Abstract
Purpose
The margin status after CO2 laser cordectomy for glottic carcinoma may influence prognosis. There are no studies assessing the possible bias due to anatomic changes of the specimens for shrinkage. The authors evaluated the intraoperative shrinkage of specimens immediately after transoral CO2 laser microsurgery (CO2 TOLMS) to improve the understanding and the interpretation of surgical margins.
Methods
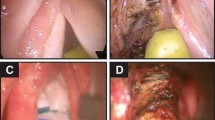
This is a prospective study involving a consecutive cohort of 23 patients (19 males, 4 females, mean age 69.9 years, range 42–83 years) with early glottic carcinoma treated by CO2 TOLMS from February 2017 to April 2019. The anteroposterior shrinkage of the specimen, of the tumor, and of the anterior and posterior margins was measured intraoperatively with a cross table reticle glass micrometer ruler, inserted into the eyepiece of the surgical microscope.
Results
The mean shrinkage of the mucosal specimen from intralaryngeal measurement to post-resection measurement was 3.8 ± 0.3 mm, resulting in an average loss of 29% of the anteroposterior length (p < 0.01). The anteroposterior length of both the tumor and the margins after resection significantly decreased, but the shrinkage of the anterior and posterior margins was significantly greater than the shrinkage of the tumor (49% versus 20% and 45% versus 20%, p < 0.01).
Conclusion
The present study demonstrates significant shrinkage of specimens after CO2 TOLMS, especially in the anteroposterior length of the vocal cords, and justifies the good oncological results for specimens with close and single positive superficial margins. Follow-up versus a second surgical look policy could be safely suggested in cases of close superficial and single positive superficial margins.


Similar content being viewed by others
References
Remacle M, Arens C, Eldin MB, Campos G, Estomba CC, Dulguerov P et al (2018) Correction to: Laser-assisted surgery of the upper aero-digestive tract: a clarification of nomenclature. A consensus statement of the European Laryngological Society. Eur Arch Otorhinolaryngol 275(2):657–658. doi: https://doi.org/10.1007/s00405-017-4851-x. (Erratum for: Eur Arch Otorhinolaryngol. 2017;274(10 ):3723–3727.)
Sjögren EV (2017) Transoral laser microsurgery in early glottic lesions. Curr Otorhinolaryngol Rep 5:56–68. https://doi.org/10.1007/s40136-017-0148-2
Carta F, Bandino F, Olla AM, Chuchueva N, Gerosa C, Puxeddu R (2018) Prognostic value of age, subglottic, and anterior commissure involvement for early glottic carcinoma treated with CO2 laser transoral microsurgery: a retrospective, single-center cohort study of 261 patients. Eur Arch Otorhinolaryngol 275:1199–1210. https://doi.org/10.1007/s00405-018-4890-y
Fiz I, Mazzola F, Fiz F, Marchi F, Filauro M, Paderno A, Parrinello G, Piazza C, Peretti G (2017) Impact of close and positive margins in transoral laser microsurgery for Tis-T2 glottic cancer. Front Oncol 7:245. https://doi.org/10.3389/fonc.2017.00245
Zhang SY, Lu ZM, Luo XN, Chen LS, Ge PJ, Song XH, Chen SH, Wu YL (2013) Retrospective analysis of prognostic factors in 205 patients with laryngeal squamous cell carcinoma who underwent surgical treatment. PLoS ONE 8:e60157. https://doi.org/10.1371/journal.pone.0060157
Charbonnier Q, Thisse AS, Sleghem L, Mouawad F, Chevalier D, Page C et al (2016) Oncologic outcomes of patients with positive margins after laser cordectomy for T1 and T2 glottic squamous cell carcinoma. Head Neck 38(12):1804–1809. https://doi.org/10.1002/hed.24518
Gallet P, Rumeau C, Nguyen DT, Teixeira PA, Baumann C, Toussaint B (2017) “Watchful observation” follow-up scheme after endoscopic CO2 laser treatment for small glottic carcinomas: a retrospective study of 93 cases. Clin Otolaryngol 42:1193–1199. https://doi.org/10.1111/coa.12863
Fiz I, Koelmel JC, Sittel C (2018) Nature and role of surgical margins in transoral laser microsurgery for early and intermediate glottic cancer. Curr Opin Otolaryngol Head Neck Surg 26:78–83. https://doi.org/10.1097/MOO.0000000000000446
Canis M, Ihler F, Martin A, Matthias C, Steiner W (2015) Transoral laser microsurgery for T1a glottic cancer: review of 404 cases. Head Neck 37:889–895. https://doi.org/10.1002/hed.23688
