Abstract
Purpose
The progressive expansion of the technology that facilitates the development of three-dimensional (3D) printing within the field of otorhinolaryngology has opened up a new study front in medicine. The objective of this study is to systematically review scientific publications describing the development of 3D models having applications in otorhinolaryngology, with emphasis on subareas with a large number of publications, as well as the countries in which the publications are concentrated.
Methods
In this literature review, specific criteria were used to search for publications on 3D models. The review considered articles published in English on the development of 3D models to teach otorhinolaryngology. The studies with presurgical purposes or without validation of the task by surgeons were excluded from this review.
Results
This review considered 39 articles published in 10 countries between 2012 and 2021. The works published prior to 2012 were not considered as per the inclusion criteria for the research. Among the 39 simulators selected for review, otology models comprised a total of 15 publications (38%); they were followed by rhinology, with 12 (31%); laryngology, with 8 (21%); and head and neck surgery, with 4 publications (10%).
Conclusion
The use of 3D technology and printing is well established in the context of surgical education and simulation models. The importance of developing new technological tools to enhance 3D printing and the current limitations in obtaining appropriate animal and cadaver models signify the necessity of investing more in 3D models.


Similar content being viewed by others
Availability of data and material
My manuscript has no associated data.
Code availability
Not applicable.
References
Deonarain AR, Harrison RV, Gordon KA, Looi T, Agur AMR, Estrada M, Wolter NE, Propst EJ (2021) Synthetic simulator for surgical training in tracheostomy and open airway surgery. Laryngoscope 131:E2378–E2386. https://doi.org/10.1002/lary.29359
Lee M, Ang C, Andreadis K, Shin J, Rameau A (2021) An open-source three-dimensionally printed laryngeal model for injection laryngoplasty training. Laryngoscope 131:E890–E895. https://doi.org/10.1002/lary.28952
Vaitaitis VJ, Dunham ME, Kwon YC, Mayer WC, Evans AK, Baker AJ, Walker KD, Cespedes GD, Stanley A, Opiri M (2020) A surgical simulator for tympanostomy tube insertion incorporating capacitive sensing technology to track instrument placement. Otolaryngol Head Neck Surg 162:343–345. https://doi.org/10.1177/0194599820901684
Gadaleta DJ, Huang D, Rankin N, Hsue V, Sakkal M, Bovenzi C, Huntley CT, Willcox T, Pelosi S, Pugliese R, Ku B (2020) 3D printed temporal bone as a tool for otologic surgery simulation. Am J Otolaryngol 41:102273. https://doi.org/10.1016/j.amjoto.2019.08.004
Alrasheed AS, Nguyen LHP, Mongeau L, Funnell WRJ, Tewfik MA (2017) Development and validation of a 3D-printed model of the ostiomeatal complex and frontal sinus for endoscopic sinus surgery training. Int Forum Allergy Rhinol 7:837–841. https://doi.org/10.1002/alr.21960
Gabrysz-Forget F, Rubin S, Nepomnayshy D, Dolan R, Yarlagadda B (2020) Development and validation of a novel surgical simulation for parotidectomy and facial nerve dissection. Otolaryngol Head Neck Surg 163:344–347. https://doi.org/10.1177/0194599820913587
