based treatment: cognitive behavioral therapy for insomnia. Sleep Med Clin 12:39–46. https://doi.org/10.1016/j.jsmc.2016.10.011
McCormack A, Edmondson-Jones M, Somerset S, Hall D (2016) A systematic review of the reporting of tinnitus prevalence and severity. Hear Res 337:70–79. https://doi.org/10.1016/j.heares.2016.05.009
Tyler RS, Baker LJ (1983) Difficulties experienced by tinnitus sufferers. J Speech Hear Disord 48:150–154. https://doi.org/10.1044/jshd.4802.150
Pinto PCL, Marcelos CM, Mezzasalma MA et al (2014) Tinnitus and its association with psychiatric disorders: systematic review. J Laryngol Otol 128:660–664. https://doi.org/10.1017/S0022215114001030
Zarenoe R, Hällgren M, Andersson G, Ledin T (2017) Working memory, sleep, and hearing problems in patients with tinnitus and hearing loss fitted with hearing aids. J Am Acad Audiol 28:141–151. https://doi.org/10.3766/jaaa.16023
Inagaki Y, Suzuki N, Oishi N et al (2020) Personality and sleep evaluation of patients with tinnitus in Japan. Psychiatr Q. https://doi.org/10.1007/s11126-020-09794-7
Xu Y, Yao J, Zhang Z, Wang W (2016) Association between sleep quality and psychiatric disorders in patients with subjective tinnitus in China. Eur Arch Otorhinolaryngol 273:3063–3072. https://doi.org/10.1007/s00405-016-3906-8
Lu T, Li S, Ma Y et al (2020) Positive correlation between tinnitus severity and poor sleep quality prior to tinnitus onset: a retrospective study. Psychiatr Q 91:379–388. https://doi.org/10.1007/s11126-019-09708-2
Hébert S, Fullum S, Carrier J (2011) Polysomnographic and quantitative electroencephalographic correlates of subjective sleep complaints in chronic tinnitus. J Sleep Res 20:38–44. https://doi.org/10.1111/j.1365-2869.2010.00860.x
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Rostom A, Dubé C, Cranney A, et al (2004) Appendix D. Quality Assessment Forms. Agency for Healthcare Research and Quality (US)
Jia R, Liu B, Cheng L, Sun FX (2019) [Clinical research on sleep quality in patients with tinnitus]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi J Clin Otorhinolaryngol Head Neck Surg 33(10):961–965. https://doi.org/10.13201/j.issn.1001-1781.2019.10.015
Li Y-L, Hsu Y-C, Lin C-Y, Wu J-L (2021) Sleep disturbance and psychological distress in adult patients with tinnitus. J Formos Med Assoc Taiwan Yi Zhi S0929–6646(21):00353–00363. https://doi.org/10.1016/j.jfma.2021.07.022
Oosterloo BC, de Feijter M, Croll PH et al (2021) Cross-sectional and longitudinal associations between tinnitus and mental health in a population-based sample of middle-aged and elderly persons. JAMA Otolaryngol Neck Surg 147:708–716. https://doi.org/10.1001/jamaoto.2021.1049
Yongli S, Liu Qi, Yang C, Dingjun Z (2021) Influencing factors of anxiety and depression in patients with chronic tinnitus. J Audiol Speech Pathol 29:398–402
Benbir G, Demir AU, Aksu M et al (2015) Prevalence of insomnia and its clinical correlates in a general population in Turkey. Psychiatry Clin Neurosci 69:543–552. https://doi.org/10.1111/pcn.12252
Cao X-L, Wang S-B, Zhong B-L et al (2017) The prevalence of insomnia in the general population in China: a meta-analysis. PLoS ONE 12:e0170772. https://doi.org/10.1371/journal.pone.0170772
Leger D, Guilleminault C, Pierre J (2000) Prevalence of insomnia in a survey of 12 778 adults in France. J Sleep Res 8
Kiejna A, Wojtyniak B, Rymaszewska J, Stokwiszewski J (2003) Prevalence of insomnia in Poland — results of the National Health Interview Survey. Acta Neuropsychiatr 15:68–73. https://doi.org/10.1034/j.1601-5215.2003.00011.x
Kim KW, Kang S-H, Yoon I-Y et al (2017) Prevalence and clinical characteristics of insomnia and its subtypes in the Korean elderly. Arch Gerontol Geriatr 68:68–75. https://doi.org/10.1016/j.archger.2016.09.005
Xiang Y-T, Ma X, Cai Z-J et al (2008) The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep 31:1655–1662. https://doi.org/10.1093/sleep/31.12.1655
Ohayon MM, Sagales T (2010) Prevalence of insomnia and sleep characteristics in the general population of Spain. Sleep Med 11:1010–1018. https://doi.org/10.1016/j.sleep.2010.02.018
Ohayon MM (2002) Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 6:97–111. https://doi.org/10.1053/smrv.2002.0186
Dai J, Chiu HFK, Xiang Y-T et al (2013) The prevalence of insomnia and its socio-demographic and clinical correlates in older adults in rural China: a pilot study. Aging Ment Health 17:761–765. https://doi.org/10.1080/13607863.2013.781117
Johnson EO, Roth T, Schultz L, Breslau N (2006) Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics 117:e247-256. https://doi.org/10.1542/peds.2004-2629
Quan SA, Li YC, Li WJ et al (2016) Gender differences in sleep disturbance among elderly koreans: hallym aging study. J Korean Med Sci 31:1689–1695. https://doi.org/10.3346/jkms.2016.31.11.1689
Hartmann JA, Carney CE, Lachowski A, Edinger JD (2015) Exploring the construct of subjective sleep quality in patients with insomnia. J Clin Psychiatry 76:e768-773. https://doi.org/10.4088/JCP.14m09066
Lu L, Wang S-B, Rao W et al (2019) The prevalence of sleep disturbances and sleep quality in older chinese adults: a comprehensive meta-analysis. Behav Sleep Med 17:683–697. https://doi.org/10.1080/15402002.2018.1469492
Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM (2018) Sleep quality during pregnancy: a meta-analysis. Sleep Med Rev 38:168–176. https://doi.org/10.1016/j.smrv.2017.06.005
Alsaadi SM, McAuley JH, Hush JM et al (2013) Detecting insomnia in patients with low back pain: accuracy of four self-report sleep measures. BMC Musculoskelet Disord 14:196. https://doi.org/10.1186/1471-2474-14-196
Fictenberg NL, Putnam SH, Mann NR et al (2001) Insomnia screening in postacute traumatic brain injury: utility and validity of the Pittsburgh Sleep Quality Index. Am J Phys Med Rehabil 80:339–345. https://doi.org/10.1097/00002060-200105000-00003
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HG and WK contributed equally to this manuscript, and they are the co-first authors. All authors contributed to the study conception and design. Material preparation, and data collection and analysis were performed by HG and WK. The first draft of the manuscript was written by HG, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Additional declarations for articles in life science journals that report the results of studies involving humans and/or animals.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethics approval
All analyses were based on previous published studies; thus, no ethical approval or patient consent were required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gu, H., Kong, W., Yin, H. et al. Prevalence of sleep impairment in patients with tinnitus: a systematic review and single-arm meta-analysis. Eur Arch Otorhinolaryngol 279, 2211–2221 (2022). https://doi.org/10.1007/s00405-021-07092-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07092-x