Jäckel MC, Ambrosch P, Martin A, Steiner W (2007) Impact of re-resection for inadequate margins on the prognosis of upper aerodigestive tract cancer treated by laser microsurgery. Laryngoscope 117:350–356. https://doi.org/10.1097/01.mlg.0000251165.48830.89
Hendriksma M, Montagne MW, Langeveld TPM, Veselic M, van Benthem PPG, Sjögren EV (2018) Evaluation of surgical margin status in patients with early glottic cancer (Tis-T2) treated with transoral CO2 laser microsurgery, on local control. Eur Arch Otorhinolaryngol 275:2333–2340. https://doi.org/10.1007/s00405-018-5070-9
Piazza C, Paderno A, Grazioli P, Del Bon F, Montalto N, Perotti P, Morello R, Filauro M, Nicolai P, Peretti G (2017) Laryngeal exposure and margin status in glottic cancer treated by transoral laser microsurgery. Laryngoscope 128:1146–1151. https://doi.org/10.1002/lary.26861
Mannelli G, Meccariello G, Deganello A, Maio V, Massi D, Gallo O (2014) Impact of low-thermal-injury devices on margin status in laryngeal cancer. An experimental ex vivo study. Oral Oncol 50:32–39. https://doi.org/10.1016/j.oraloncology.2013.10.001
AluffiValletti P, Taranto F, Chiesa A, Pia F, Valente G (2018) Impact of resection margin status on oncological outcomes after CO2 laser cordectomy. Acta Otorhinolaryngol Ital 38:24–30
Dauendorffer JN, Bastuji-Garin S, Guéro S, Brousse N, Fraitag S (2009) Shrinkage of skin excision specimens: formalin fixation is not the culprit. Br J Dermatol 160:810–814. https://doi.org/10.1111/j.1365-2133.2008.08994.x
Blasdale C, Charlton FG, Weatherhead SC, Ormond P, Lawrence CM (2010) Effect of tissue shrinkage on histological tumour-free margin after excision of basal cell carcinoma. Br J Dermatol 162:607–610. https://doi.org/10.1111/j.1365-2133.2009.09577.x
Sevray M, Brenaut E, Grangier Y, Misery L, Poizeau F, Staroz F (2020) Retraction of cutaneous specimens: tumours and margins after surgical excision. J Clin Pathol 73:42–46. https://doi.org/10.1136/jclinpath-2019-205988
Goldstein NS, Soman A, Sacksner J (1999) Disparate surgical margin lengths of colorectal resection specimens between in vivo and in vitro measurements: the effects of surgical resection and formalin fixation on organ shrinkage. Am J Clin Pathol 111:349–351. https://doi.org/10.1093/ajcp/111.3.349
Sondenaa K, Kjellevold KH (1990) A prospective study of the length of the distal margin after low anterior resection for rectal cancer. Int J Colorectal Dis 5:103–105. https://doi.org/10.1007/BF00298480
Siu KF, Cheung HC, Wong J (1986) Shrinkage of the esophagus after resection for carcinoma. Ann Surg 203:173–176. https://doi.org/10.1097/00000658-198602000-00011
Umstattd LA, Mills JC, Critchlow WA, Renner GJ, Zitsch RP (2017) Shrinkage in oral squamous cell carcinoma: an analysis of tumor and margin measurements in vivo, post-resection, and post-formalin fixation. Am J Otolaryngol 38:660–662. https://doi.org/10.1016/j.amjoto.2017.08.011
Egemen O, Bingöl D, Orman Ç, Sayilgan AT, Özkaya Ö, Akan M (2014) Quantification of the surgical margin shrinkage in lip cancer: determining the relation between the surgical and histopathologic margins. J Craniofacial Surg 25:2152–2155. https://doi.org/10.1097/SCS.0000000000001150
Johnson RE, Sigman JD, Funk GF, Robinson RA, Hoffman HT (1997) Quantification of surgical margin shrinkage in the oral cavity. Head Neck 19:281–286. https://doi.org/10.1002/(sici)1097-0347(199707)19:4%3c281::aid-hed6%3e3.0.co;2-x
Mistry RC, Qureshi SS, Kumaran C (2005) Post-resection mucosal margin shrinkage in oral cancer: quantification and significance. J Surg Oncol 91:131–133. https://doi.org/10.1002/jso.20285
Puxeddu R, Sionis S, Gerosa C, Carta F (2015) Enhanced contact endoscopy for the detection of neoangiogenesis in tumors of the larynx and hypopharynx. Laryngoscope 125:1600–1606. https://doi.org/10.1002/lary.25124
Remacle M, Eckel HE, Antonelli A, Brasnu D, Chevalier D, Friedrich G, Olofsson J, Rudert HH, Thumfart W, de Vincentiis M, Wustrow TP (2000) Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur Arch Otorhinolaryngol 257:227–231. https://doi.org/10.1007/s004050050228
