Abstract
Purpose
Previous studies on fungus balls have primarily focused on immunocompetent patients, and only a few studies have described the clinical characteristics of fungus balls in malignant hematological disease (MHD) patients. Therefore, we compared the clinical features of maxillary sinus fungus ball (MSFB) between immunosuppressive patients with MHD and immunocompetent patients.
Methods
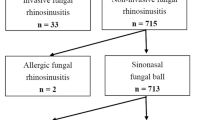
Twenty patients with MHD and 40 randomly selected immunocompetent patients were enrolled and divided into MHD and non-MHD groups. All patients were diagnosed with MSFB and their clinical features were retrospectively analyzed.
Results
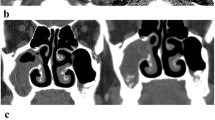
Patients in the MHD group had non-specific clinical symptoms and endoscopic manifestations of MSFB, similar to those in the non-MHD group. On computed tomography (CT), the MHD group showed higher Lund-Mackay scores, lesser single sinus opacifications, more multiple sinus opacifications on the affected side, and more bilateral opacifications compared to the non-MHD group. The MHD group had a lower frequency of central hyper-density and heterogeneous opacifications than the non-MHD group. There were no significant differences between the two groups in terms of the fungal-infected side, lateral sinus wall ratio, sclerosis of the lateral sinus wall, erosion of the inner sinus wall, and nasal septum deviation.
Conclusion
The clinical symptoms and endoscopic manifestations of MSFB in patients with MHD were similar to those of immunocompetent patients. However, more atypical signs and wider mucosal inflammation were found on CT scans of MSFB patients with MHD. These results indicate that caution should be executed when excluding the possibility of fungus balls in immunosuppressive patients.

Similar content being viewed by others
Availability of data and material
The datasets used and analyzed during the current study are available on reasonable request.
Code availability
Not applicable.
References
Lee JS, Shin SY, Lee KH, Kim SW, Cho JS (2013) Change of prevalence and clinical aspects of fungal ball according to temporal difference. Eur Arch Otorhinolaryngol 270:1673–1677. https://doi.org/10.1007/s00405-012-2234-x
Liu X, Liu C, Wei H, He S, Dong S, Zhou B et al (2020) A retrospective analysis of 1,717 paranasal sinus fungus ball cases from 2008 to 2017. Laryngoscope 130:75–79. https://doi.org/10.1002/lary.27869
Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina W, Kita H et al (2009) Fungal rhinosinusitis: a categorization and definitional schema addressing current controversies. Laryngoscope 119:1809–1818. https://doi.org/10.1002/lary.20520
Cha H, Song Y, Bae YJ, Won TB, Kim JW, Cho SW, Rhee CS (2020) Clinical characteristics other than intralesional hyperdensity may increase the preoperative diagnostic accuracy of maxillary sinus fungal ball. Clin Exp Otorhinolaryngol 13:157–163. https://doi.org/10.21053/ceo.2019.00836
Dufour X, Kauffmann-Lacroix C, Ferrie JC, Goujon JM, Rodier MH, Klossek JM (2006) Paranasal sinus fungus ball: epidemiology, clinical features and diagnosis. A retrospective analysis of 173 cases from a single medical center in France, 1989–2002. Med Mycol 44:61–67. https://doi.org/10.1080/13693780500235728
Robey AB, O’Brien EK, Richardson BE, Baker JJ, Poage DP, Leopold DA (2009) The changing face of paranasal sinus fungus balls. Ann Otol Rhinol Laryngol 118:500–505. https://doi.org/10.1177/000348940911800708
Grosjean P, Weber R (2007) Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol 264:461–470. https://doi.org/10.1007/s00405-007-0281-5
Azoulay E, Russell L, Van de Louw A, Metaxa V, Bauer P, Povoa P et al (2020) Diagnosis of severe respiratory infections in immunocompromised patients. Intensive Care Med 46:298–314. https://doi.org/10.1007/s00134-019-05906-5
Deutsch PG, Whittaker J, Prasad S (2019) Invasive and non-invasive fungal rhinosinusitis—a review and update of the evidence. Medicina (Kaunas). https://doi.org/10.3390/medicina55070319
Seo MY, Seok H, Lee SH, Choi JE, Hong SD, Chung SK et al (2020) Microinvasive fungal rhinosinusitis: proposal of a new subtype in the classification. J Clin Med. https://doi.org/10.3390/jcm9020600
Ferguson BJ (2000) Fungus balls of the paranasal sinuses. Otolaryngol Clin North Am 33:389–398. https://doi.org/10.1016/s0030-6665(00)80013-4
Gungor A, Adusumilli V, Corey JP (1998) Fungal sinusitis: progression of disease in immunosuppression–a case report. Ear Nose Throat J 77(207–210):215
Kim YK, Kim HJ, Kim HY, Cha J, Lee JY, Chung SK et al (2016) Extrasinonasal infiltrative process associated with a sinonasal fungus ball: does it mean invasive fungal sinusitis? Diagn Interv Radiol 22:347–353. https://doi.org/10.5152/dir.2015.15417
Soler ZM, Schlosser RJ (2012) The role of fungi in diseases of the nose and sinuses. Am J Rhinol Allergy 26:351–358. https://doi.org/10.2500/ajra.2012.26.3807
