Abstract
Purpose
To measure postoperative residual parotid volumes in parotidectomy patients and to measure the effect of residual parotid volumes on the symptom-specific quality of life (SSQOL) and complications.
Methods
Between January 2010 and December 2016, 148 parotid gland surgeries were performed, and 74 patients were included in the study. Bilateral parotid gland volumes were measured by Magnetic Resonance Imaging (MRI). Parotidectomy Outcome Inventory-8 and aesthetic scale questionnaire were applied to the patients. The volumetric averages obtained were compared with the questions in the SSQOL scale, the aesthetic scale data, and complications.
Results
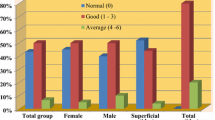
In the volumetric examination performed with MRI, the mean residual volumes of the operated parotid glands were 9.5 cm3, while the non-operated side was 28.8 cm3. The width of the surgery and the residual parotid tissue volume was inversely correlated. There was a statistically significant difference between the residual parotid gland volume and the pain related to the surgical area, depression in the surgical site, Frey's syndrome, incision scar, and numbness. As the residual parotid gland volumes decreased, the patients' cosmetic problems related to the surgical field increased significantly, and their SSQOL decreased.
Conclusion
Postoperative residual parotid tissue volume could be an objective parameter to measure patients' SSQOL and complications. After parotidectomy, the maximum amount of disease-free tissue of the parotid gland should be left in place to increase patients' quality of life and minimize complications.


Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
No applicable.
References
Ciuman RR, Oels W, Jaussi R, Dost P (2012) Outcome, general, and symptom-specific quality of life after various types of parotid resection. Laryngoscope 122(6):1254–1261. https://doi.org/10.1002/lary.23318
Beutner D, Wittekindt C, Dinh S, Huttenbrink KB, Guntinas-Lichius O (2006) Impact of lateral parotidectomy for benign tumors on quality of life. Acta Otolaryngol 126(10):1091–1095. https://doi.org/10.1080/00016480600606731
Nitzan D, Kronenberg J, Horowitz Z, Wolf M, Bedrin L, Chaushu G, Talmi YP (2004) Quality of life following parotidectomy for malignant and benign disease. Plast Reconstr Surg 114(5):1060–1067. https://doi.org/10.1097/01.prs.0000135326.50939.c1
Baumann I, Cerman Z, Sertel S, Skevas T, Klingmann C, Plinkert PK (2009) Development and validation of the Parotidectomy Outcome Inventory 8 (POI-8). Measurement of quality of life after parotidectomy in benign diseases. HNO 57(9):884–888. https://doi.org/10.1007/s00106-009-1991-3
Mehle ME, Kraus DH, Wood BG, Benninger MS, Eliachar I, Levine HL, Tucker HM, Lavertu P (1993) Facial nerve morbidity following parotid surgery for benign disease: the Cleveland Clinic Foundation experience. Laryngoscope 103(4):386–388
Marshall AH, Quraishi SM, Bradley PJ (2003) Patients’ perspectives on the short-and long-term outcomes following surgery for benign parotid neoplasms. J Laryngol Otol 117(8):624
Duman S (2010) Parotis neoplazilerinde postoperatif yaşam kalitesinin incelenmesi. Doctorate, Inonu University, Malatya
Upton DC, McNamar JP, Connor NP, Harari PM, Hartig GK (2007) Parotidectomy: ten-year review of 237 cases at a single institution. Otolaryngol Head Neck Surg 136(5):788–792
McGurk M, Renehan A, Gleave E, Hancock B (1996) Clinical significance of the tumour capsule in the treatment of parotid pleomorphic adenomas. Br J Surg 83(12):1747–1749
de Bree R, van der Waal I, Leemans CR (2007) Management of Frey syndrome. Head Neck 29(8):773–778. https://doi.org/10.1002/hed.20568
Rustemeyer J, Eufinger H, Bremerich A (2008) The incidence of Frey’s syndrome. J Cranio-Maxillofac Surg 36(1):34–37
Zhao H-W, Li L-J, Han B, Liu H, Pan J (2008) Preventing post-surgical complications by modification of parotidectomy. Int J Oral Maxillofac Surg 37(4):345–349
Minor V (1928) Ein neues Verfahren zu der klinischen Untersuchung der Schweissabsonderung. Dtsch Z Nervenheilkd 101(1):302–308
Linder TE, Huber A, Schmid S (1997) Frey’s syndrome after parotidectomy: a retrospective and prospective analysis. Laryngoscope 107(11):1496–1501
Koch M, Zenk J, Iro H (2010) Long-term results of morbidity after parotid gland surgery in benign disease. Laryngoscope 120(4):724–730
Brown J, Ord R (1989) Preserving the great auricular nerve in parotid surgery. Br J Oral Maxillofac Surg 27(6):459–466
Christensen N, Jacobsen S (1997) Parotidectomy. Preserving the posterior branch of the great auricular nerve. J Laryngol Otol 111(6):556–559
Yan F, Desiato VM, Nguyen SA, Lentsch EJ (2021) Impact of greater auricular nerve sacrifice during parotidectomy on quality of life. Head Neck 43(1):70–78. https://doi.org/10.1002/hed.26452
Min HJ, Lee HS, Lee YS, Jeong JH, Cho SH, Lee SH, Kim KR, Park CW, Tae K (2007) Is it necessary to preserve the posterior branch of the great auricular nerve in parotidectomy? Otolaryngol Head Neck Surg 137(4):636–641
Porter M, Wood S (1997) Preservation of the great auricular nerve during parotidectomy. Clin Otolaryngol Allied Sci 22(3):251–253
George M, Karkos PD, Dwivedi RC, Leong SC, Kim D, Repanos C (2014) Preservation of greater auricular nerve during parotidectomy: sensation, quality of life, and morbidity issues. A systematic review. Head Neck 36(4):603–608. https://doi.org/10.1002/hed.23292
de Oliveira FA, Duarte ECB, Taveira CT, Máximo AA, de Aquino EC, de Cássia AR, Vencio EF (2009) Salivary gland tumor: a review of 599 cases in a Brazilian population. Head Neck Pathol 3(4):271
Kaya BV, Kılıç C, Özlügedik S, Tuncel Ü, Cömert E (2016) Long-term effects of parotidectomy. Eur Arch Otorhinolaryngol 273(12):4579–4583
Chaushu G, Dori S, Sela B-A, Taicher S, Kronenberg J, Talmi YP (2001) Salivary flow dynamics after parotid surgery: a preliminary report. Otolaryngol Head Neck Surg 124(3):270–273
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Sukru Aydin and Mehmet Fatih Erbay. The first draft of the manuscript was written by Sukru Aydin and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Malatya Clinical Research Ethics Committee (2017/63).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This research was presented as a thesis at Inonu University Faculty of Medicine, Department of Otorhinolaryngology-Head and Neck Surgery, in 2019. Permission has been obtained from Dr. Baumann to use Parotidectomy Outcome Inventory-8.
Rights and permissions
About this article
Cite this article
Aydin, S., Erbay, M.F. & Kizilay, A. The effects of residual parotid volume on symptom-specific quality of life and complications in patients undergoing parotid surgery. Eur Arch Otorhinolaryngol 278, 5003–5011 (2021). https://doi.org/10.1007/s00405-021-06742-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06742-4