Remacle M, van Haverbeke C, Eckel H, Bradley P, Chevalier D, Djukic V, de Vicentiis M, Friedrich G, Olofsson J, Peretti G, Quer M, Werner J (2007) Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies. Eur Arch Otorhinolaryngol 264:499–504. https://doi.org/10.1007/s00405-007-0279-z ((Erratum in: Remacle M, van Haverbeke C, Eckel H, Bradley P, Chevalier D, Djukic V, de Vicentiis M, Friedrich G, Olofsson J, Peretti G, Quer M, Werner J (2007) Eur Arch Otorhinolaryngol 264:709))
Lydiatt WM, Patel G, O’Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, Loomis AM, Shah JP (2017) Head and neck cancers-major changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin 67:122–137
Blanch JL, Vilaseca I, Bernal-Sprekelsen M, Grau JJ, Moragas M, Traserra-Coderch J, Caballero M, Sabater F, Guilemany JM, Alos L (2007) Prognostic significance of surgical margins in transoral CO2 laser microsurgery for T1–T4 pharyngo- laryngeal cancers. Eur Arch Otorhinolaryngol 264:1045–1051. https://doi.org/10.1007/s00405-007-0320-2
Peretti G, Piazza C, Cocco D, de Benedetto L, del Bon F, de Zinis RLO, Nicolai P (2010) Transoral CO2 laser treatment for Tis-T3 glottic cancer: the University of Brescia experience on 595 patients. Head Neck 32:977–983. https://doi.org/10.1002/hed.21278
Karatzanis AD, Waldfahrer F, Psychogios G, Hornung J, Zenk J, Velegrakis GA, Iro H (2010) Resection margins and other prognostic factors regarding surgically treated glottic carcinomas. J Surg Oncol 101:131–136. https://doi.org/10.1002/jso.21449
Galli A, Giordano L, Sarandria D, Di Santo D, Bussi M (2016) Oncological and complication assessment of CO2 laser-assisted endoscopic surgery for T1–T2 glottic tumours: clinical experience. Acta Otorhinolaryngol Ital 36:167–173
Bertolin A, Lionello M, Salis G, Rizzotto G, Lucioni M (2017) Two-stage CO2 -laser-assisted bilateral cordectomy for cT1b glottic carcinoma. Am J Otolaryngol 38:183–187. https://doi.org/10.1016/j.amjoto.2017.01.004
Hoffmann C, Cornu N, Hans S, Sadoughi B, Badoual C, Brasnu D (2016) Early glottic cancer involving the anterior commissure treated by transoral laser cordectomy. Laryngoscope 126:1817–1822. https://doi.org/10.1002/lary.25757
Hartl DM, de Monès E, Hans S, Janot F, Brasnu D (2007) Treatment of early-stage glottic cancer by transoral laser resection. Ann Otol Rhinol Laryngol 116:832–836. https://doi.org/10.1177/000348940711601107
Brøndbo K, Fridrich K, Boysen M (2007) Laser surgery of T1a glottic carcinomas; significance of resection margins. Eur Arch Otorhinolaryngol 264:627–630. https://doi.org/10.1007/s00405-006-0233-5
Remacle M, Lawson G, Nollevaux M-C, Delos M (2008) Current state of scanning micromanipulator applications with the carbon dioxide laser. Ann Otol Rhinol Laryngol 117:239–244. https://doi.org/10.1177/000348940811700401
Zhang Z (2019) Structural constitutive modeling of the anisotropic mechanical properties of human vocal fold lamina propria. J Acoust Soc Am 145:EL476. https://doi.org/https://doi.org/10.1121/1.5109794
Rohlfs A-K, Goodyer E, Clauditz T, Hess M, Kob M, Koops S, Püschel K, Roemer FW, Müller F (2013) The anisotropic nature of the human vocal fold: an ex vivo study. Eur Arch Otorhinolaryngol 270:1885–1895. https://doi.org/10.1007/s00405-013-2428-x
Kelleher JE, Siegmund T, Du M, Naseri E, Chan RW (2013) Empirical measurements of biomechanical anisotropy of the human vocal fold lamina propria. Biomech Model Mechanobiol 12:555–567. https://doi.org/10.1007/s10237-012-0425-4
Puxeddu R, Piazza C, Mensi MC, Ledda GP, Argiolas F, Peretti G (2004) Carbon dioxide laser salvage surgery after radiotherapy failure in T1 and T2 glottic carcinoma. Otolaryngol Head Neck Surg 130(1):84–88. https://doi.org/10.1016/j.otohns.2003.07.002
Winter JCF (2013) Using the student’s t-test with extremely small sample sizes. Pract Assessment, Res Eval 18(10):1–12. https://doi.org/10.7275/e4r6-dj05
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mariani, C., Carta, F., Tatti, M. et al. Shrinkage of specimens after CO2 laser cordectomy: an objective intraoperative evaluation. Eur Arch Otorhinolaryngol 278, 1515–1521 (2021). https://doi.org/10.1007/s00405-021-06625-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06625-8