Abstract
Purpose
To analyze and compare surgical and audiological outcomes of conventional approaches versus laser CO2 surgery in stapes surgery.
Methods
333 patients who underwent stapes surgery were enrolled in the study; the patient population was divided into three groups: group 1: 170 patients treated with conventional stapedotomy with manual microdrill (average age 49.13 years); group 2: 119 patients treated with conventional stapedotomy with electrical microdrill (average age 51.06 years); group 3: 44 patients (average age 50.4 years) who underwent CO2 laser stapedotomy. Intra-operative, postoperative outcomes and audiological results were investigated.
Results
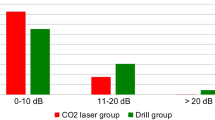
The average surgical time of laser CO2 surgery was longer than for other surgical procedures. No statistical differences emerged in post-operative abnormal taste sensation. There was also no difference in postoperative dizziness. Air-bone gap (ABG) went down from 29.7 ± 10 dB (group 1) and 27.32 ± 9.20 (group 2) to 10 ± 6.9 dB (group 1) and 10.7 ± 6.03 dB (group 2). In group 3 the preoperative ABG was lowered from 28.3 ± 10.1 to 11.8 ± 10.9, with a statistical difference in auditory recovery (p = 0.0001); The group of patients treated with laser CO2 showed a percentage of patients with an ABG closure of between 0 and 10 dB higher than in the group treated with manual microdrills (77.2% vs. 60%, respectively; p = 0.03).
Conclusion
Overall surgical results of CO2 laser and conventional stapedotomy are comparable without any significant difference; however, the group treated with CO2 laser appears to have a percentage of patients with an ABG closure 0–10 dB higher than the group treated using the conventional technique.
Similar content being viewed by others
References
Eshraghi AA, Telischi FF (2018) Otosclerosis and stapes surgery. Otolaryngol Clin North Am 51(2):xvii–ix
Nazarian R, McElveen JT Jr, Eshraghi AA (2018) History of otosclerosis and stapes surgery. Otolaryngol Clin North Am 51:275–290
Iannella G, Angeletti D, Manno A, Pasquariello B, Re M, Magliulo G (2018) Malleostapedotomy in stapes revision surgery: is an endoscopic approach possible? Laryngoscope 128:2611–2614
Sevy A, Arriaga M (2018) The stapes prosthesis: past, present, and future. Otolaryngol Clin North Am 51:393–404
Yeh CF, Wang MC, Chu CH, Shiao AS (2019) Predictors of hearing outcomes after stapes surgery in otosclerosis. Acta Otolaryngol 139:1058–1062
Young E, Mitchell-Innes A, Jindal M (2015) Lasers in stapes surgery: a review. J Laryngol Otol 129:627–633
Iannella G, Magliulo G (2016) Endoscopic versus microscopic approach in stapes surgery: are operative times and learning curve important for making the choice? Otol Neurotol 37:1350–1357
Pauli N, Strömbäck K, Lundman L, Dahlin-Redfors Y (2020) Surgical technique in stapedotomy hearing outcome and complications. Laryngoscope 130:790–796
Iannella G, Marcotullio D, Re M, Manno A et al (2017) Endoscopic vs. microscopic approach in stapes surgery: advantages in the middle ear structures visualization and trainees point of view. J Int Adv Otol 13:14–20
Lancer H, Manickavasagam J, Zaman A, Lancer J (2016) Stapes surgery: a national survey of British otologists. Eur Arch Otorhinolaryngol 273:371–379
Boyev KP (2018) Use of lasers in otosclerosis surgery. Otolaryngol Clin North Am 51:405–413
Bartel R, Huguet G, Cruellas F, Hamdan M, Gonzalez-Compta X, Cisa E (2021) Laser vs drill for footplate fenestration during stapedotomy: a systematic review and meta-analysis of hearing results. Eur Arch Otorhinolaryngol 278:9–14
Forton GE, Wuyts FL, Delsupehe KG, Verfaillie J, Loncke R (2009) CO2 laser-assisted stapedotomy combined with a Wengen titanium clip stapes prosthesis: superior short-term results. Otol Neurotol 30:1071–1078
Du LJ, Gao HG, Tong J, Chen WW, Shan L, Cai XH (2017) Comparative analysis of laser and non-laser stapes surgeries. J Int Adv Otol 13:32–35
Altamami NM, Huyghues G, Fieux M et al (2019) Is one of these two techniques: CO2laser versus microdrill assisted stapedotomy results in better post-operative hearing outcome? Eur Arch Otorhinolaryngol 276:1907–1913
Monsell E, Balkany T, Gates G, Goldenberg RA, Meyerhoff WL, House JW (1995) Committee on hearing and equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg 113:186–187
Watson GJ, da Cruz M (2018) Reporting in stapes surgery: are we following the guidelines? J Laryngol Otol 132:479–485
Srivastava R, Cho W, Fergie N (2021) The use of lasers in stapes surgery. Ear Nose Throat J 100:73–76
Kuo CW, Wu HM (2018) Fully endoscopic laser stapedotomy: is it comparable with microscopic surgery? Acta Otolaryngol 138:871–876
Schönfeld U, Weiming H, Hofmann VM, Jovanovic S, Albers AE (2017) CO2laser stapedotomy safety: influence of laser energy and time on bone-conduction hearing levels. Eur Arch Otorhinolaryngol 274:4131–4139
Ryan S, Thornton MA, Kieran S, Charles D (2009) A comparison of CO2 laser versus traditional stapedectomy outcomes. Ir Med J 102:218–220
Brase C, Keil I, Schwitulla J et al (2013) Bone conduction after stapes surgery: comparison of CO2 laser and manual perforation. Otol Neurotol 34:821–826
Perkins RC (1980) Laser stepedotomy for otosclerosis. Laryngoscope 90:228–240
Fang L, Lin H, Zhang TY, Tan J (2014) Laser versus non-laser stapedotomy in otosclerosis: a systematic review and meta-analysis. Auris Nasus Larynx 4:337–342
Wegner I, Swartz JE, Bance ML, Grolman W (2016) A systematic review of the effect of different crimping techniques in stapes surgery for otosclerosis. Laryngoscope 126:1207–1217
Cuda D, Murri A, Mochi P, Solenghi T, Tinelli N (2009) Microdrill, CO2-laser, and piezoelectric stapedotomy: a comparative study. Otol Neurotol 30:1111–1115
Kaul VF, Chow K, Estrera SL, Schwam ZG, Wanna GB (2020) Microdrill in endoscopic stapes surgery: is it safe? Am J Otolaryngol 41:102666
Iannella G, De Vincentiis M, Greco A et al (2019) Endoscopic approach in second stage ossicular chain reconstruction. Am J Otolaryngol 40:735–742
Watson GJ, Byth K, da Cruz M (2015) Outcomes in stapedotomy surgery: the learning curve redefined. Otol Neurotol 36(10):1601–1603
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Vito, A., Mandalà, M., Soprani, F. et al. Conventional approaches versus laser CO2 surgery in stapes surgery: a multicentre retrospective study. Eur Arch Otorhinolaryngol 279, 2321–2327 (2022). https://doi.org/10.1007/s00405-021-06926-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06926-y