Abstract
Purpose
Competent otoscopy is a key otolaryngology skill for a broad range of medical careers, yet undergraduate’s confidence to perform otoscopy is reported as low. Smartphone otoscopes have been suggested to improve undergraduates learning of normal eardrum anatomy because unlike the traditional otoscope, the learner and educator share the same image. This study aimed to evaluate whether a smartphone otoscope could enhance medical undergraduates recognition of common ear pathology.
Methods
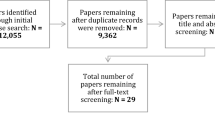
52 medical students were randomised into a standard group that used a traditional otoscope and an intervention group that used a smartphone otoscope. Both groups received a short didactic presentation on the recognition of common ear pathologies and were asked to diagnose four simulated pathologies. Both groups received feedback and guidance on how to better visualise the tympanic membrane. Force response items and 5-point Likert scales loaded on an electronic platform recorded their diagnosis and their perceptions towards the otoscope.
Results
The smartphone-group (n = 20) had higher overall rates of correct diagnosis compared to control (n = 22) (84% vs. 39%, p = < 0.001). Only the grommet station did not show a significant improvement between the two groups (100% vs. 91%, p = 0.49). 90% (n = 20) of participants felt the smartphone otoscope was preferential for their learning. The same number expressed that they want to use it in future learning. The remainder were indifferent.
Conclusions
The smartphone otoscope enabled learners to better observe and recognise middle ear pathology. This popular learning tool has the potential to accelerate the learning curve of otoscopy and therefore improve the proficiency of future doctors at recognising middle ear diseases.




Similar content being viewed by others
References
UK Foundation Programme Office (UKFPO). UK F2 Career destinations report (Internet). 2018 (cited 2020 Jul 3). Available from: https://www.foundationprogramme.nhs.uk/wp-content/uploads/sites/2/2019/11/F2-Career-Destinations-Report_FINAL-2018.pdf. Accessed 03 July 2020
General Medical Council (2011) General Medical Council Education Strategy.
General Medical Council. Practical skills and procedures. Outcome for graduates (Internet). 2018 (cited 2020 Jul 3). Available from: https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates/practical-skills-and-procedures. Accessed 07 Mar 2020
Lund VJ (1990) Otolaryngology in the curriculum–10 years on: discussion paper. J R Soc Med 83(6):377–379
Khan MM, Saeed SR (2012) Provision of undergraduate otorhinolaryngology teaching within general medical council approved UK medical schools: what is current practice? J Laryngol Otol 126(04):340–344
Powell J, Cooles FAH, Carrie S, Paleri V (2011) Is undergraduate medical education working for ENT surgery? A survey of UK medical school graduates. J Laryngol Otol 125(09):896–905
Ferguson GR, Bacila IA, Swamy M (2016) Does current provision of undergraduate education prepare UK medical students in ENT? A systematic literature review. BMJ Open 6(4):e010054
Clamp PJ, Gunasekaran S, Pothier DD, Saunders MW (2007) ENT in general practice: training, experience and referral rates. J Laryngol Otol 121:06
Easto RH, Reddy V (2016) A survey of ENT experience in South West Peninsula general practitioner trainees: how can post-graduate ENT training be improved? J Laryngol Otol 130(10):893–896
Hakimi AA, Lalehzarian AS, Lalehzarian SP, Azhdam AM, Nedjat-Haiem S, Boodaie BD (2019) Utility of a smartphone-enabled otoscope in the instruction of otoscopy and middle ear anatomy. Eur Arch Otorhinolaryngol 276(10):2953–2956
Schuster-Bruce J, Davies A, Conchie H, Shamil E, Waddell A (2020) A letter in response to the article entitled ‘Utility of a smartphone‐enabled otoscope in the instruction of otoscopy and middle ear anatomy.’ Eur Arch Otorhinolaryngol. Available from: https://link.springer.com/10.1007/s00405-019-05775-0. Accessed 04 Mar 2020
