Abstract
Objective
The possible etiological relationship of the vitamin D with laryngomalacia is unclear. The aim of the study was to demonstrate the relationship between laryngomalacia and vitamin D levels.
Methods
Twenty-three non-syndromic babies under the age of 1 year who were diagnosed with laryngomalacia were included in the study group. Forty healthy babies were included in the control group. The detailed anamnesis was obtained and a complete systemic physical examination, a flexible endoscopic laryngeal examination, and laboratory tests [calcium (Ca), phosphorus (P), alkaline phosphatase (ALP), parathormone (PTH), alanine transaminase (ALT), aspartate transaminase (AST), blood urea nitrogen (BUN), creatinine (Cre), and 25-hydroxy vitamin D (25-OH D)] were performed in all patients. All laboratory tests of the groups were compared.
Results
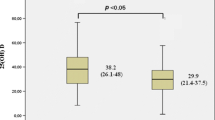
It was observed that there was no significant difference in the parameters that could affect vitamin D levels, namely type of feeding, vitamin D supplement intake, and the season when the serum sample was taken (p > 0.05). The vitamin D level was significantly lower (p = 0.003, p < 0.05) and the P and ALP levels were significantly higher (p = 0.016 and p = 0.001, respectively; p < 0.05) in the laryngomalacia group. Although the correlation between vitamin D and PTH was not statistically significant according to the Pearson correlation analysis, it was lower in the laryngomalacia group compared to the control group (p = 0.381, p > 0.05).
Conclusion
In this study, it was observed that the vitamin D levels were lower in infants with laryngomalacia compared to the control group. We consider that vitamin D deficiency may be a factor in the etiology of laryngomalacia with a yet-to-be-clarified etiology.

Similar content being viewed by others
References
Landry AM, Thompson DM (2012) Laryngomalacia: disease presentation, spectrum and management. Int J Pediatr 2012:753526. https://doi.org/10.1155/2012/753526
Ayari S, Aubertin G, Girschig H, Van Den Abbeele T, Mondain M (2012) Pathophysiology and diagnostic approach to laryngomalacia in infants. Eur Ann Otorhinolaryngol Head Neck Dis 129:257–263
Hassan MM, Emam AM, Mahmoud AM et al (2020) Congenital laryngomalacia: Is it an inflammatory disease? The role of vitamin D. Laryngoscope 130(2):448–453
Isaac A, Zhang H, Soon SR, Campbell S, El-Hakim H (2016) A systematic review of the evidence on spontaneous resolution of laryngomalacia and its symptoms. Int J Pediatr Otorhinolaryngol 83:78–83
Rathi A, Rathi S (2017) Relative imbalance as etiology of laryngomalacia—a new theory. Med Hypotheses 98:38–41. https://doi.org/10.1016/j.mehy.2016.11.004
Munson PD, Saad AG, El-Jamal SM, Dai Y, Bower CM, Richter GT (2011) Submucosal nerve hypertrophy in congenital laryngomalacia. Laryngoscope 121:627–629
Thompson DM (2007) Abnormal sensorimotor integrative function of the larynx in congenital laryngomalacia: a new theory of etiology. Laryngoscope 117(6 pt 2 suppl 114):1–33
Francesca D, Fulvio L, Juergen B et al (2014) Relationship between vitamin D and inflammatory markers in older individuals. Age (Dordr) 36:9694
Cashman KD, Dowling KG, Škrabáková Z et al (2016) Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr 103:1033–1044
Gholami F, Moradi G, Zareei B et al (2019) The association between circulating 25 hydroxyvitamin D and cardiovascular diseases: a meta-analysis of prospective cohort studies. BMC Cardiovasc Disord 19(1):248. https://doi.org/10.1186/s12872-019-1236-7
Sharawat IK, Dawman L (2019) Bone mineral density and its correlation with vitamin D status in healthy school-going children of Western India. Arch Osteoporos 14(1):13. https://doi.org/10.1007/s11657-019-0568-3
Antonucci R, Locci C, Clemente MG, Chicconi E, Antonucci L (2018) Vitamin D deficiency in childhood: old lessons and current challenges. J Pediatr Endocrinol Metab 31(3):247–260. https://doi.org/10.1515/jpem-2017-0391