Alwani MM, Svenstrup TJ, Bandali EH, Sharma D, Higgins TS, Wu AW, Shipchandler TZ, Illing EA, Ting JY (2020) Validity testing of a three-dimensionally printed endoscopic sinonasal surgery simulator. Laryngoscope 130:2748–2753. https://doi.org/10.1002/lary.28356
Sparks D, Kavanagh KR, Vargas JA, Valdez TA (2020) 3D printed myringotomy and tube simulation as an introduction to otolaryngology for medical students. Int J Pediatr Otorhinolaryngol 128:109730. https://doi.org/10.1016/j.ijporl.2019.109730
Wong V, Unger B, Pisa J, Gousseau M, Westerberg B, Hochman JB (2019) Construct validation of a printed bone substitute in otologic education. Otol Neurotol 40:e698–e703. https://doi.org/10.1097/MAO.0000000000002285
Low CM, Morris JM, Matsumoto JS, Stokken JK, O’Brien EK, Choby G (2019) Use of 3D-printed and 2D-illustrated international frontal sinus anatomy classification anatomic models for resident education. Otolaryngol Head Neck Surg 161:705–713. https://doi.org/10.1177/0194599819860832
Reighard CL, Green K, Powell AR, Rooney DM, Zopf DA (2019) Development of a high fidelity subglottic stenosis simulator for laryngotracheal reconstruction rehearsal using 3D printing. Int J Pediatr Otorhinolaryngol 124:134–138. https://doi.org/10.1016/j.ijporl.2019.05.027
Hoetzenecker K, Chan HHL, Frommlet F, Schweiger T, Keshavjee S, Waddell TK, Klepetko W, Irish JC, Yasufuku K (2019) 3D models in the diagnosis of subglottic airway stenosis. Ann Thorac Surg 107:1860–1865. https://doi.org/10.1016/j.athoracsur.2019.01.045
Yoshiyasu Y, Chang DR, Bunegin L, Lin RP, Aden JK, Prihoda TJ, Weitzel EK, McMains KC, Malekzadeh S, Bowe SN, Chen PG (2019) Construct validity of a low-cost medium-fidelity endoscopic sinus surgery simulation model. Laryngoscope 129:1505–1509. https://doi.org/10.1002/lary.27748
Reighard CL, Green K, Rooney DM, Zopf DA (2019) Development of a novel, low-cost, high-fidelity cleft lip repair surgical simulator using computer-aided design and 3-dimensional printing. JAMA Facial Plast Surg 21:77–79. https://doi.org/10.1001/jamafacial.2018.1237
Maza G, VanKoevering KK, Yanez-Siller JC, Baglam T, Otto BA, Prevedello DM, Carrau RL (2019) Surgical simulation of a catastrophic internal carotid artery injury: a laser-sintered model. Int Forum Allergy Rhinol 9:53–59. https://doi.org/10.1002/alr.22178
Cote V, Schwartz M, Arbouin Vargas JF, Canfarotta M, Kavanagh KR, Hamdan U, Valdez TA (2018) 3-Dimensional printed haptic simulation model to teach incomplete cleft palate surgery in an international setting. Int J Pediatr Otorhinolaryngol 113:292–297. https://doi.org/10.1016/j.ijporl.2018.08.016
Zhang XD, Li ZH, Wu ZS, Lin W, Lin WJ, Lin JC, Zhuang LM (2018) A novel three-dimensional-printed paranasal sinus-skull base anatomical model. Eur Arch Otorhinolaryngol 275:2045–2049. https://doi.org/10.1007/s00405-018-5051-z
Hsieh TY, Cervenka B, Dedhia R, Strong EB, Steele T (2018) Assessment of a patient-specific, 3-dimensionally printed endoscopic sinus and skull base surgical model. JAMA Otolaryngol Head Neck Surg 144:574–579. https://doi.org/10.1001/jamaoto.2018.0473
Nguyen Y, Mamelle E, De Seta D, Sterkers O, Bernardeschi D, Torres R (2017) Modifications to a 3D-printed temporal bone model for augmented stapes fixation surgery teaching. Eur Arch Otorhinolaryngol 274:2733–2739. https://doi.org/10.1007/s00405-017-4572-1
Takahashi K, Morita Y, Ohshima S, Izumi S, Kubota Y, Yamamoto Y, Takahashi S, Horii A (2017) Creating an optimal 3D printed model for temporal bone dissection training. Ann Otol Rhinol Laryngol 126:530–536. https://doi.org/10.1177/0003489417705395
