Abstract
Purpose
To present a large series ears with tympanic membrane perforations (TMP), to describe their characteristics, and to propose a new classification system based on the pathogenesis of TMP.
Methods
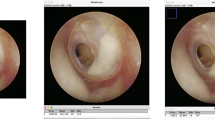
This cross-sectional study was conducted at a tertiary university hospital with 1003 ears (792 consecutive patients with TMP in at least 1 ear). Otoendoscopy and audiometry were performed. Perforation measurements and their locations were digitally assessed. TMP with no suggestive signs of previous retraction were classified as Group 1, and those with possible previous retraction were classified as Group 2. Signs of retraction previous to the TMP, symptom length, perforation size and location, status of the contralateral ear, and hearing status were compared.
Results
Group 1 comprised 63.5% of the included ears. Compared to Group 2, Group 1 presented a higher rate of central perforations (99% vs. 53%), a shorter duration of symptoms, smaller perforations (mean area: 18.5% vs. 41.4%), a higher rate of perforations in the anterior quadrants, better hearing levels (mean tritonal gap: 23.9 dB vs. 29.2 dB), and a lower rate of abnormal contralateral ears (28% vs. 66%).
Conclusion
The classification of TMP into two groups based on signs of previous retractions is feasible and indicates two different levels of disease severity. While the group without previous signs of retraction comprises ears with more limited disease, membranes with previous retraction seem to show more severe disease and, consequently, a less functional middle ear.



Similar content being viewed by others
Availability of data and materials
All the data of this study are available from the first author, who can be reached by email and at the address provided above. All the data are stored at the Hospital de Clínicas de Porto Alegre (Zona 19).
References
da Costa SS, de Dornelles C (2006) Otite Média Crônica não-colesteatomatosa. In: da Costa SS, Cruz OLM, de Oliveira JAA (eds) Otorrinolaringologia: Princípios e Prática, vol 10.4, 2nd edn. Artmed, Porto Alegre, pp 289–308
Bluestone CD, Kenna MA (1988) Introduction: definitions and goals of the workshop. Ann Otol Rhinol Laryngol. 97(2 supl):7
da Costa SS, de Dornelles C, Netto LFS, Braga MEL (2006) Aspectos Gerais das Otites Médias. In: da Costa SS, Cruz OLM, de Oliveira JAA (eds) Otorrinolaringologia: Princípios e Prática, vol 10.1, 2nd edn. Artmed, Porto Alegre, pp 254–273
Olszewska E, Wagner M, Bernal-Sprekelsen M et al (2004) Etiopathogenesis of cholesteatoma. Eur Arch Oto-Rhino-Laryngology 261(1):6–24. https://doi.org/10.1007/s00405-003-0623-x
Habermann J (1888) Zur Entstehung des Cholesteatoms des Mittelohres [in German]. Arch Ohrenheilkd 27:43–51
Bezold F (1890) Cholesteatom, Perforation der Membrana flaccida und Tubenverschluß [in German]. Z Hals Nasen Ohrenheilk 20:5–29
Rosito LPS, Sperling N, Teixeira AR et al (2018) The role of tympanic membrane retractions in cholesteatoma pathogenesis. Biomed Res Int. https://doi.org/10.1155/2018/9817123
Costa SS, Rosito LPS, da Silva MN, Selaimen FA (2019) Chronic otitis media without cholesteatoma. In: Paparella M, Costa SS, Fagan J (eds) Paparella’s otolaryngology head & neck surgery, vol 10. New Delhi, Jaypee, pp 116–135
Lerut B, Pfammatter A, Moons J, Linder T (2012) Functional correlations of tympanic membrane perforation size. Otol Neurotol 33(3):379–386. https://doi.org/10.1097/MAO.0b013e318245cea5
Comunello E, Von WA, Heck V, Dornelles C, Selamen S (2009) A computational method for the semi-automated quantitative analysis of tympanic membrane perforations and tympanosclerosis. Comput Biol Med 39(10):889–895. https://doi.org/10.1016/j.compbiomed.2009.07.002
Heck Junior V, Wangenheim AV, Abdala DD, Comunello E, Costa SS, Dornelles CC (2007) Computational techniques for accompaniment and measuring of otology pathologies. In: 20th symposium on IEEE computer society. pp 53–58. https://doi.org/10.1109/cbms.2007.34
Sadé J, Avraham S, Brown M (1981) Atelectasis. Retraction pockets and cholesteatoma. Acta Otolaryngol 92(5–6):501–512
Sudhoff H, Tos M (2007) Pathogenesis of sinus cholesteatoma. Eur Arch Oto-Rhino-Laryngol 264(10):1137–1143. https://doi.org/10.1007/s00405-007-0340-y
Yung M, Tono T, Olszewska E et al (2017) EAONO/JOS joint consensus statements on the definitions, classification and staging of middle ear cholesteatoma. J Int Adv Otol 13(1):1–8. https://doi.org/10.5152/iao.2017.3363
Ryan MA, Kaylie DM (2016) What is the optimal age to repair tympanic membrane perforations in pediatric patients? Laryngoscope 126(10):2201–2202. https://doi.org/10.1002/lary.26052
Ribeiro JC, Rui C, Natercia S, Jose R, Antonio P (2011) Tympanoplasty in children: a review of 91 cases. Auris Nasus Larynx 38(1):21–25. https://doi.org/10.1016/j.anl.2010.05.004
Hardman J, Muzaffar J, Nankivell P, Coulson C (2015) Tympanoplasty for chronic tympanic membrane perforation in children: systematic review and meta-analysis. Otol Neurotol 36(5):796–804
