Abstract
Background
The histological and electron-microscopic (EM) characteristics of juvenile nasopharyngeal angiofibroma (JNA) have been described but no study has compared them with one another or with clinical features. The objective is to compare ultrastructural characteristics of JNA with clinical parameters.
Methods
This prospective study included histology of 21 samples of which only 13 underwent transmission-EM. Four clinical parameters (age, duration, epistaxis, recurrence), three radiological-staging, 13 histological and 15 EM characteristics were considered. A descriptive analysis for association of these characteristics and also with clinical parameters was attempted. Furthermore statistical analysis of clinical and radiological categories with respect to frequencies of ultrastructural characteristics was also undertaken.
Results
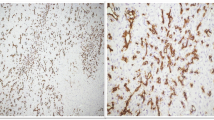
Dense-intranuclear-inclusions (DNI) and peripheral-nuclear-irregularities were universally encountered while other very prominent features were nuclear-blebs-and-pockets, myoid-features, thin-vessel-wall (TnVW), irregular-vascular-contour (IVC) and fibrous-stroma (FS). Statistical significance was obtained between recurrence with histology (p = 0.04) and Fisch staging with EM (p = 0.001). While muscle-in-vessel-wall, thick-vessel-wall, mast-cells, stellate-stromal-cells and cellular-stroma predominated in recurrent cases, the upfront disease showed predominance of scar-like-stroma, fusiform-stromal-cells, IVC, TnVW, FS, organised-collagen-bundles and less-cellular-stroma. A very unique Rod-like-structures were appreciated in the cytoplasm of the fibroblast for the first time.
Conclusions
While histological parameters of recurrence need further validation, a larger sample may better define histopathological surrogate for predicting intracellular dynamics that may further correlate with underlying cellular stresses. Hence an ‘ultrastructural staging’ may better customise treatment protocol and prognosis. Furthermore ‘characteristic’ unique rods need to be further investigated along with validation of viral aetiology for DNI.






Similar content being viewed by others
References:
Svoboda DJ, Kirchner F (1966) Ultrastructure of nasopharyngeal angiofibromas. Cancer 19(12):1949–1962
McGavran MH, Sessions DG, Dorfman RF, Davis DO, Ogura JH (1969) Nasopharyngeal angiofibroma. Arch Otolaryngol 90(1):68–78
Walike JW, Mackay B (1970) Nasopharyngeal angiofibroma: light and electron microscopic changes after stilbesterol therapy. Laryngoscope 80(7):1109–1121
Taxy JB (1977) Juvenile nasopharyngeal angiofibroma. An ultrastructural study. Cancer 39(3):1044–1054
Fisch U (1983) The infratemporal fossa approach for nasopharyngeal tumors. Laryngoscope 93(1):36–44
Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT (1996) Angiofibroma: changes in staging and treatment. Arch Otolaryngol Head Neck Surg 122(2):122–129
Mishra SC, Shukla GK, Bhatia N, Pant MC (1989) A rational classification of angiofibromas of the post nasal space. J Laryngol Otol 103(10):912–916
Queisser Q, Wiegert S, Bading H (2011) Structural dynamics of the cell nucleus: basis for morphology modulation of nuclear calcium signalling and gene transcription. Nucleus 2(2):98–104
Kuttner K, Katenkamp D, Stiller D (1977) Hormontherapiebedingte Besonderheiten an der Ultrastruktur des juvenilen Nasenrachenfibroms. Arch Oto Rhino Laryngol 214:331–338
Topilko A, Zakrzewski A, Pichard E, Viron A (1984) Ultrastructural cytochemistry of intranuclear dense granules in nasopharyngeal angiofibroma. Ultrastruct Pathol 6(2–3):221–228. https://doi.org/10.3109/01913128409018576
Bouteille M, Kalifat SR, Delarue J (1967) Ultrastructural variations of nuclear bodies in human diseases. J Ultrastruct Res 19(5–6):474–486
Robertson DM, MacLean JD (1965) Nuclear inclusions in malignant gliomas. Arch Neurol 13(3):287–296
Henry K, Petts V (1969) Nuclear bodies in human thymus. J Ultrastruct Res 27(3–4):330–343
Krishan A, Uzman BG, Hedley-Whyte ET (1967) Nuclear bodies: a component of cell nuclei in hamster tissues and human tumors. J Ultrastruct Res 19(5–6):563–572
Horstmann E, Richter R, Roosen-Runge E (1966) Zur Elektronenmikroskopie der Kerneinschlüsse im menschlichen Nebenhodenepithel. Z Zellforsch Mikrosk Anat 69(1):69–79
Arnold W (1976) Etiological aspects regarding the development of laryngeal papillomas (author’s transl). Laryngol Rhinol Otol 55(2):102–111
Arnold W, Ganzer U, Nasemann T (1977) Zur Pathogenese und Klinik der papillomatösen Haut-und Schleimhauterkrankungen. Arch Otorhinolaryngol 214(3):221–239
Dalton AJ, Haguenau F (Eds) (1973) Howatson A. Papovaviruses. In: Ultrastructure of animal viruses and bacteriophages: an atlas
Arnold W, Huth F (1978) Electron microscopic findings in four cases of nasopharyngeal fibroma. Virchows Archiv A 379(4):285–298