Ha JF, Morrison RJ, Green GE, Zopf DA (2017) Computer-aided design and 3-dimensional printing for costal cartilage simulation of airway graft carving. Otolaryngol Head Neck Surg 156:1044–1047. https://doi.org/10.1177/0194599817697048
Chang DR, Lin RP, Bowe S, Bunegin L, Weitzel EK, McMains KC, Willson T, Chen PG (2017) Fabrication and validation of a low-cost, medium-fidelity silicone injection molded endoscopic sinus surgery simulation model. Laryngoscope 127:781–786. https://doi.org/10.1002/lary.26370
AlReefi MA, Nguyen LH, Mongeau LG, Haq BU, Boyanapalli S, Hafeez N, Cegarra-Escolano F, Tewfik MA (2017) Development and validation of a septoplasty training model using 3-dimensional printing technology. Int Forum Allergy Rhinol 7:399–404. https://doi.org/10.1002/alr.21887
Kavanagh KR, Cote V, Tsui Y, Kudernatsch S, Peterson DR, Valdez TA (2017) Pediatric laryngeal simulator using 3D printed models: a novel technique. Laryngoscope 127:E132–E137. https://doi.org/10.1002/lary.26326
Barber SR, Kozin ED, Dedmon M, Lin BM, Lee K, Sinha S, Black N, Remenschneider AK, Lee DJ (2016) 3D-printed pediatric endoscopic ear surgery simulator for surgical training. Int J Pediatr Otorhinolaryngol 90:113–118. https://doi.org/10.1016/j.ijporl.2016.08.027
Mowry SE, Jammal H, Myer C 4th, Solares CA, Weinberger P (2015) A novel temporal bone simulation model using 3D printing techniques. Otol Neurotol 36:1562–1565. https://doi.org/10.1097/MAO.0000000000000848
Hochman JB, Rhodes C, Wong D, Kraut J, Pisa J, Unger B (2015) Comparison of cadaveric and isomorphic three-dimensional printed models in temporal bone education. Laryngoscope 125:2353–2357. https://doi.org/10.1002/lary.24919
Da Cruz MJ, Francis HW (2015) Face and content validation of a novel three-dimensional printed temporal bone for surgical skills development. J Laryngol Otol 129(Suppl 3):S23–S29. https://doi.org/10.1017/S0022215115001346
Rose AS, Kimbell JS, Webster CE, Harrysson OL, Formeister EJ, Buchman CA (2015) Multi-material 3D models for temporal bone surgical simulation. Ann Otol Rhinol Laryngol 124:528–536. https://doi.org/10.1177/0003489415570937
Mick PT, Arnoldner C, Mainprize JG, Symons SP, Chen JM (2013) Face validity study of an artificial temporal bone for simulation surgery. Otol Neurotol 34:1305–1310. https://doi.org/10.1097/MAO.0b013e3182937af6
Monfared A, Mitteramskogler G, Gruber S, Salisbury JK Jr, Stampfl J, Blevins NH (2012) High-fidelity, inexpensive surgical middle ear simulator. Otol Neurotol 33:1573–1577. https://doi.org/10.1097/MAO.0b013e31826dbca5
Canzi P, Capaccio P, Marconi S, Conte G, Preda L, Avato I, Aprile F, Gaffuri M, Occhini A, Pignataro L, Auricchio F, Benazzo M (2020) Feasibility of 3D printed salivary duct models for sialendoscopic skills training: preliminary report [preliminary report]. Eur Arch Otorhinolaryngol 277:909–915. https://doi.org/10.1007/s00405-019-05763-4
Muto J, Carrau RL, Oyama K, Otto BA, Prevedello DM (2017) Training model for control of an internal carotid artery injury during transsphenoidal surgery. Laryngoscope 127:38–43. https://doi.org/10.1002/lary.26181
Bone TM, Mowry SE (2016) Content validity of temporal bone models printed via inexpensive methods and materials. Otol Neurotol 37:1183–1188. https://doi.org/10.1097/MAO.0000000000001131