Orlowski H, McWilliams S, Mellnick VM, Bhalla S, Lubner MG, Pickhardt PJ et al (2017) Imaging spectrum of invasive fungal and fungal-like infections. Radiographics 37:1119–1134. https://doi.org/10.1148/rg.2017160110
Arulrajah S, Symons H, Cahoon EK, Tekes A, Huisman TA, Izbudak I (2012) Relationship between clinical sinusitis symptoms and sinus CT severity in pediatric post bone marrow transplant and immunocompetent patients. Eur J Pediatr 171:375–381. https://doi.org/10.1007/s00431-011-1560-0
Ho CF, Lee TJ, Wu PW, Huang CC, Chang PH, Huang YL et al (2019) Diagnosis of a maxillary sinus fungus ball without intralesional hyperdensity on computed tomography. Laryngoscope 129:1041–1045. https://doi.org/10.1002/lary.27670
DeShazo RD, O’Brien M, Chapin K, Soto-Aguilar M, Gardner L, Swain R (1997) A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg 123:1181–1188. https://doi.org/10.1001/archotol.1997.01900110031005
Seo MY, Lee SH, Ryu G, Hong SD, Kim HY, Dhong HJ et al (2019) Clinical pattern of fungal balls in the paranasal sinuses: our experience with 70 patients. Eur Arch Otorhinolaryngol 276:1035–1038. https://doi.org/10.1007/s00405-018-5258-z
Callejas CA, Douglas RG (2013) Fungal rhinosinusitis: what every allergist should know. Clin Exp Allergy 43:835–849. https://doi.org/10.1111/cea.12118
Klossek JM, Serrano E, Peloquin L, Percodani J, Fontanel JP, Pessey JJ (1997) Functional endoscopic sinus surgery and 109 mycetomas of paranasal sinuses. Laryngoscope 107:112–117. https://doi.org/10.1097/00005537-199701000-00021
Ortiz E, Nakamura E, Magalhaes R, Souza CA, Chone CT, Vigorito AC et al (2010) Prognostic value of sinus CT scans in hematopoietic stem cell transplantation. Braz J Otorhinolaryngol 76:618–622
Pagella F, Matti E, De Bernardi F, Semino L, Cavanna C, Marone P et al (2007) Paranasal sinus fungus ball: diagnosis and management. Mycoses 50:451–456. https://doi.org/10.1111/j.1439-0507.2007.01416.x
Chen JC, Ho CY (2012) The significance of computed tomographic findings in the diagnosis of fungus ball in the paranasal sinuses. Am J Rhinol Allergy 26:117–119. https://doi.org/10.2500/ajra.2012.26.3707
Yoon YH, Xu J, Park SK, Heo JH, Kim YM, Rha KS (2017) A retrospective analysis of 538 sinonasal fungus ball cases treated at a single tertiary medical center in Korea (1996–2015). Int Forum Allergy Rhinol 7:1070–1075. https://doi.org/10.1002/alr.22007
Stammberger H, Jakse R, Beaufort F (1984) Aspergillosis of the paranasal sinuses x-ray diagnosis, histopathology, and clinical aspects. Ann Otol Rhinol Laryngol 93:251–256. https://doi.org/10.1177/000348948409300313
Nicolai P, Mensi M, Marsili F, Piccioni M, Salgarello S, Gilberti E et al (2015) Maxillary fungus ball: zinc-oxide endodontic materials as a risk factor. Acta Otorhinolaryngol Ital 35:93–96
Kim SC, Ryoo I, Shin JM, Suh S, Jung HN, Shin SU (2020) MR Findings of fungus ball: significance of high signal intensity on T1-weighted images. J Korean Med Sci 35:e22. https://doi.org/10.3346/jkms.2020.35.e22
Seo YJ, Kim J, Kim K, Lee JG, Kim CH, Yoon JH (2011) Radiologic characteristics of sinonasal fungus ball: an analysis of 119 cases. Acta Radiol 52:790–795. https://doi.org/10.1258/ar.2011.110021
Eggesbo HB (2006) Radiological imaging of inflammatory lesions in the nasal cavity and paranasal sinuses. Eur Radiol 16:872–888. https://doi.org/10.1007/s00330-005-0068-2
McCarty JL, David RM, Lensing SY, Samant RS, Kumar M, Van Hemert RL et al (2017) Root cause analysis: an examination of odontogenic origins of acute maxillary sinusitis in both immunocompetent & immunocompromised patients. J Comput Assist Tomogr 41:484–488. https://doi.org/10.1097/RCT.0000000000000522
Lamoth F, Calandra T (2017) Early diagnosis of invasive mould infections and disease. J Antimicrob Chemother 72:i19–i28. https://doi.org/10.1093/jac/dkx030
Wickes BL, Wiederhold NP (2018) Molecular diagnostics in medical mycology. Nat Commun 9:5135. https://doi.org/10.1038/s41467-018-07556-5
Tarkan O, Karagun B, Ozdemir S, Tuncer U, Surmelioglu O, Cekic E et al (2012) Endonasal treatment of acute invasive fungal rhinosinusitis in immunocompromised pediatric hematology-oncology patients. Int J Pediatr Otorhinolaryngol 76:1458–1464. https://doi.org/10.1016/j.ijporl.2012.06.021
Funding
This work supported by Natural Science Foundation of Beijing Municipality (Grant Number: 7202215). The funding organization did not contribute to the design or conduct of this study; preparation, review, approval, or decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yang Yang, Zhimin Xing, Lisheng Yu, Xiaopei Yuan, Min Wang, Congli Geng, Yan Liu, Shichang Li and Yuanjun Liu. The first draft of the manuscript was written by Yang Yang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, Y., Xing, Z., Yu, L. et al. Clinical features in maxillary sinus fungus ball in patients with malignant hematological disease. Eur Arch Otorhinolaryngol 279, 1919–1927 (2022). https://doi.org/10.1007/s00405-021-06973-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06973-5