Mandavia R, Lapa T, Smith M, Bhutta MF (2016) A cross-sectional evaluation of the validity of a smartphone otoscopy device in screening for ear disease in Nepal. Clin Otolaryngol 43(1):31–38
Lloyd S (2014) Undergraduate Curriculum| SFO UK (Internet). Sfo.entuk.org. (cited 23 November 2017). Available from: https://sfo.entuk.org/services/undergraduate-curriculum. Accessed 2 Mar 2018
TYMPA Health (2016) Available at: https://www.tympahealth.com/the-tympa-system/. Accessed 1 April 2020
Soares C, Clifton W, Freeman WD. Use of Handheld Video Otoscopy for the diagnosis of acute otitis media: technical note. Cureus (Internet). 2019 Sep 1; Available from: https://www.cureus.com/articles/22776-use-of-handheld-video-otoscopy-for-the-diagnosis-of-acute-otitis-media-technical-note. Accessed 28 Dec 2019
Niermeyer WL, Philips RHW, Essig GF, Moberly AC (2019) Diagnostic accuracy and confidence for otoscopy: Are medical students receiving sufficient training?: Otoscopic accuracy and confidence. Laryngoscope 129(8):1891–1897
You P, Chahine S, Husein M (2017) Improving learning and confidence through small group, structured otoscopy teaching: a prospective interventional study. J of Otolaryngol Head Neck Surg 46(1):68
Lee DJ, Fu TS, Carrillo B, Campisi P, Forte V, Chiodo A (2015) Evaluation of an otoscopy simulator to teach otoscopy and normative anatomy to first year medical students. Laryngoscope 125(9):2159–2162
Wickens B, Lewis J, Morris DP, Husein M, Ladak HM, Agrawal SK (2015) Face and content validity of a novel, web-based otoscopy simulator for medical education. J of Otolaryngol Head Neck Surg 44(1):7
Livingstone D, Talai AS, Chau J, Forkert ND (2019) Building an Otoscopic screening prototype tool using deep learning. J of Otolaryngol Head Neck Surg 48(1):66
Livingstone D, Chau J (2019) Otoscopic diagnosis using computer vision: an automated machine learning approach. Laryngoscope 2:82–92
Demant MN, Jensen RG, Bhutta MF, Laier GH, Lous J, Homøe P (2019) Smartphone otoscopy by non-specialist health workers in rural Greenland: a cross-sectional study. Int J Pediatr Otorhinolaryngol 126:109628
Shah MU, Sohal M, Valdez TA, Grindle CR (2018) iPhone otoscopes: currently available, but reliable for tele-otoscopy in the hands of parents? Int J Pediatr Otorhinolaryngol 106:59–63
Acknowledgements
The authors would like to acknowledge Mr Krishan Ramdoo of Tympahealth for donating the TympaSystems that were used in this study.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JSB had previously received monies from TYMPAhealth in remuneration for the organisation and delivery of a user training session. He does not own any shares and does not have any ongoing financial relationship. JRS works at TYMPA with a share option at the discretion of the companies’ board. JRS performed the statistical tests but did not have a role in the design, execution, or interpretation of the data. All other authors have no conflicts of interest in connection with this article or affiliation with TympaHealth, and have not received any financial remuneration or incentives. TympaHealth were not involved in the design or manuscript, except for statistical analysis, which was corroborated by remaining authors for accuracy. Data and statistical analysis were available.
Ethical approval
St George’s University ethics board granted ethical approval for the intervention. Written consent was sought from students prior to participation.
Location of study
St Georges University of London.
Availability of data and materials
Data can be made available on request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schuster-Bruce, J.R., Ali, A., Van, M. et al. A randomised trial to assess the educational benefit of a smartphone otoscope in undergraduate medical training. Eur Arch Otorhinolaryngol 278, 1799–1804 (2021). https://doi.org/10.1007/s00405-020-06373-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06373-1