Ding CY, Yi XH, Jiang CZ, Xu H, Yan XR, Zhang YL, Kang DZ, Lin ZY (2019) Development and validation of a multi-color model using 3-dimensional printing technology for endoscopic endonasal surgical training. Am J Transl Res 11:1040–1048
Narayanan V, Narayanan P, Rajagopalan R, Karuppiah R, Rahman ZA, Wormald PJ, Van Hasselt CA, Waran V (2015) Endoscopic skull base training using 3D printed models with pre-existing pathology. Eur Arch Otorhinolaryngol 272:753–757. https://doi.org/10.1007/s00405-014-3300-3
Barber SR, Kozin ED, Naunheim MR, Sethi R, Remenschneider AK, Deschler DG (2018) 3D-printed tracheoesophageal puncture and prosthesis placement simulator. Am J Otolaryngol 39:37–40. https://doi.org/10.1016/j.amjoto.2017.08.001
Ainsworth TA, Kobler JB, Loan GJ, Burns JA (2014) Simulation model for transcervical laryngeal injection providing real-time feedback. Ann Otol Rhinol Laryngol 123:881–886. https://doi.org/10.1177/0003489414539922
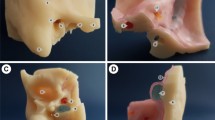
Bento RF, Rocha BA, Freitas EL, Balsalobre FA (2019) Otobone ®: three-dimensional printed temporal bone biomodel for simulation of surgical procedures. Int Arch Otorhinolaryngol 23:e451–e454. https://doi.org/10.1055/s-0039-1688924
Vimawala S, Gao T, Goldfarb J, Gadaleta D, Ku B, Jean-Gilles P, Luginbuhl A, Pugliese R, Weed D, Curry JM (2020) Initial experience using 3-dimensional printed models for head and neck reconstruction in Haiti. Ear Nose Throat J 32:145561320938920. https://doi.org/10.1177/0145561320938920
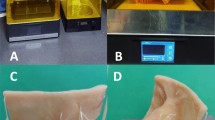
Ferreira E, Silva L, Chisté Ferreira M, Couceiro Seto II, Martins Umbelino A, Aguiar Gomes VC, de Borborema GL, Almeida Amaro LJ (2021) A three-dimensional printed myringotomy, tympanostomy and ventilation tube placement simulator. J Laryngol Otol 135:420–425. https://doi.org/10.1017/S0022215121001146
Chae R, Sharon JD, Kournoutas I, Ovunc SS, Wang M, Abla AA, El-Sayed IH, Rubio RR (2020) Replicating skull base anatomy with 3D technologies: a comparative study using 3D-scanned and 3D-printed models of the temporal bone. Otol Neurotol 41:e392–e403. https://doi.org/10.1097/MAO.0000000000002524
Thiong’o GM, Bernstein M, Drake JM (2021) 3D printing in neurosurgery education: a review. 3D Print Med. https://doi.org/10.1186/s41205-021-00099-4
Meara JG, Greenberg SLM (2015) The Lancet Commission on global surgery global surgery 2030: evidence and solutions for achieving health, welfare and economic development. Surgery 157:834–835. https://doi.org/10.1016/j.surg.2015.02.009
McMillan A, Kocharyan A, Dekker SE, Kikano EG, Garg A, Huang VW, Moon N, Cooke M, Mowry SE (2020) Comparison of materials used for 3D-printing temporal bone models to simulate surgical dissection. Ann Otol Rhinol Laryngol 129:1168–1173. https://doi.org/10.1177/0003489420918273
Funding
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Contributions
RFB and MAdS conceived the idea for this article. MAdS and DdMPR collected relevant data. LF and RFB analyzed the data after discussions with MAdS. MAdS, DdMPR, and PTL drafted the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Souza, M.A., Bento, R.F., Lopes, P.T. et al. Three-dimensional printing in otolaryngology education: a systematic review. Eur Arch Otorhinolaryngol 279, 1709–1719 (2022). https://doi.org/10.1007/s00405-021-07088-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07088-7