Celik O, Eskiizmir G, Ulkumen B, Karaca G (2018) Impact of graft type on anatomical and functional outcome in type-I tympanoplasty. B-ENT 15:169–177
Bhattacharya S, Pal S, Saha S, Gure P, Roy A (2016) Comparison of a microsliced modified chondroperichondrium shield graft and a temporalis fascia graft in primary type I tympanoplasty: a prospective randomized controlled trial. Ear Nose Throat J 95(7):274–283
Ciğer E, Balcı MK, İşlek A, Önal K (2018) The wheel-shaped composite cartilage graft (WsCCG) and temporalis fascia for type 1 tympanoplasty: a prospective, randomized study. Eur Arch Oto-Rhino-Laryngol 275(12):2975–2981. https://doi.org/10.1007/s00405-018-5171-5
Lyons SA, Su T, Vissers LET, Peters JPM, Smit AL, Grolman W (2016) Fascia compared to one-piece composite cartilage-perichondrium grafting for tympanoplasty. Laryngoscope 126(July):1662–1670. https://doi.org/10.1002/lary.25772
Tseng C, Lai M, Wu C, Yuan S, Ding Y (2017) Comparison of the efficacy of endoscopic tympanoplasty and microscopic tympanoplasty: a systematic review and meta-analysis. Laryngoscope 127(8):1890–1896. https://doi.org/10.1002/lary.26379
Jumaily M, Franco J, Gallogly J et al (2018) Butterfly cartilage tympanoplasty outcomes: a single-institution experience and literature review. Am J Otolarynogol 39(4):396–400. https://doi.org/10.1016/j.amjoto.2018.03.029
Abdelghany A (2013) The button graft technique for perforations affecting less than 25% of the tympanic membrane: a non-randomised comparison of a new modification to cartilage tympanoplasty with underlay and overlay grafts. Clin Otolaryngol Off J ENT-UK 38(3):208–216
Tong M, Yue V, Ku P, van Hasselt C (2002) Preoperative topical ofloxacin solution for tympanoplasty: a randomized, controlled study. Otol Neurotol 23(1):18–20
Onal K, Uguz M, Kazikdas K, Gursoy S, Gokce H (2005) A multivariate analysis of otological, surgical and patient-related factors in determining success in myringoplasty. Clin Otolaryngol Off J ENT-UK 30(2):115–120
Malafronte G, Filosa B (2018) One hundred twenty-five fat myringoplasties: does marginal perforation matter? Clin Otolaryngol Off J ENT-UK 43(1):362–365. https://doi.org/10.1111/coa.12976
da Costa SS (1999) Otites médias - aspectos gerais. In: Cruz OLM, da Costa SS (eds) Otologia Clínica e Cirúrgica, 1st edn. Revinter, Rio de Janeiro, pp 137–161
da Costa SS, Cruz OLM (1996) Exploratory tympanotomy. Oper Tech Otolaryngol Head Neck Surg 7(1):20–26
Martin C, Karkas A, Prades J (2017) Tubotympanic system functioning. Eur Ann Otorhinolaryngol Head Neck Dis 134(3):177–184. https://doi.org/10.1016/j.anorl.2017.03.010
Padurariu S, de Greef D, Jacobsen H, Kamavuako EN, Dirckx JJ, Gaihede M (2015) Pressure buffering by the tympanic membrane. In vivo measurements of middle ear pressure fluctuations during elevator motion. Hear Res. 340:113–120. https://doi.org/10.1016/j.heares.2015.12.004
Gaihede M, Padurariu S, Jacobsen H, De GD, Dirckx JJJ (2013) Eustachian tube pressure equilibration. Temporal analysis of pressure changes based on direct physiological recordings with an intact tympanic membrane. Hear Res. 301:53–59. https://doi.org/10.1016/j.heares.2013.01.003
Bluestone CD (2004) Studies in otitis media: Children’s Hospital of Pittsburgh-University of Pittsburgh Progress Report—2004. Laryngoscope. 114(11 III):1–26. https://doi.org/10.1097/01.mlg.0000148223.45374.ec
Mcdonald MH, Hoffman MR, Gentry LR, Jiang JJ (2012) New insights into mechanism of Eustachian tube ventilation based on cine computed tomography images. Eur Arch Oto-Rhino-Laryngol 269(8):1901–1907. https://doi.org/10.1007/s00405-011-1829-y
Berger GB (1989) Nature of spontaneous tympanic membrane perforation in acute otitis media in children. J Laryngol Otol 103(12):1150–1153. https://doi.org/10.1017/S0022215100111247
Rosito LPS, Canali I, Selaimen FA et al (2013) Análise descritiva dos achados otoscópicos em perfurações marginais da membrana timpânica. Braz J Otorhinolaryngol. 79(6 s1):2
Mansour S, Magnan J, Haidar H, Nicolas K (2015) Tympanic membrane retraction pocket. Springer, New York. https://doi.org/10.1007/978-3-319-13996-8
Paço J, Branco C, Estibeiro H (2009) The posterosuperior quadrant of the tympanic. Otolaryngol Head Neck Surg. 140(6):884–888. https://doi.org/10.1016/j.otohns.2009.01.009
Funding
None to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None to declare.
Ethics approval
The present study was performed in accordance with the ethical standards approved by the Research and Graduate Group of our institution (protocol #3.222.820).
Consent to participate
All patients signed a written informed consent form.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Selaimen, F.A., Rosito, L.P.S., da Silva, M.N.L. et al. Tympanic membrane perforations: a critical analysis of 1003 ears and proposal of a new classification based on pathogenesis. Eur Arch Otorhinolaryngol 279, 1277–1283 (2022). https://doi.org/10.1007/s00405-021-06776-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06776-8