Mishra A, Sachadeva M, Jain A, Shukla NM, Pandey A (2016) Human papilloma virus in juvenile nasopharyngeal angiofibroma: possible recent trend. Am J Otolaryngol 37(4):317–322
Baumann O, Walz B (2001) Endoplasmic reticulum of animal cells and its organization into structural and functional domains. Int Rev Cytol 205:149–214
Alberts B, Johnson A, Lewis J, Raff M, Roberts K, Walter P (2002) Membrane-bound ribosomes define the rough ER. In molecular biology of the cell; 4th edition. Garland science. Retrieved 09 Dec 2008. https://www.ncbi.nlm.nih.gov/books/NBK26841/#2204
Pandey P, Mishra A, Tripathi A, Verma V, Trivedi R, Singh HP, Kumar S, Patel B, Singh V, Pandey S, Pandey A (2017) Mishra SC current molecular profile of juvenile nasopharyngeal angiofibroma: first comprehensive study from India. Laryngoscope 127(3):e100–e106
Westrate LM, Lee JE, Prinz WA, Voeltz GK (2015) Form follows function: the importance of endoplasmic reticulum shape. Annu Rev Biochem 84:791–811
Crocker DJ, Murad TM (1969) Ultrastructure of fibrosarcoma in a male breast. Cancer 23(4):891–899
Gabbiani G, Majno G (1972) Dupuytren’s contracture: fibroblast contraction? An ultrastructural study. Am J Pathol 66(1):131–146
Murray M, Schrodt GR, Berg HF (1966) Role of smooth muscle cells in healing of injured arteries. Arch Pathol 82:138–146
Navas-Palacios JJ (1983) The fibromatoses an ultrastructual study of 31 cases. Path Res Pract 176:158–175
Beham A, Kainz J, Stammberger H, Auböck L, Beham-Schmid C (1997) Immunohistochemical and electron microscopical characterization of stromal cells in nasopharyngeal angiofibromas. Eur Arch Otorhinolaryngol 254(4):196–199
Sennes LU, Butugan O, Sanchez TG, Bernardi FDC, Saldiva PHN (2004) Tissue maturation during the growth of juvenile nasopharyngeal angiofibroma. Ann Otol Rhinol Laryngol 113(1):34–38
Maurice M, Milad M (1981) Pathogenesis of juvenile nasopharyngeal fibroma (A new concept). J Laryngol Otol 95:1121–1126
Sánchez-Romero C, Carlos R, Díaz Molina JB, Thompson LDR, Almeida OPD, Piña AR (2018) Nasopharyngeal angiofibroma: a clinical, histopathological and immunohistochemical study of 42 cases with emphasis on stromal features. Head Neck Pathol 12(1):52–61
Wendler O, Schäfer R, Schick B (2007) Mast cells and T-lymphocytes in juvenile angiofibromas. Eur Arch Otorhinolaryngol 264(7):769–775
Gebhardt T, Lorentz A, Detmer F, Trautwein C, Bektas H, Manns MP, BischoV SC (2005) Growth, phenotype, and function of human intestinal mast cells are tightly regulated by transforming growth factor 1. Gut 54:928–934
Kollur SM, Pattankar VL, ElHag IA (2004) Mast cells in testicular lesions. Ups J Med Sci 109:239–246
Shakoory B, Fitzgerald SM, Lee SA, Chi DS, Krishnaswamy G (2004) The role of human mast cell-derived cytokines in eosinophil biology. J Interferon Cytokine Res 24:271–281
Yu P, Fu YX (2006) Tumor-infiltrating T-lymphocytes: friends or foes? Lab Invest 86:231–245
Özdemir Ö (2006) Mast cell density, angiogenesis, and their significance in tumor development. Gynecol Oncol 100:628–629
Hallgren J, Pejler G (2006) Biology of mast cell tryptase. An infammatory mediator. FEBS 273:1871–1895
Dabbous MK, Walker R, Haney L, Carter LM, Nicolson GL, Wooley DE (1986) Mast cells and matrix degranulation at sites of tumor invasion in rat mammary adenocarcinomas. Br J Cancer 54:459–465
Ribatti D, Finato N, Crivellato E, Marzullo A, Mangieri D, Nico B, Vacca A, Beltrami CA (2005) Neovascularization and mast cells with tryptase activity increase simultaneously with pathologic progression in human endometrial cancer. Am J Obstet Gynecol 193:1961–1965
Acknowledgements
The authors acknowledge primarily Mr. Anil Majumdar the chief technician of the electron microscopy laboratory and Mr. Harshit Singh the lab engineer in charge of the electron microscopy setup for their valuable time and efforts. Furthermore, the authors also acknowledge Dr. V Verma, Dr. HP Singh, Dr. S Kumar, Dr. M Chandra and Dr. AB Singh for recruiting patients for surgery. Finally Dr. Girja Kant Shukla Professor of statistics at Indian Institute of Technology, Kanpur (Retd.) and Indian Institute of Management, Lucknow (Retd.) needs due acknowledgement for his statistical inputs.
A part of work is adapted from the Master’s Thesis project of Dr Hage Ampu under the chief supervision of Professor *Anupam Mishra.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None to be declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hage, A., Singhai, A., Mishra, A. et al. Electron microscopy of juvenile nasopharyngeal angiofibroma: clinical and histopathological correlates. Eur Arch Otorhinolaryngol 279, 233–247 (2022). https://doi.org/10.1007/s00405-021-06815-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06815-4