Halterman JS, Smith SA (1998) Hypocalcemia and stridor: an unusual presentation of vitamin D-deficient rickets. J Emerg Med 16(1):41–43
- Sharma D, Pandita A, Pratap OT, Murki S (2014) Laryngospasm and neonatal seizure due to hypocalcaemia and vitamin D deficiency: an emergency condition in NICU and challenge to the neonatologist. Case Rep. 2014:bcr2014206795
Bassiouni H, Aly H, Zaky K, Abaza N, Bardin T (2015) Probing the relation between vitamin D deficiency and progression of medial femoro-tibial osteoarthitis of the knee. Ann Rheum Dis 74:368–369
Mabey T, Honsawek S (2015) Role of vitamin D in osteoarthritis: molecular, cellular, and clinical perspectives. Int J Endocrinol 2015:383918
Holick MF, Binkley NC, Bischoff-Ferrari HA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 96:1911–1930
Lane NE (2009) Metabolic bone disease. In: Firestein GS, Budd RC, Harris ED, Mclnnes IB, Ruddy S, Sergent JS (eds) Textbook of rheumatology Kelley’s. Saunders Elsevier, pp 1579–1599
Holick MF, Garabedian M (2006) Vitamin D photobiology, metabolism, mechanism of action and clinical application. In: Favus MJ (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism, 6th edn. American Society for Bone and Mineral Research, Washington, DC, pp 106–114
Hatun S, Ozkan B, Orbak Z et al (2005) Vitamin D deficiency in early infancy. J Nutr 135:279–282
Alon US (2011) Clinical practice. Fibroblast growth factor (FGF)23: a new hormone. Eur J Pediatr 170(5):545–554
Gattineni J, Bates C, Twombley K et al (2009) FGF23 decreases renal NaPi-2a and NaPi-2c expression and induces hypophosphatemia in vivo predominantly via FGF receptor 1. Am J Physiol Renal Physiol 297(2):F282–F291
Harding JE, Wilson J, Brown J (2017) Calcium and phosphorus supplementation of human milk for preterm infants. Cochrane Database Syst Rev 2:CD003310
Wan H, Zhu J, Su G et al (2016) Dietary supplementation with beta-hydroxy-beta-methylbutyrate calcium during the early postnatal period accelerates skeletal muscle fibre growth and maturity in intra-uterine growth-retarded and normal-birth-weight piglets. Br J Nutr 115(8):1360–1369
Turan S, Topcu B, Gökçe İ et al (2011) Serum alkaline phosphatase levels in healthy children and evaluation of alkaline phosphatase z-scores in different types of rickets. J Clin Res Pediatr Endocrinol 3(1):7–11. https://doi.org/10.4274/jcrpe.v3i1.02
Sharma U, Pal D, Prasad R (2014) Alkaline phosphatase: an overview. Indian J Clin Biochem 29(3):269–278. https://doi.org/10.1007/s12291-013-0408-y
Schipani E, Provot S (2003) PTHrP, PTH, and the PTH/PTHrP receptor in endochondral bone development. Birth Defects Res Part C Embryo Today Rev 69(4):352–362. https://doi.org/10.1002/bdrc.10028
Krishnan Y, Grodzinsky AJ (2018) Cartilage diseases. Matrix Biol 71–72:51–69. https://doi.org/10.1016/j.matbio.2018.05.005
Jin X, Jones G, Cicuttini F et al (2016) Effect of vitamin D supplementation on tibial cartilage volume and knee pain among patients with symptomatic knee osteoarthritis: a randomized clinical trial. JAMA 315:1005–1013
Veronese N, Maggi S, Noale M et al (2015) Serum 25-hydroxyvitamin D and osteoarthritis in older people: the Progetto Veneto Anziani study. Rejuvenation Res 18:543–553
Hollis BW, Wagner CL (2013) Vitamin D and pregnancy: skeletal effects, nonskeletal effects, and birth outcomes. Calcif Tissue Int 92:128–139
Hossein-nezhad A, Holick MF (2013) Vitamin D for health: a global perspective. Mayo Clin Proc 88:720–755
Yeşiltepe GM, Hatun S (2011) Perinatal D vitamini yetersizliği. Çocuk Sağlığı ve Hastalıkları Dergisi 54:87–98
Funding
The work received no external financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bozkurt, H.B., Çelik, M. Investigation of the serum vitamin D level in infants followed up with the diagnosis of laryngomalacia: a case–control study. Eur Arch Otorhinolaryngol 278, 733–739 (2021). https://doi.org/10.1007/s00405-020-06412-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06412-x