Abstract
Objective
This study aimed to analyze the role of the endoscope in revision canal-wall down (CWD) tympanomastoid surgery and compare its use to the more traditional microscopic approach. Moreover, we aim to investigate functional outcomes of revision surgeries in a cohort of two tertiary reference centers.
Methods
A total of 103 patients undergoing revision surgery after previous CWD tympanomastoidectomy were included in the present study and divided in three groups according to the surgical technique used: endoscope exclusive (n = 22), combined (n = 35) and microscope exclusive (n = 46). Data regarding surgical indications, pre-operative clinical and audiological assessments, intraoperative findings and surgical considerations were extracted. During follow-up, data regarding anatomic and audiologic outcomes were collected and persistence or recurrence of the disease assessed.
Results
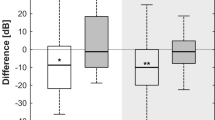
The most frequent sites of cholesteatoma recurrence or persistence was the anterior epitympanum. There was a statistically significant ABG improvement of − 6.02 dB HL (95% CI − 8.87 to − 3.16, p < 0.001) between pre-operative and postoperative ABG, without significant effect of surgical technique. During follow-up, no significant differences regarding disease or otorrhea control were observed. Duration of surgery and hospitalization was shorter in the endoscopic cohort without statistical significance. Intra- and postoperative complications were lower in the endoscopic group.
Conclusion
Revision CWD surgery can take advantage of the endoscope as a minimally invasive exclusive or adjunct tool to traditional microscopic procedures. Outcome measures of endoscopic revision CWD surgery showed anatomic and functional results comparable to those of the microscopic group. The complication rate, the duration of surgery and hospitalization were favorable in the endoscopic group.



Similar content being viewed by others
Availability of data and material
All relevant data and the final dataset are available upon motivated request to the corresponding author.
References
Kasenõmm P (2013) Intraoperative findings of revision canal wall-down tympanomastoid surgery. ActaOtolaryngol 133(8):826–832. https://doi.org/10.3109/00016489.2013.787645
Kerckhoffs KGP, Kommer MBJ, van Strien THL et al (2016) The disease recurrence rate after the canal wall up or canal wall down technique in adults: a review on cholesteatoma recidivism after CWU and CWD. Laryngoscope 126(4):980–987. https://doi.org/10.1002/lary.25591
Walker PC, Mowry SE, Hansen MR, Gantz BJ (2014) Long-term results of canal wall reconstruction tympanomastoidectomy. OtolNeurotol 35(6):954–960. https://doi.org/10.1097/MAO.0b013e3182a446da
Lucidi D, De Corso E, Paludetti G, Sergi B (2019) Quality of life and functional results in canal wall down vs canal wall up mastoidectomy. ActaOtorhinolaryngol Ital 39(1):53–60. https://doi.org/10.14639/0392-100X-2005
Alicandri-Ciufelli M, Fermi M, Bonali M et al (2018) Facial sinus endoscopic evaluation, radiologic assessment, and classification: facial sinus endoscopic study. Laryngoscope 128(10):2397–2402. https://doi.org/10.1002/lary.27135
Anschuetz L, Alicandri-Ciufelli M, Bonali M et al (2018) Novel surgical and radiologic classification of the subtympanic sinus: implications for endoscopic ear surgery. Otolaryngol-Head Neck Surg 159(6):1037–1042. https://doi.org/10.1177/0194599818787180
Cohen MS, Basonbul RA, Barber SR, Kozin ED, Rivas AC, Lee DJ (2018) Development and validation of an endoscopic ear surgery classification system: endoscopic ear surgery classification system. Laryngoscope 128(4):967–970. https://doi.org/10.1002/lary.26802
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences. 2nd ed. L. Erlbaum Associates
Košec A, Kelava I, Ajduk J, Ries M, Trotić R, Bedeković V (2017) Significance of intraoperative findings in revision tympanomastoidectomy. Am J Otolaryngol 38(4):462–465. https://doi.org/10.1016/j.amjoto.2017.04.006
Pareschi R, Lepera D, Nucci R (2019) Canal wall down approach for tympano-mastoid cholesteatoma: long-term results and prognostic factors. ActaOtorhinolaryngol Ital 39(2):122–129. https://doi.org/10.14639/0392-100X-2237
Das S, Dutta M, Panja T, Sinha R (2019) Chronic draining ear and cholesteatoma recidivism: a retrospection from clinical, imaging, and surgical perspectives. Turk Arch Otorhinolaryngol 57(3):133–139. https://doi.org/10.5152/tao.2019.4266
Yung M, Tono T, Olszewska E et al (2017) EAONO/JOS joint consensus statements on the definitions, classification and staging of middle ear cholesteatoma. J IntAdvOtol 13(1):1–8. https://doi.org/10.5152/iao.2017.3363
van der Toom H, van der Schroeff M, Janssen J, Westzaan A, Pauw R (2020) A retrospective analysis and comparison of the STAM and STAMCO Classification and EAONO/JOS cholesteatoma staging system in predicting surgical treatment outcomes of middle ear cholesteatoma. OtolNeurotol 41(4):e468–e474. https://doi.org/10.1097/MAO.0000000000002549
Bonali M, Fermi M, Alicandri-Ciufelli M et al (2020) Correlation of radiologic versus endoscopic visualization of the middle ear: implications for endoscopic ear surgery. OtolNeurotol 41(9):e1122–e1127. https://doi.org/10.1097/MAO.0000000000002787
Anschuetz L, Bonali M, Guarino P, et al (2018) Management of bleeding in exclusive endoscopic ear surgery: pilot clinical experience. Otolaryngol-Head Neck Surg. Published online September 5, 2017:019459981772698. https://doi.org/10.1177/0194599817726982
Ferri G, Fermi M, Alicandri-Ciufelli M, Villari D, Presutti L (2019) Management of jugular bulb injuries during endoscopic ear surgery: our experience. J Neurol Surg Part B Skull Base. Published online January 21, 2019. https://doi.org/10.1055/s-0039-1677679
Marchioni D, Rubini A, Gazzini L et al (2018) Complications in endoscopic ear surgery. OtolNeurotol 39(8):1012–1017. https://doi.org/10.1097/MAO.0000000000001933
Chiao W, Chieffe D, Fina M (2021) Endoscopic management of primary acquired cholesteatoma. OtolaryngolClin North Am 54(1):129–145. https://doi.org/10.1016/j.otc.2020.09.014
Botti C, Fermi M, Amorosa L, et al (2019) Cochlear function after type-1 tympanoplasty: endoscopic versus microscopic approach, a comparative study. Eur Arch Oto-Rhino-Laryngol. Published online October 25, 2019. https://doi.org/10.1007/s00405-019-05706-z
Funding
No funding is reported for the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fermi, M., Siggemann, T., Melchiorri, C. et al. Revision canal-wall down surgery: comparison of surgical outcomes with three different techniques. Eur Arch Otorhinolaryngol 279, 1731–1739 (2022). https://doi.org/10.1007/s00405-021-06829-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06829-y